revised EC Coupling
advertisement

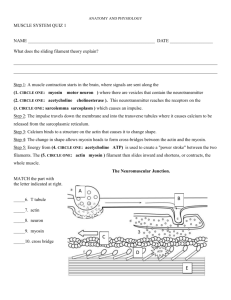
Muscles Alive! Excitation – Contraction Coupling, Mechanics and Adaptations Anatomy and Physiology Spring 2016 Stan Misler <latrotox@gmail.com> A. Short Review of Skeletal muscle Machina carnis (machine made of flesh): Tissue using chemical energy stored in high energy phosphate bonds (hydrolysis of ATP) to generate cycles of internal tension -> moving of joint across arc or fixing joint against a load. Muscle force transmitted to tendon Muscle = parallel bundles of multinucleated cells. Unit of function = sarcomere of interdigitating actin and myosin filaments B. Linkage of action potential in muscle plasma membrane (sarcolemma) to subsequent muscle contraction (i.e., excitation-contraction or EC coupling) (i) Muscle membrane is depolarized by acetylcholine released from nerve terminal -> (ii) Muscle action potential propagates along T –tubules which have membrane proteins that can link up with Ca channels in terminal cisterns of sarcoplasmic reticulum (SR) (iii) Pulling out foot process of SR Ca channel-> release of Ca from SR into cytoplasm near sarcomeres-> (iv) Ca binding to actin allows interaction of actin & myosin (cross bridge formation) -> (vi) Generation of tension: head of myosin molecule rotates and pulls actin until myosin head falls off actin. myosin Actin Heads of myosin contacting actin and forming cross-bridges C. Details of EC coupling in skeletal myocytes 1. Skeletal myocytes, like nerve cell bodies and axons, conduct action potentials 2. In skeletal myocytes regions of indented plasma membrane, the T tubules, conduct the AP towards center of fiber where they make close contacts with Ca loaded sarcoplasmic reticulum (SR, elaborated endoplasmic reticulum) 3. Skinned muscle fibers (plasma membrane stripped off) dipped in fluids of different Ca concentrations causes fiber contraction with threshold cytosolic [Ca] at least 100 nM as measured by Ca sensing dye previously injected into the cytoplasm 4. In intact muscle fibers the rise in cytosolic Ca comes from T tubule –SR “electrical synapse” : Propagation of AP down T-tubule possessing dihydropyridine receptor proteins (DHPR) changes DHPR configuration allowing it to pull on “foot” of Ca release channel, the ryanodine receptor, RyR, in terminal cisternae of SR-> localized increase in cytosolic [Ca] 5. Binding of Ca to troponin changes conformation of blocking tropomyosin -> interaction of head of myosin interdigitating with actin -> actin myosin bond at 45o from myosin stalk -> actin/myosin cross bridge formation. D. Actin /myosin crossbridges and contraction. From interference and electron microscopies, interdigitating actin and myosin filaments are clearly seen where myosin projections (heads) are uniformly distributed over myosin filaments except at middle region. With contraction sarcomeres are reduced in length, while with stretching sarcomeres increase in length. However the lengths of interdigitating actin and myosin filaments do not change (see left) suggesting that actin and myosin slide past each other. Also, during contraction heads of myosin are seen to attach to actin and then tilt pulling actin towards the center of the sarcomere (see right). Since length of putative crossbridge is small (0.2 um) compared with sarcomere contractions of 1 um, during contraction there must be repeated cycles of attachment/pull racheting pull/detachment Direction of sliding of actin with respect to myosin heads 1. Sliding filament model/ swinging crossbridge model for contraction = myosin heads cyclically walking along actin (left) myosin head attaching to actin, twisting/ tilting -> pulling actin and then falling off at extreme position after binding ATP. New cross bridges can be formed as long as ATP be hydrolyzed and there is sufficient local cytosolic Ca vs. (right) poorly breakable actin/myosin bonds at low cytosolic [ATP] = rigor complex and rigor mortis until proteins breakdown Tilting / twisting and dragging to dissociate 2. Length-tension and force-velocity curves basic to muscle contraction are best explained by sliding filament hypothesis a. Length-tension curve: Optimization of pre-contraction sarcomere length to one which provides optimal actin/myosin filament overlap and presumed cross-bridging opportunity (2.1 um), gives largest tension with in response to repeated or tetanic muscle stimulation (= jittery tension at almost no change in sarcomere length). b. Generating a force - velocity curve The lower the load the sarcomere must support, (i) the smaller the average number of cross-bridges needed to form to support the load, (ii) the faster the muscle shortens , (iii) the faster the dissociation of actin – myosin complex (less resistance to head tilting 3. 4. Adapting muscle to specific task. Increasing # sarcomeres in series (longer fiber) -> greater speed and extent of maximum contraction while increasing # of sarcomeres in parallel (thicker fiber) -> greater maximum force of contraction E. Types of muscles: how they look and function Skeletal Muscle 1. 2. 3. Tension generates movement of part of body in relation to external environment (force on tendon and movement of joint). This is critical for coarse movements (walking) or fine movements needed for communication (speech, writing and pointing) Individual non-communicating muscle fibers are grouped into motor units innervated by a single motor neuron originating in the spinal cord. The depolarizing end-plate potential sets off an muscle action potential of several ms duration that propagates along the muscle surface as well deep into the fiber via T-tubules. This triggers the releases Ca from internal stores in SR. Muscle twitches of ~ 50 ms in duration are set off Operational view of motor unit: motor nerve fired continuously by an electrode placed in single spinal motor neuron (MN) results in glycogen loss by hundreds of muscle fibers the MN innervates Cardiac muscle 1. Atria and ventricles are cardiac chambers composed of networks of non-innervated, striated muscle cells conducting long duration APs and connected to one another by electrical junctions through which K ions flow. 2. The cardiac impulse begins with spontaneously firing of APs by sinoatrial node located at junction between vena cava and right atrium spread by specialized conducting fibers to atria and ventricles. 3. Action potentials, first propagating in atria and later in ventricles, are 200-300 ms in duration with 150 ms plateaus near 0 mV, the latter due to slow opening and slow inactivation of voltage dependent Ca channels. Each AP sets off contractile tension lasting nearly 300 ms which empties by ~80% the contents of both atria and ventricles. Cardiac myocyte EC coupling: Ca entry induced Ca release from SR (CICR) Long plateau of cardiac AP provides long opening of plasma membrane Ca channels and thus longer “trigger Ca” entry to release SR Ca Positive inotropic effect in cardiac muscle: while its shortening velocity is smaller than that of skeletal both maximal velocity and force can be increased by catecholamines 1. Smooth muscle Hollow organs in digestive, respiratory and reproductive tracts are enclosed by non- striated, spindle-shaped smooth muscle fibers which move fluids by changing the diameters of the tubes. These fibers have dense bodies at the surface into which thin actin filaments insert and more interiorly in the cell interact with small bundles of thick myosin filaments. 2. The smooth muscle impulse begins with spontaneously firing of APs in by a subset of noncontractile pacemaker fibers and spread via electrical junctions to contractile fibers. 3. Action potentials are 50 -100 ms in duration and set off contractions as long as 1 s in duration. 4. synapses made by nerve viscosities largely onto pacemaker fibers, change the efficiency of pacemaker impulses while synapses formed by nerve varicosites on contracting muscle cells change the force of contraction Smooth muscle E-C coupling pathways for entry of Ca and release of Ca from SR Unique way that Ca allows x-bridge formation Velocity of shortening of smooth muscle is much smaller than skeletal muscle but energy efficiency is much greater: smooth muscle can maintain tonic tension with little consumption of ATP due to slow detachment of x-bridges