Physiology and Psychology of Pregnancy
advertisement

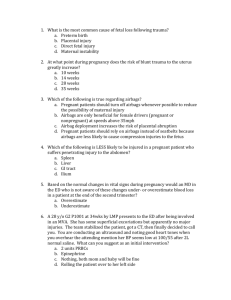
Physiology & Psychology • Maternal physiological adaptations to pregnancy • The placenta • Psychosocial adaptations Physiology of Pregnancy Goals: 1) Healthy mother 2) Appropriately grown, healthy fetus with low risk for adult disease Systematic Adjustments to Pregnancy • • • • Cardiovascular Respiratory Renal GI Cardiovascular Adaptations • Heart rate increases – 10-20% – Begins as early as 5 weeks – Peaks by 32 weeks • Stoke volume increases – 25-30% – Peeks at 16-24 weeks • Systemic Vascular Resistance decreases – – – – 20% As early as 5 weeks Result of vascular smooth muscle relaxation Allows changes in cardiac output without increase in arterial pressure Cardiac output during three stages of gestation, labor, and immediately postpartum compared with values of nonpregnant women. All values were determined with women in the lateral recumbent position. Respiratory Adaptations • 30% increased production of CO2 • 50% increase volume air and gas exchange • Increase in lung volume • Decreased airway resistance Renal Function Changes • Renal blood flow – Increases 50-80% by end of 1st trimester – Decreases gradually to term • Glomerular filtration rate – Increases 40-50% – Begins at 5 weeks, peaks at 9-16 weeks – May decrease 15-20% from 36 weeks to term Mean glomerular filtration rate in healthy women over a short period with infused inulin (solid line), simultaneously as creatinine clearance during the inulin infusion (broken line), and over 24 hours as endogenous creatinine clearance (dotted line). GI Adaptations • Anatomic – growing uterus • Hormonal – Progesterone – relaxation of GI smooth muscle – Estrogen – increased tissue vascularity Adjustments in Nutrient Metabolism • Goals – support changes in anatomy and physiology of mother – support fetal growth and development – maintain maternal homeostasis – prepare for lactation • Adjustments are complex and evolve throughout pregnancy General Concepts 1. Alterations include: • increased intestinal absorption • reduced excretion by kidney or GI tract 2. Alterations are driven by: • hormonal changes • fetal demands • maternal nutrient supply 3. There may be more than one adjustment for each nutrient. 4. Maternal behavioral changes augment physiologic adjustments. 5. When adjustment limits are exceeded, fetal growth and development are impaired. Birth weight of 11 children born to a poor woman in Montreal; 8 children were born before receiving nutritional counseling and food supplements from the Montreal Diet Dispensary and 3 children were born afterward. 6. The first half of pregnancy is a time of preparation for the demands of rapid fetal growth in the second half. 7. Alterations in maternal physiology facilitate transfer of nutrients to the fetus. Nitrogen Balance (g/day) Source Early pregnant Late pregnant Nonpregnant Intake 12.03 12.19 11.88 Fecal loss -0.82 -0.92 -0.64 Urinary loss -10.52 -9.02 -10.56 Integumental loss -0.14 -0.18 -0.21 0.56 2.10 0.46 Retention Hormonal Adjustments • Changes in over 30 different hormones have been detected in pregnancy • Estrogens: increase significantly in pregnancy, influence carbohydrate, lipid, and bone metabolism • Progesterone: relaxes smooth muscle and causes atony of GI and urinary tract • Human Placental Lactogen (hPL): stimulates maternal metabolism, increases insulin resistance, aids glucose transport across placenta, stimulates breast development Late gestation is characterized by: – Anti-insulinogenic and lipolytic effects of Human chorionic somatomammotropin, prolactin, cortisol, glucagon Which Results in: – Glucose intolerance, insulin resistance, decreased hepatic glycogen, mobilization of adipose tissue Maternal Nutrient Levels • Increased triglycerides • Increased cholesterol • Decreased plasma amino acids & albumin Lipids Total triglycerides Total cholesterol VLDL cholesterol Non pregnant 60 170 10 Early Late pregnancy pregnancy 75 to 100 210 175 to 200 250 10 25 LDL cholesterol 105 100 to 125 150 HDL cholesterol 55 55 to 75 65 Maternal Albumin Week of Gestation 10 20 30 40 Serum Albumin g/L 32 29 28 28 Maternal Plasma volume increases ~ 40% • range 30-50% • nutrient concentration declines due to increased volume, but total amount of vitamins and minerals in circulation actually increases. Mean hemoglobin concentrations ( — ) and 5th and 95th ( — percentiles for healthy pregnant women taking iron supplements ) Embryonic and Placental Development • http://www.youtube.com/watch?v=UgT5rU Q9EmQ • http://www.youtube.com/watch?v=jo3NjAp FSQE • http://www.youtube.com/watch?v=YJL9roi 1LbM&feature=related Embryonic Development • In early gestation Embryo is nourished by secretions of the oviduct and uterine endometrial glands • Uterine secretions include growth factors (e.g. TNFa, epidermal growth factor) that promote placental growth • Growth trajectories of both placenta and fetus are established early & have lifelong consequences Nutrient Availability & Maternal Metabolic Status • Blastocyst development & implantation are reduced – diabetic mothers – animal models with insufficient nutrients • Poorly nourished women and obese women at risk for aberrations in embryonic and placental development – Congenital anomalies – Adverse outcomes later in pregnancy (e.g. preeclampsia) The Placenta • 10-12 weeks is the period of placentation • Rapid early growth prepares way for fetal growth • Trophoblast cells use same molecular mechanisms as tumors, but are highly regulated and controlled Placental Functions • Maintains immunological distance between mother and fetus • Special endocrine organ: “transient hypothalamo-pituitary-gonadal axis” • Responsible for exchange of nutrients, gases & metabolic waste products between maternal and fetal circulation Placental Architecture • Maternal and fetal blood do not mix: “placental barrier” – Fetal blood flows through capillary networks within highly branched terminal chorionic villi – Maternal blood flows through intervillous space • Uterine arteriols bring blood in • Uterine venules drain blood Placental vasculature Reproduced with permission from: Vander, AJ, Sherman, JH, Luciano, DS. Human Physiology, 6th ed, McGraw-Hill, Inc 2001. p. 679. Original Figure . 19-24. Copyright © 2001 McGraw-Hill ©2007 UpToDate® • www.uptodate.com Licensed to Univ Of Washington Placental Capacity Increases During Gestation • Expression of transporters increases • The “brush border” microvilli develop to: – increase surface area – impede maternal blood flow • Flow through the placenta at term is 500 ml/minute Mechanisms of Nutrient Transfer Across the Placenta Maternal to Infant Nutrient Transportation Across The Placenta Substance Primary Mechanism Water, electrolytes, urea, free fatty Passive diffusion acids, steroids, fat soluble vitamins Glucose Facilitated diffusion Amino acids, water soluble vitamins, calcium, iron, iodine Active transport Globulins, phospholipids, lipoproteins Pinocytosis and endocytosis Water, electrolytes Bulk flow (due to changes in hydrostatic or osmotic forces), solvent drag Fetal to Maternal Transport • Carbon dioxide • Water & urea • Signaling Molecules: Hormones, cytokines, others Factors Affecting Placental Transfer • Placental size • Diffusion distance – – diabetes and infection cause edema of the villi – distance decreases as pregnancy progresses and fetal needs increase • Maternal-placental blood flow • Blood saturation with gases and nutrients Factors Affecting Placental Transfer (cont) • Maternal-placental metabolism of the substance • Disorders in expression or activity of nutrient transporters • Maternal use of tobacco, cocaine, alcohol Metabolic Functions of the Placenta • Glycogen synthesis: from maternal glucose & stored • Cholesterol synthesis: placental cholesterol is precursor for placental progesterone and estrogens • Protein production: rises to 7.5 g per day at term • Lactate: produced in large quantities and needs to be removed Endocrine Functions • Placenta Produces Peptide hormones – Human Chorionic gonodotrophin (hCG) - secreted early and helps to maintain synthesis of progesterone – Human placental lactogen (hPL): increase supply of glucose to future by decreasing maternal stores of fatty acids by altering maternal secretion of insulin – Insulin-like growth factors (IGF): IGF signaling system is a major regulator of growth in fetus and infant Endocrine Functions • Steroid hormones – Progesterone: produced by placenta, needed to maintain non-contractile uterus – Estrogen: produced by placenta drives many processes in pregnancy • Glucocorticoids: placenta regulates fetal exposure Emerging Understandings • Cytokines & Inflammatory molecules are produced by the placenta as well as adipocytes • Adverse outcomes in obese women may be associated with imbalances due to overproduction from both sources • “In pregnancy complicated with obesity or DM, continuous adverse stimulus is associated with dysregulation of metabolic, vasular and inflammatory pathways.” The Known and Unknown of Leptin in Pregnancy (Hauguel-de-Mouzon, Am J Obstet Gynecology, 2006) • Maternal plasma leptin levels rise in pregnancy • Leptin is produced by placenta • Overproduction of placental leptin is seen with diabetes and htn in pregnancy • Umbilical leptin levels are biomarker of fetal adiposity • “Leptin may be sensitive to maternal energy status and coordinate metabolic response accordingly.” (King, Ann Rev Nutr, 2006) Maternal Undernutrition Influences Placental-Fetal Development (Belkacemi et al. Bio Repro. 2010) • What nutritional factors are associated with placental “plasticity?” • What are the long term impacts of placental insufficiency? • What are the implications for practice? Psychology of Pregnancy • Psychosocial adaptation – Process over time – Prerequisite for developing parental identify and behavior • Factors that impact psychosocial adaptation – Pregnancy intendedness – Stress & depression Why do we care in terms of nutrition? • Stress interferes with ability to achieve developmental tasks • Developmental tasks key to ability of mother to take care of herself and her baby nutritionally. Maternal Focus Trimester 1 I’m pregnant! 2 There’s a BABY….. 3 I’m going to be a MOM Developmental Tasks of Pregnancy (Rubin, 1984) • Seeking safe passage for herself and her child through pregnancy, labor, and delivery. • Ensuring the acceptance by significant persons in her family of the child she bears. • Binding-in to her unknown baby. • Learning to give of herself. Ensuring Safe Passage • Care and knowledge seeking behaviors • Concerns – T1: own well-being – T2: focus shifts to fetus/baby – T3: surviving labor and birth • Goal: personal survival and safe birth of healthy baby Seeking Acceptance/Support for Self and Baby • Re-defining relationships with – Spouse/partner – Family of origin – Friends – New social support networks • Goal: ensure a place in the world for herself, as a woman with a child, and her baby “Binding-in” to Unborn Child • Attachment to fetus • Process: – Begins in childhood – Intensifies in pregnancy with fantasizing about unborn infant – Well developed relationship by T3 – Birth – let go of being pregnant & adjusts to being mother – Integrates real baby • Goal: maternal identity development Giving of Oneself • Willingness & ability to make personal sacrifices for well-being of fetus/infant • Goal: insure baby’s future well-being What about Dad? Psychosocial and mental health issues for new fathers. (Condon, 2006. The Australian First Time Fathers Study) Tasks: 1. Developing an attachment to the fetus 2. Adjusting to the dyad becoming a triad 3. Conceptualizing the self as “father” 4. What type of father? Unintended Pregnancy At the time you became pregnant, did you want to become pregnant then, did you want to wait until later, or did you want no (more) children at all? Births from Unintended Pregnancy in WA State (PRAMS) 2000 2007 2010 Medicaid 56 54 51 Non-Medicaid 26 22 23 Total 38 36 36 http://www.doh.wa.gov/Portals/1/Documents/Pubs/950153_PerinatalIndicatorsforWashingtonResidents.pdf, May 2012 Unintended Pregnancy Effects of pregnancy planning status on birth outcomes and infant care (Kost et al. Family Planning Perspectives, 1998) Intended Mistimed Unwanted LBW 5.1 6.5 9.7 SGA 9.5 11.3 13.7 Any negative outcomes 15.6 20.4 25.5 Ever breastfed 59.9 46.6 36.1 Prevalence of Self-Reported Postpartum Depressive Symptoms. MMWR, April 2008 • Overall prevalence ranged from 12-20% in states. • Characteristics associated with PDS: • Maternal age • Marital status • Maternal education, medicaide coverage WA State Post-Partum Depression • 2008: ~9% of mothers reported always or often feeling down, depressed or hopeless, 10% reported always or often having little interest or pleasure in doing things (two questions combined identify subjects at higher risk for post partum depression). • 2008: 13% of women expressed experiencing postpartum depression symptoms. More women on Medicaid reported symptoms than women who did not receive Medicaid. • 2010:11% of women expressed feeling down, depressed or sad. More women on Medicaid (14%) reported symptoms than women who did not receive Medicaid (8%). http://www.doh.wa.gov/Portals/1/Documents/Pubs/950153_PerinatalIndicatorsforWashingtonResidents.pdf, May 2012. WA State PDS Prevalence, 2004-2005 (MMWR, 2008) Age Race/ethnicity Marital status Education < 20 > 30 White/non Hispanic Black/non Hispanic Hispanic married other < 12 > 12 20 % 9% 11 % 20 % 14 % 12 % 17 % 19 % 11 % Washington State PRAMS WA State PRAMS