THE RESPIRATORY SYSTEM
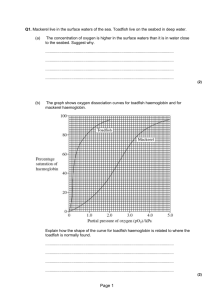
advertisement

Respiration:-exchange of O2 and CO2 between atmosphere and body cells is called respiration. 1)Exchange of O2 and CO2 between alveolar air and blood. 2)Excretion of volatile substances eg. NH3,keton bodies essential oils, alcohol, water vapours, etc. Maintenance of acid –base balance by adjusting CO2 elimination. 4)Maintenance of temp. balance by losing heat in expired air. 5)Helps venous return by dec. intra-thoracic pressure and inc. intra-abdominal pressure during inspiration. Atmospheric pressure – 760 mm Hg, Intrapleural pressure – 756 mm Hg – pressure between pleural layers Intrapulmonary pressure – varies, pressure inside lungs Diameter of airways, esp. bronchioles Sympathetic & Parasympathetic NS Surface tension tends to oppose alveoli expansion Pulmonary surfactant reduces surface tension Mechanism of inspiration:- inspiration is induced by the contraction of the diaphragm( main muscle of inspiration), along with some accessory muscles that expand chest wall. (active process) Net effect of contracting these muscles is to decrease (make more negative ) intrapleural pressure. The expansion of lung causes the gases in the alveoli to expand , creating a slightly negative alveolar pressure. This causes air to flow into the lungs. Other muscles of inspiration are used primarily during exercise or in diseases that increases airway resistance (e.g. asthma). Vertical diameter of chest cavity is inc. by downward movement of diaphragm. Antero-posterior diameter of chest cavity is inc .by elevation of ribs Expiration under resting conditions is produced simply by the relaxation of the muscles of inspiration. (passive process). The relaxation of the diaphragm and accessory muscles of inspiration increases (make more positive) intrapleural pressure. Lung deflation begins. Deflation of lung compresses the gases in the alveoli, creating a slightly positive alveolar pressure .This causes air to flow out of the lungs. Muscles of expiration are used during exercise or increased airway resistance (e.g. asthma). Vertical diameter of chest cavity is dec. by upward movement of diaphragm. Antero-posterior diameter of chest cavity is dec. by depression of ribs. 1)Diaphragm (primary muscle of inspiration). 2)Sternocleidomastoid (elevates sternum). 3)Serratus anterior. 4)scaleni( elevates first two ribs). External intercostals. (moves ribs upward and outward) 1)Elastic recoil of lungs( it is not muscle , but it is the main factor). 2)Rectus abdominus (main muscle). 3)Internal intercostals. (pull ribs downward and inward). 1)Tidal volume (TV):- It is volume of air inspired or expired with each normal breath. Value:- 500 ml. 2)Inspiratory Reserve volume (IRV):- It is extra volume of air that can be inspired forcefully over and beyond normal tidal volume. Value:- 3000 ml 3)Expiratory Reserve volume (ERV):- It is extra volume of air that can be expired forcefully over and beyond normal tidal volume. Value:- 1100 ml Residual volume (RV):- It is volume of air remaining in lungs after most forceful expiration. (amount of air that can never be expelled from lung). Value:- 1200 ml. Combination of two or more pulmonary volumes, is called pulmonary capacity. 1)Inspiratory Capacity (IC):- It is combination of tidal volume and inspiratory reserve volume. Value:- 3500 ml. 2)Functional Residual Capacity (FRC):- It is combination of expiratory reserve volume and residual volume OR volume of gas in the lungs at the end of a passive expiration or with the glottis open and all respiratory muscles relaxed. This is also considered to be the natural or equilibrium point for the respiratory system. Value:- 2300 ml. 3)Vital Capacity:- It is combination of inspiratory reserve volume, tidal volume and expiratory reserve volume. Value:- 4600 ml. 4)Total Lung Capacity (TLC):- It is combination of vital capacity and residual volume . It is the maximum volume to which lungs can be expanded with greatest possible inspiratory efforts. Value:- 5800 ml. A) Nervous control:Respiratory center. B) Chemical controlChemosensitive area in brain. Peripheral chemoreceptors ( carotid and aortic bodies). Group of neurons located bilaterally in medulla and pons which control all aspects of respiration. The Respiratory Centers Are Composed of Three Main Groups of Neurons:1)The Dorsal Respiratory Group. 2)The Pneumotaxic Center. 3)The Ventral Respiratory Group. For spontaneous breathing, an intact medulla must be connected to the diaphragm (via the phrenic nerve). Thus a complete C1 or C2 lesion will prevent diaphragmatic breathing but not complete C6 or lower lesion. 1)Increasen activity of vasomotor center . 2)Increase body temprature. 3)Increase CO2. 4)Decrease O2 How Gases Are Transported O2 is transported by the blood either, ◦ Combined with haemoglobin (Hb) in the red blood cells (>98%) or, ◦ Dissolved in the blood plasma (<2%). The resting body requires 250ml of O2 per minute. We have four to six billion haemoglobin containing red blood cells. Haemoglobin molecules can transport up to four O2’s When 4 O2’s are bound to haemoglobin, it is 100% saturated, with fewer O2’s it is partially saturated. Co-operative binding: haemoglobin’s affinity for O2 increases as its saturation increases. Oxygen binding occurs in response to the high PO2 in the lungs Haemoglobin saturation is the amount of oxygen bound by each molecule of haemoglobin Each molecule of haemoglobin can carry four molecules of O2. When oxygen binds to haemoglobin, it forms OXYHAEMOGLOBIN; Haemoglobin that is not bound to oxygen is referred to as DEOXYHAEMOGLOBIN. The binding of O2 to haemoglobin depends on the PO2 in the blood and the bonding strength, or affinity, between haemoglobin and oxygen. The graph on the following page shows an oxygen dissociation curve, which reveals the amount of haemoglobin saturation at different PO2 values. Reveals the amount of haemoglobin saturation at different PO2 values. Haemoglobin saturation is determined by the partial pressure of oxygen. When these values are graphed they produce the Oxygen Disassociation Curve In the lungs the partial pressure is approximately 100mm Hg at this Partial Pressure haemoglobin has a high affinity to 02 and is 98% saturated. In the tissues of other organs a typical PO2 is 40 mmHg here haemoglobin has a lower affinity for O2 and releases some but not all of its O2 to the tissues. When haemoglobin leaves the tissues it is still 75% Lungs at sea level: PO2 of 100mmHg haemoglobin is 98% SATURATED When the PO2 in the lungs declines below typical sea level values, haemoglobin still has a high affinity for O2 and remains almost fully saturated. Lungs at high elevations: PO2 of 80mmHg, haemoglobin 95 % saturated Even though PO2 differs by 20 mmHg there is almost no difference in haemoglobin saturation. Blood acidity… Blood temperature… Carbon Dioxide concentration Respiratory Response to Exercise BLOOD TEMPERATURE increased blood temperature reduces haemoglobin affinity for O2 hence more O2 is delivered to warmed-up tissue BLOOD Ph • lowering of blood pH (making blood more acidic) • caused by presence of H+ ions from lactic acid or carbonic acid • reduces affinity of Hb for O2 • and more O2 is delivered to acidic sites which are working harder CARBON DIOXIDE CONCENTRATION • the higher CO2 concentration in tissue • the less the affinity of Hb for O2 • so the harder the tissue is working, the more O2 is released Carbon dioxide also relies on the blood for transportation. Once carbon dioxide is released from the cells, it is carried in the blood primarily in three ways… Dissolved in plasma, As bicarbonate ions resulting from the dissociation of carbonic acid, Bound to haemoglobin. Part of the carbon dioxide released from the tissues is dissolved in plasma. But only a small amount, typically just 7 – 10%, is transported this way. This dissolved carbon dioxide comes out of solution where the PCO2 is low, such as in the lungs. There it diffuses out of the capillaries into the alveoli to be exhaled.