Gas Exchange Live Show
advertisement

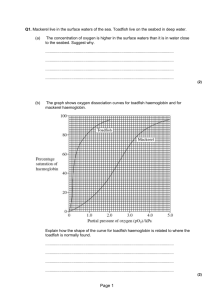
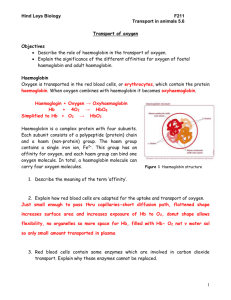
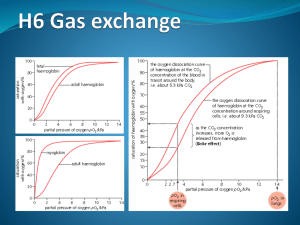
GAS EXCHANGE • Gaseous exchange refers to the exchange of gases, namely Oxygen and Carbon Dioxide and relies on a process called diffusion. • Diffusion is the movement of gases from an area of high pressure to low. The difference between the high and low pressure is called the diffusion gradient • The bigger the diffusion gradient the greater the diffusion and gaseous exchange that takes place. DEFINITIONS Partial Pressure: “Air is made up of several gases, each of these gases make up air as a whole, individually they exert part (partial) of total air pressure” Partial pressure = Barometric pressure x Fractional pressure e.g. pO2 = 760 x 0.21 = 159.6 mmHg Work out the partial pressures for: 1. Co2 (carbon dioxide) 2. N2 (Nitrogen) 3. H2o (Water) The partial pressures of the 4 gases add up to 760mm Hg. Dalton’s Law; in a mixture of gases, the total pressure equals the sum of the partial pressures exerted by each gas. Oxygen Transport • O2 is transported by the blood either, – Combined with haemoglobin (Hb) in the red blood cells (>98%) or, – Dissolved in the blood plasma (<2%). Oxygen Transport • The resting body requires 250ml of O2 per minute. • We have four to six billion haemoglobin containing red blood cells. • The haemoglobin allows nearly 70 times more O2 than dissolved in plasma. The Site of Gas Exchange • External Respiration • Pp of O2 higher in alveoli than pulmonary capillaries so O2 diffuses to blood • Pp of CO2 diffuses from pulmonary capillaries into alveoli •Internal respiration •Pp of CO2 in muscle tissues is higher than blood so diffuses into capillaries •Pp of O2 higher in blood than muscle tissues so diffuses from capillaries into muscle tissue Factors Influencing External Respiration Efficient external respiration depends on 3 main factors 1) Surface area and structure of the respiratory membrane 2) Partial Pressure gradients 3) Matching alveolar airflow to pulmonary capillary blood flow. Gas exchange at the lungs There is imbalance between gases in the alveoli and the blood that causes a pressure gradient which results in a movement of gases across the respiratory membrane. Movement is 2 way – oxygen from alveoli to blood and carbon dioxide from blood to alveoli The diffusion gradient As oxygen is moved around the body to the muscle tissues for use, the partial pressure it exerts is greatly reduced (high to low pressure) (po2) Oxygen in atmosphere air - 159 mmHg Oxygen in the Alveoli - 105 mmHG Oxygen in the arteries - 100 mmHg Oxygen in the body cells - 40 mmHg Oxygen back to lungs - 40mmHg This is mirrored in the sense that as the muscle cells produce carbon dioxide where co2 pressure is at its highest it travels to the lungs where pressure expels it out of the body when we breath With altitude there is a decrease in atmospheric pressure but the percentage of gases within air remains the same At sea level: Resting ppO2 in the arteries is 100mmHg At the muscle tissue at sea is 40mmHg At altitude of 8000 feet: Resting ppO2 in the arteries falls to 60mmHg At the muscle tissue at altitude is still 40mmHg Pressure gradient falls from 60 to 20 therefore oxygen movement is greatly reduced Endurance training Long distance runners etc may train at high altitude based on the principle that the body will create more red blood cells and haemoglobin to adapt to oxygen shortage at muscles Although recent research suggests living at altitude and training at sea level maybe more advantageous Haemoglobin Haemoglobin molecules can transport up to four O2’s When 4 O2’s are bound to haemoglobin, it is 100% saturated, with fewer O2’s it is partially saturated. Co-operative binding: haemoglobin’s affinity for O2 increases as its saturation increases. Oxygen binding occurs in response to the high PO2 in the lungs Lets Now Look at Haemoglobin Saturation • Haemoglobin saturation is the amount of oxygen bound by each molecule of haemoglobin • Each molecule of haemoglobin can carry four molecules of O2. • When oxygen binds to haemoglobin, it forms OXYHAEMOGLOBIN; • Haemoglobin that is not bound to oxygen is referred to as DEOXYHAEMOGLOBIN. Haemoglobin Saturation • The binding of O2 to haemoglobin depends on the PO2 in the blood and the bonding strength, or affinity, between haemoglobin and oxygen. • The graph on the following page shows an oxygen dissociation curve, which reveals the amount of haemoglobin saturation at different PO2 values. The Oxygen Disassociation Curve In the lungs the partial Haemoglobin saturation is determined pressure is approximately by the partial pressure of oxygen. When 100mm Hg at this Partial haemoglobin these values are graphed theyPressure produce has a high affinity to 02 the Oxygen Disassociation and Curve is 98% saturated. In the tissues of other organs a typical PO2 is 40 mmHg here haemoglobin has a lower affinity for O2 and releases some but not all of its O2 to the tissues. When haemoglobin leaves the tissues it is still 75% saturated. Haemoglobin Saturation at High Values Lungs at sea level: PO2 of 100mmHg haemoglobin is 98% SATURATED When the PO2 in the lungs declines below typical sea level values, haemoglobin still has a high affinity for O2 and remains almost fully saturated. Lungs at high elevations: PO2 of 80mmHg, haemoglobin 95 % saturated Even though PO2 differs by 20 mmHg there is almost no difference in haemoglobin saturation. Haemoglobin Saturation at Low Values What effects effective dissociation between oxygen and haemoglobin? 1. 2. 3. 4. Fall in the pO2 within the muscle Increase in blood and muscle temperature Increase in pCO2 within the muscle Fall in pH due to lactic acid production Factors Altering Haemoglobin Saturation (Exercise) The Bohr Shift Gas exchange at the muscles This is very similar to exchange at the lungs, high to low pressure gradient. At the muscles the oxygen attaches to myoglobin rather than haemoglobin and is taken to the mitochondria within the cell to be used (Slow twitch muscle fibres have higher amounts of myoglobin)