PBL #2 Case 1 A 57 year old female complains of right
advertisement
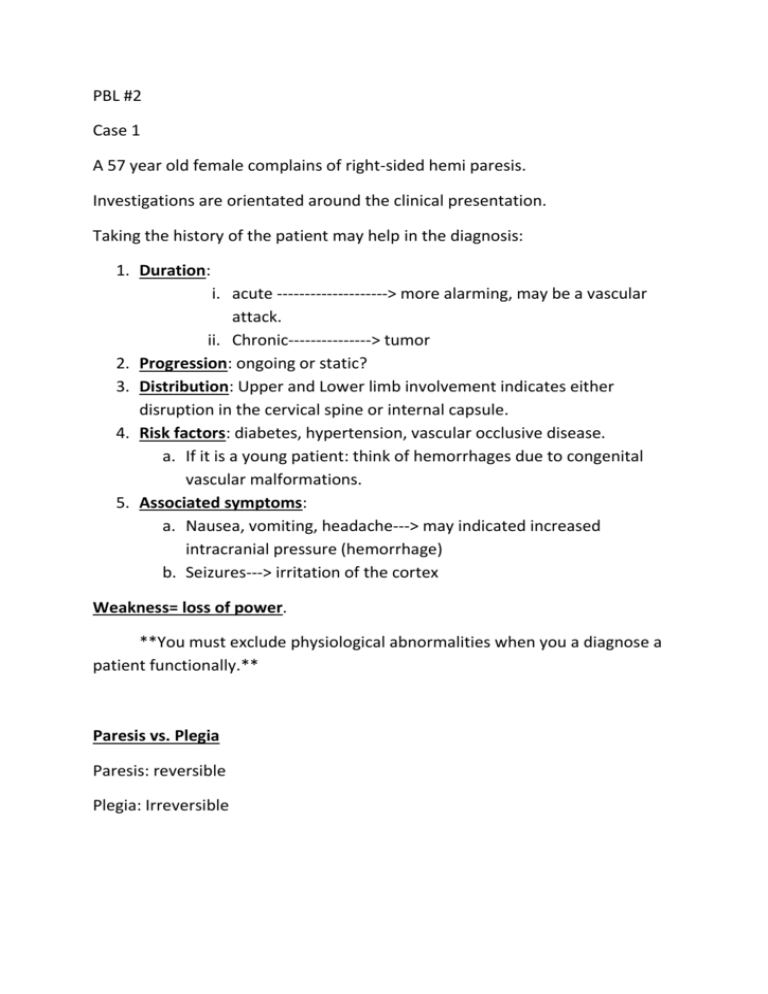
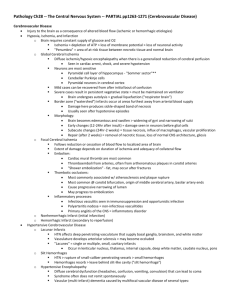
PBL #2 Case 1 A 57 year old female complains of right-sided hemi paresis. Investigations are orientated around the clinical presentation. Taking the history of the patient may help in the diagnosis: 1. Duration: 2. 3. 4. 5. i. acute --------------------> more alarming, may be a vascular attack. ii. Chronic---------------> tumor Progression: ongoing or static? Distribution: Upper and Lower limb involvement indicates either disruption in the cervical spine or internal capsule. Risk factors: diabetes, hypertension, vascular occlusive disease. a. If it is a young patient: think of hemorrhages due to congenital vascular malformations. Associated symptoms: a. Nausea, vomiting, headache---> may indicated increased intracranial pressure (hemorrhage) b. Seizures---> irritation of the cortex Weakness= loss of power. **You must exclude physiological abnormalities when you a diagnose a patient functionally.** Paresis vs. Plegia Paresis: reversible Plegia: Irreversible An infarction is a region of hypodensity on a CT scan. It will NOT show until after 6 hours of an attack. Thus, early ischemic changes should be recorded by a diffuse scan. -Hemorrhage: seen as a large white mass -Tumor: is a non-vascular, chronic space-occupying lesion. -If the patient is middle-aged, think of ANEURYSM -If the patient is elderly, think of ISCHEMIA or HEMORRHAGE. -Systemic diseases will cause both brain and limb ischemia Diabetes will cause SMALL VESSEL DISEASE, which may lead to strokes. Lab tests are used to rule out systemic diseases. *** Acute intervention--------> Catheterization (first 3-6 hours) 1. To ensure rapid recovery of the neurons 2. Given with anticoagulants Rehabilitation is needed for CHRONIC MANAGEMENT.