red blood cells
advertisement

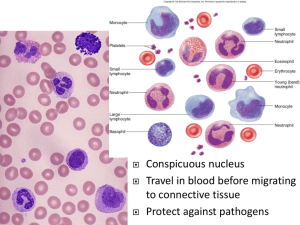
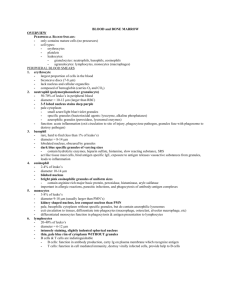
Blood and hemopoiesis Lecture, 26.4.2012 Blood structure and function • • • • • • • • • • „connective tissue“ (cells and ECM ) blood cells and plasma erythrocytes (red blood cells) leukocytes (white blood cells) platelets serum – differs from plasma by the absence of factors (oraganic and anorganic), which leave plasma during coagulation (has been involved in clot) hematocrit - the volume of combined formed elements in the blood after centrifugation erythrocytes – 43% leukocytes and paltelets (buffy coat) 1% 40-50% male 30-40% female Blood structure and function • total volume 5,5L • transport : oxygen, CO2, nutrients, waste products, hormones… • maintaining of acid/base and osmotic balance, body temperature • plasma: water, proteins (albumin, globulins, clotting proteins, complement, lipoproteins), inorganic salts, ions, nitrogenous compounds, nutrients, gases Formed elements Erythrocytes red blood cells biconcave-shaped discs without nuclei size: 7,5 x 2,6 μm (in the middle only 0,8 μm) shape provides the cell with larger surface area thus enhancing its capability for the exchange of gases number: 3,9 – 5,5 milions in 1μL it depends on age, gender, race and other factors as diet,altitude ect. Therefore, every country has to determinate and statistically calculate reference values. plasmalemma (integral proteins: glycophorins, ion channels, anion transporters), subplasmalemmal cytoskeleton (spectrin, actin tetramers).. hemoglobin (33%), enzymes: glycolysis, hexosemonophosphate shunt they survive 120 days in circulation oligosacharides on the surface, that acts like antigen – AB0 system determination Clinical applications anemia polycythemia – physiological adaptation or haemoblastosis – it increases blood viscosity anisocytosis – higher variability in size macrocytes – greater – impairment of maturation (deficiency of vit. B12) microcytes – smaller (defeiciency of iron) sicle cell disease/thallasemia – point mutation in the gene for hemoglobin – HBS shape – abnormal/crescent shape of RBC (red blood cell) – anemia, small vessels/venules obstruction Leukocytes – white blood cells granulocytes a agranulocytes neutrophil eosinophil basophill lymphocyte monocytes • granulocytes • neutrophils (polymorphonuclear leucocytes) • eosinophils • basophils • agranulocytes/ mononuclear – see mononuclear phagocyte system • lymphocytes , B, T • monocytes Leukocytes function • number 6500 – 10,000 in 1μL • do not function in blood stream, but use it for transport to connective tissue, where perform their function • diapedesis – active migration from blood stream do CT Granulocytes content of two granule types: specific with specific function for particular garnulocyrte type nonspecific/azurophilic (lysosomes) all granulocytes in periferal blood are terminal postmitotic stages of the cell development – cells do not divide. They survive only few days in peripheral blood nuclei are divided in two or more lobes Neutrophilic granulocytes 60-70% of lekocytes size: 12-15 μm (in smear) nucleus is divides in two or three lobes that are connected by chromatin bridges; (small appendage to the nucleus inactive second X chromosome – Barr body in females´neutrophiles good indentified) specific granules – small, near the limit of resolution in LM lysosomes azurophilic granules – 0,5 μm glycogen – source of energy – anaerobic metabolism phagocytosis, oxidative burst – (H2O2) and oxygen radicals Neutrophil • chemoattraction to sites of microorganism invasion • phagocytosis of microorganisms - phagosome • release of hydrolytic enzymes and by reactive oxidative compounds in phagosome (superoxide, hydrogen peroxide, hypochlorous acid (oxidative stress) • only once perform a phagocytosis and die (pus) Eosinophilic granulocytes 2-4% size: 12-15 μm bilobed nucleus specific granules: crystalline core (internum) – major basic protein matrix (externum) - lighter allergy, parasitic infections modulation of inflamation (inactivation of leukotrienes and histamine) Basophilic granulocytes less that 1% size 12-15 μm nucleus is divided in irregular lobes, but it is not distinct because it is covered by granules specific granules – metachromatic, content of heparine and histamine – liberation of granules – degranulation - after binding of certain antigens. similarity between basophil and mast cell Lymphocytes on the basis of size: small (6-8μm), medium-sized and large (up to 18μm). small lymphocytes prevail in blood – memory cells large round nucleus, chromatin is condensed, nucleolus thin rim of cytoplasm, ribosomes, azurophilic granules Lymphocyte function T and B lymphocytes – specific immunity (T lymphocytes prevail in peripheral blood: 65% - 75% ) B lymphocytes – humoral – differentiation in plasma cells – production of antibodies T lymphocytes – cytotoxic CD8 (induce apoptosis) , helper CD4 (cooperate with B-lymphocytes and macrophages) NK (natural killers) medium-sized lymphocytes – 10-15% in peripheral blood – nonspecific - innate immune response Monocytes size: 12 -20μm oval, horseshoe or kidney shaped nucleus, excentrically placed basophilic cytoplasm, azurophilic granules (lysosomes), RER, polyribosomes, mitochondria, Golgi complex monocytes differentiate into macrophages (antigen presenting cells) Leukocytes - differential white cell count: the distribution of the diffrent types of white cells present in circulating blood 6 000 -10 000 in 1μL granulocytes neutrophiles 60 -70%, 3500-7500 eosinophiles 2-4%, 150 - 400 basophiles 0-1% agranulocytes lymphocytes 20-30% monocytes 3-8% 50-100 1500-2500 200-800 Platelets - thrombocytes nonnucleated, disc-like cell fragments of megakaryocytes size - 2-4 μm 200 000– 400 000 in uL central zone containing granules – granulomera and peripheral lighter zone - hyalomera hyalomera: open canalicular system – invagination of superficial plasmalemma, marginal bundle of microtubules, actin and myosin – contractile granulomera: mitochondria, glycogen, granules (δ - dense bodies – ATP and serotonin; α – platelet-specific proteins: fibrinogen, PdGF, FGF, von Willebrandt factor, platelet-specific factor IV; λ lysosomes) hemophilia – inherited deficiency of factor VIII or IX Von Willebrand disease – the most frequent bleeding disorder, hereditary disease with abnormal or defect of von Willebrand factor Platelets Hemopoeisis Chick embryo – blood islands, 2ED • mesoderm of yolk sac •(3 week) • intraembryonic splanchnic mesoderm (3week – 6week) • liver • spleen (hepato-lineal period) •bone marrow (from8week) Hemopoeisis hemopoiesis is a result of simultaneous proliferation and differentiation hemopoetic stem cells – types and terms: pluripotent stem cell – self-renewal – low mitotic activity multipotent stem cell – lymphoid and myeloid stem cells unipotent - progenitor cells - colony forming cells - self-renewing – high mitotic activity precursor cells (blasts) – not self-renewing (lymphoblast, erythroblast....) mature cells – (cytes) (lymphocyte, erythrocyte) Development of blood cells regulation microenvironment – cells of stroma, extracellular matrix growth factors: growth factors – stimulation of mitotic activity colony-stimulating factors (CSF) hematopoietins (erythropoietin – synthesis in kidney, thrombopoeitin - synthesis in liver) Red bone marrow stroma: hematopoietic cords and sinusoids stroma – reticular connective tissue (reticular cells and reticular fibres – (collagen type 1 and 3, fibronectin, laminin and proteoglycans) sinusoids – capillaries with discontinuous endothelium stem cells – they can differentiate also in other cellular types that blood cells – appropriate stimulation is necessary Haemopoiesis Erythropoiesis Proerythroblast – large cell with loose chromatin, nucleoli and basophilic cytoplasm Basophilic erythroblast – condensed nucleus, basophilic cytoplasm - polyribosomes Polychromatophilic erythroblast – polyribosomes decrease, hemoglobin appears Orthochromatophilic erythroblast – eosinophilic cytoplasmhemoglobin, maximally condensed nucleus – nucleus expulsion Reticulocyte – rest of ribosomes – substantia reticulofilamentosa – 1% in peripheral blood Erythrocyte Erythropoiesis erythropoietin, iron, folic acid, cyancobalamin (vit B12) 3 - 5 division from proerythroblast to erythrocyte approximately 7 days from proerythroblast to reticulocyte decrease of the cell volume condensation of chromatin (pycnotic nucleus) and its expulsion synthesis of hemoglobin and successive loss of basophilia (polyribosomes) Granulopoiesis Gardual synthesis of azurophilic and later also specific granules Myeloblast – finely dispersed chromatin, no granules Promyelocyte – basophilic cytoplasm, Golgi complex and azurophilic granules neutrophilic, basophilic and eosinophilic myelocytes – condensation of nucleus, appearance of specific granules neutrophilic metamyelocyte – band cell – mature granulocyte Maturation of lymphocytes no specific morphologic differences stem cells - progenitors in bone marrow –– they do not have antigens specific for B and T lymphocytes maturation in thymus (precursors T- lymphoblasts – differentiate in mature lymphocytes) or in bone marrow (B – lymphoblasts, lymphocytes), they may divide in periphery in lymphoid organs (spleen, lymph node, tonsil) Maturation of monocytes monoblast – identical with myeloblast promonocyte – large cell – up to 18μm; basophilic cytoplasm, large slightly indented nucleus, large amount of RER, large Golgi complex formation of azurophilic granules – lysosomes in blood, they circulate approximately 8 hours they survive in periphery for several months – macrophages - antigen presenting cells Origin of platelets megakaryoblast – 15 - 50 μm, large ovoid nucleus, numerous nucleoli. Polyploid cell - up to 30 sets of chromosomes (reflecting its size) megakaryocyte – giant cell - 35 – 150 μm. irregular nucleus, numerous mitochondria, welldeveloped RER and extensive Golgi complex. Formation of granules. Invagination of plasmalemma – demarcation membranes – they surround areas – processes – fragmentation – release of platelets into the blood after dessintegration of cytoplasm into the platelets, megakaryocyte die by apoptosis