OGGYN Trauma - M3 Ob/Gyn Clerkship at the USC SOM
advertisement
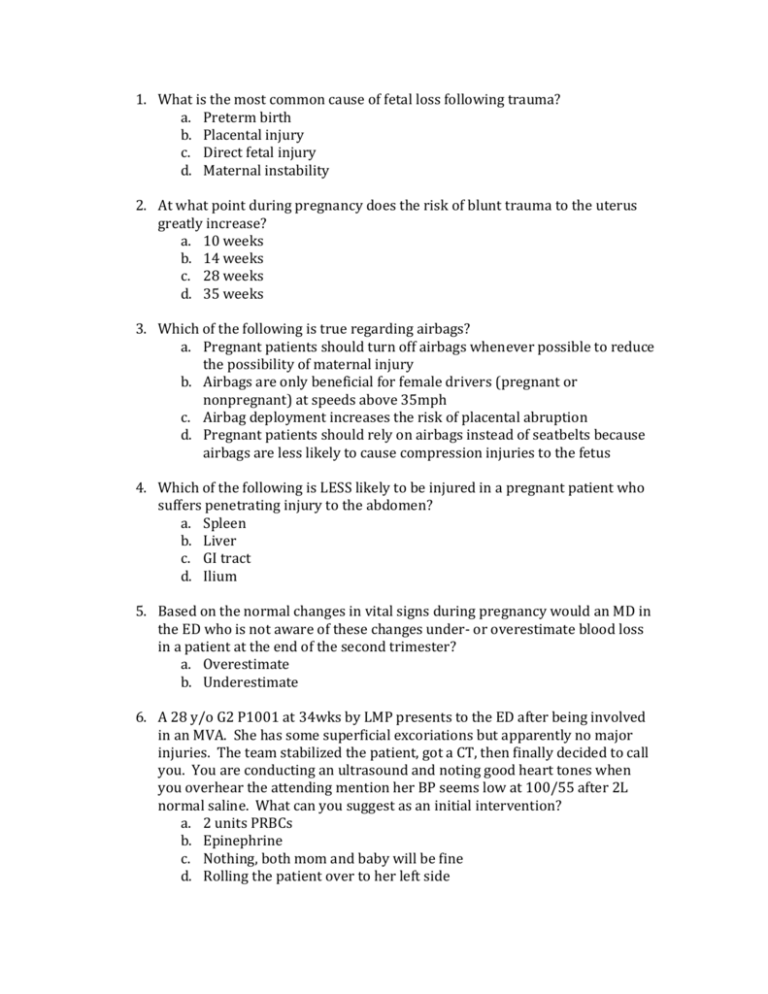
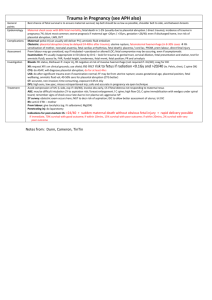
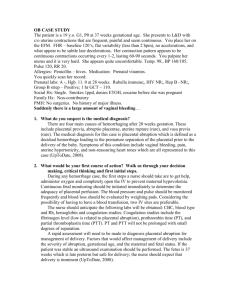
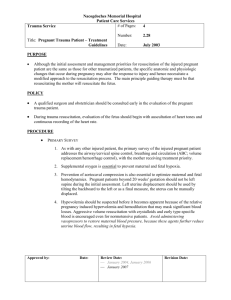
1. What is the most common cause of fetal loss following trauma? a. Preterm birth b. Placental injury c. Direct fetal injury d. Maternal instability 2. At what point during pregnancy does the risk of blunt trauma to the uterus greatly increase? a. 10 weeks b. 14 weeks c. 28 weeks d. 35 weeks 3. Which of the following is true regarding airbags? a. Pregnant patients should turn off airbags whenever possible to reduce the possibility of maternal injury b. Airbags are only beneficial for female drivers (pregnant or nonpregnant) at speeds above 35mph c. Airbag deployment increases the risk of placental abruption d. Pregnant patients should rely on airbags instead of seatbelts because airbags are less likely to cause compression injuries to the fetus 4. Which of the following is LESS likely to be injured in a pregnant patient who suffers penetrating injury to the abdomen? a. Spleen b. Liver c. GI tract d. Ilium 5. Based on the normal changes in vital signs during pregnancy would an MD in the ED who is not aware of these changes under- or overestimate blood loss in a patient at the end of the second trimester? a. Overestimate b. Underestimate 6. A 28 y/o G2 P1001 at 34wks by LMP presents to the ED after being involved in an MVA. She has some superficial excoriations but apparently no major injuries. The team stabilized the patient, got a CT, then finally decided to call you. You are conducting an ultrasound and noting good heart tones when you overhear the attending mention her BP seems low at 100/55 after 2L normal saline. What can you suggest as an initial intervention? a. 2 units PRBCs b. Epinephrine c. Nothing, both mom and baby will be fine d. Rolling the patient over to her left side 7. A 36 y/o G1P0 at 31wks by LMP is admitted for observation following an MVA. She is stable and all labs and imaging studies have been normal thus far. 2 hours after admission you look at her monitoring strip and decide she may be going into pre-term labor. Which of the following should you be cautious of using in this situation? a. Indomethacin b. Magnesium sulfate c. Brethine 1. B- placental injury. Placental abruption occurs in up to 40% of cases of severe blunt abdominal trauma. Direct fetal injury occurs in <1% of cases. Maternal instability and preterm birth are both somewhere between these extremes. Placental abruption causes release of thromboplastins which can further complicate a hemorrhagic state. Fetal monitoring would show late decelerations. 2. B- 14 weeks. The uterus is below the anterior pelvic brim until approximately 1214 weeks gestation. After this point the fetus is much more likely to be affected in a case of blunt abdominal trauma. 3. B- Airbags are only beneficial for female drivers (pregnant or nonpregnant) at speeds above 35mph . Airbags were initially designed for average male drivers. As such the force with which they deploy can cause harm to smaller female drivers. The benefits outweigh the risks at speeds above 35mph. C is not true. A study conducted in 2006 found no difference in the rate of placental abruption when airbags did vs did not deploy. 4. C- GI tract. During pregnancy the uterus shields the GI tract from penetrating injury. Studies of gun shot wounds to the abdomens of pregnant women have found that 40-70% of fetuses and 5-10% of mothers die from these injuries. 5. A-overestimate. Blood pressure begins to decrease early in the 2nd trimester. Systolic drop 2-4mmHg and diastolic by 5-15mmHg. Heart rate increases 10-15 bpm. This picture of hypotension and tachycardia can cause a physician to overestimate volume loss after trauma. 6. D- Rolling the patient over to her left side. Many ER physicians may not be cognizant of this simple intervention. If the patient is supine this is the first thing to try. Her vitals are not bad enough to warrant PRBCs and epinephrine is not a first line pressor in pregnant patients. Ephedrine and phenylephrine are first line pressors because they have fewer effects on the placental vasculature. 7. C- Brethine. Brethine (Terbutaline) is a beta 2 agonist. This can cause maternal tachycardia, an effect that can mask maternal hemorrhage. Brown, H. L. (2009). Trauma in Pregnancy. Obstetrics and Gynecology, 114, 147-160. Oxford, C. M. & Ludmir, J. (2009). Trauma in Pregnancy. Clinical Obstetrics and Gynecology, 52, 611-629.