The s Skeletal System
advertisement

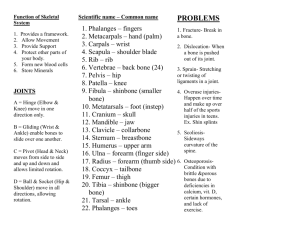
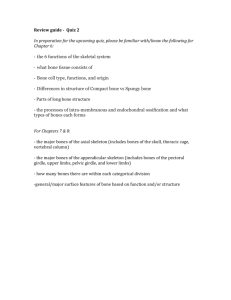
The Skeletal System Function of Bones Support – form the framework that supports the body and cradles soft organs Protection – provide a protective case for the brain, spinal cord, and vital organs Movement – provide levers for muscles Mineral storage – reservoir for minerals, especially calcium and phosphorus Blood cell formation – hematopoiesis occurs within the marrow cavities of bones Bone Markings Bulges, depressions, and holes that serve as: – – – Sites of attachment for muscles, ligaments, and tendons Joint surfaces Conduits for blood vessels and nerves Bone Markings: Projections – Sites of Muscle and Ligament Attachment Tuberosity – rounded projection Crest – narrow, prominent ridge of bone Trochanter – large, blunt, irregular surface Line – narrow ridge of bone Bone Markings: Projections – Sites of Muscle and Ligament Attachment Tubercle – small rounded projection Epicondyle – raised area above a condyle Spine – sharp, slender projection Process – any bony prominence Bone Markings: Projections – Projections That Help to Form Joints Head – bony expansion carried on a narrow neck Facet – smooth, nearly flat articular surface Condyle – rounded articular projection Ramus – armlike bar of bone Bone Markings: Depressions and Openings Meatus – canal-like passageway Sinus – cavity within a bone Fossa – shallow, basinlike depression Groove – furrow Fissure – narrow, slitlike opening Foramen – round or oval opening through a bone The Skeletal and Muscular Systems Video There are 206 bones in the human body A. The axial skeleton includes the skull and the vertebral column. Frontal View of the Skull The Skull The skull, the body’s most complex bony structure, is formed by the cranium and facial bones Cranium – protects the brain and is the site of attachment for head and neck muscles Facial bones – – – Supply the framework of the face, the sense organs, and the teeth Provide openings for the passage of air and food Anchor the facial muscles of expression Anatomy of the Cranium Eight cranial bones – two parietal, two temporal, frontal, occipital, sphenoid, and ethmoid Cranial bones are thin and remarkably strong for their weight Skull: Posterior View Parietal Bones and Major Associated Sutures Form most of the superior and lateral aspects of the skull Superior View of the Skull Posterior View of the Skull 1. Occipital Bone 2. Lambdoidal Suture 3. Parietal Bone 4. Sagittal Suture 5. Coronal Suture 6. Frontal Bone Lateral View of the Skull 1.Parietal Bone 2. Coronal Suture 3. Frontal Bone 4. Nasal Bone 5.Vomer 6. Lacrimal Bone 7. Orbital Part of Ethmoid 8. Zygomatic Bone 9. Maxilla 10. Body of Mandible 11. Ramus of Mandible 12.Coronoid Process 13.Mandibular Condyle 14.Mental Foramen 15.Styloid Process 16. External Acoustic Meatus 17. Mastoid Process 18. Zygomatic Process 19.Temporal Bone 20. Greater Wing of Sphenoid 21.Inferior Temporal Line 22. Superior Temporal Line 23.Squamosal Suture 24.Lambdoidal Suture 25.Occipital Bone Bones of the Skull Inferior of the Cranial Vault The bone at the top is the Frontal Bone. The tongue shaped bone below the Frontal Bone is the Ethmoid Bone. Below that is the Sphenoid Bone. To the left and the right in below the Sphenoid Bone are the Left and Right Temporal Bones. In the Occiput at the bottom of the picture you will notice a large opening, called the Foramen Magnum, through which the spinal cord passes. (Photo by Paula Kliewer Photography) Inferior View of the Skull 1.Anterior Palatine Foramen 2. Palatine Process of Maxilla 3. Palatine 4. Greater Palatine Foramen 5.Lesser Palatine Foramen 6. Pterygoid Processes of Sphenoid 7.Zygomatic Process 8. Squamous Part of Temporal Bone 9. Mandibular Fossa 10. Styloid Process 11.Stylomastoid Foramen 12. Mastoid Process 13.Mastoid Foramen 14. Superior Nuchal Line 15. External Occipital Protruberance 16.Median Nuchal Line 17. Inferior Nuchal Line1 8.Foramen Magnum 19. Condyloid Canal 20.Occipital Condyle 21.Hypoglossal Canal 22.Jugular Foramen 23.Carotid Canal 24.Foramen Spinosum 25.Foramen Ovale 26.Foramen Lacerum 27.Vomer 28.Transverse Palatine Suture 29.Median Palatine Suture Hyoid 1. Greater horns 2.Lesser horns 3. Body Temporal Bones Sphenoid Bone Ethmoid Bone Wormian Bones Tiny irregularly shaped bones that appear within sutures Mandible and Its Markings Maxillary Bone Orbits Nasal Cavity Nasal Cavity Paranasal Sinuses Vertebral Column Vertebral Column Formed from 26 irregular bones (vertebrae) connected in such a way that a flexible curved structure results – – – – Cervical vertebrae – 7 bones of the neck Thoracic vertebrae – 12 bones of the torso Lumbar vertebrae – 5 bones of the lower back Sacrum – bone inferior to the lumbar vertebrae that articulates with the hip bones Vertebral Column: Curvatures Posteriorly concave curvatures – cervical and lumbar Posteriorly convex curvatures – thoracic and sacral Abnormal spine curvatures include scoliosis (abnormal lateral curve), kyphosis (hunchback), and lordosis (swayback) Vertebral Column: Ligaments Anterior and posterior longitudinal ligaments – continuous bands down the front and back of the spine from the neck to the sacrum Short ligaments connect adjoining vertebrae together Vertebral Column: Intervertebral Discs Cushionlike pad composed of two parts – – Nucleus pulposus – inner gelatinous nucleus that gives the disc its elasticity and compressibility Annulus fibrosus – surrounds the nucleus pulposus with a collar composed of collagen and fibrocartilage General Structure of Vertebrae Body or centrum – disc-shaped, weightbearing region Vertebral arch – composed of pedicles and laminae that, along with the centrum, enclose the vertebral foramen Vertebral foramina – make up the vertebral canal through which the spinal cord passes General Structure of Vertebrae Spinous processes project posteriorly, and transverse processes project laterally Superior and inferior articular processes – protrude superiorly and inferiorly from the pediclelamina junctions Intervertebral foramina – lateral openings formed from notched areas on the superior and inferior borders of adjacent pedicles Cervical Vertebrae Seven vertebrae (C1-C7) are the smallest, lightest vertebrae C3-C7 are distinguished with an oval body, short spinous processes, and large, triangular vertebral foramina Each transverse process contains a transverse foramen Cervical Vertebrae: The Atlas (C1) The atlas has no body and no spinous process It consists of anterior and posterior arches, and two lateral masses The superior surfaces of lateral masses articulate with the occipital condyles Cervical Vertebrae: The Axis (C2) The axis has a body, spine, and vertebral arches as do other cervical vertebrae Unique to the axis is the dens, or odontoid process, which projects superiorly from the body and is cradled in the anterior arch of the atlas The dens is a pivot for the rotation of the atlas Cervical Vertebrae: The Atlas (C2) Thoracic Vertebrae There are twelve vertebrae (T1T12) all of which articulate with ribs Major markings include two facets and two demifacets on the heart-shaped body, the circular vertebral foramen, transverse processes, and a long spinous process The location of the articulate facets prevents flexion and extension, but allows rotation of this area of the spine Lumbar Vertebrae The five lumbar vertebrae (L1-L5) are located in the small of the back and have an enhanced weight-bearing function They have short, thick pedicles and laminae, flat hatchet-shaped spinous processes, and a triangularshaped vertebral foramen Orientation of articular facets locks the lumbar vertebrae together to provide stability Sacrum Sacrum – – – Consists of five fused vertebrae (S1-S5), which shape the posterior wall of the pelvis It articulates with L5 superiorly, and with the auricular surfaces of the hip bones Major markings include the sacral promontory, transverse lines, alae, dorsal sacral foramina, sacral canal, and sacral hiatus Coccyx Coccyx (Tailbone) – The coccyx is made up of four (in some cases three to five) fused vertebrae that articulate superiorly with the sacrum Bony Thorax (Thoracic Cage) The thoracic cage is composed of the thoracic vertebrae dorsally, the ribs laterally, and the sternum and costal cartilages anteriorly Functions – – – – Forms a protective cage around the heart, lungs, and great blood vessels Supports the shoulder girdles and upper limbs Provides attachment for many neck, back, chest, and shoulder muscles Uses intercostal muscles to lift and depress the thorax during breathing Thoracic Cage Bony Thorax (Thoracic Cage) Sternum (Breastbone) A dagger-shaped, flat bone that lies in the anterior midline of the thorax Results from the fusion of three bones – the superior manubrium, the body, and the inferior xiphoid process Anatomical landmarks include the jugular (suprasternal) notch, the sternal angle, and the xiphisternal joint Ribs There are twelve pair of ribs forming the flaring sides of the thoracic cage All ribs attach posteriorly to the thoracic vertebrae The superior 7 pair (true, or vertebrosternal ribs) attach directly to the sternum via costal cartilages Ribs 8-10 (false, or vertebrocondral ribs) attach indirectly to the sternum via costal cartilage Ribs 11-12 (floating, or vertebral ribs) have no anterior attachment Structure of a Typical True Rib Bowed, flat bone consisting of a head, neck, tubercle, and shaft Appendicular Skeleton The appendicular skeleton is made up of the bones of the limbs and their girdles Pectoral girdles attach the upper limbs to the body trunk Pelvic girdle secures the lower limbs Pectoral Girdles (Shoulder Girdles) The pectoral girdles consist of the anterior clavicles and the posterior scapulae They attach the upper limbs to the axial skeleton in a manner that allows for maximum movement They provide attachment points for muscles that move the upper limbs Clavicles (Collarbones) The clavicles are slender, doubly curved long bones lying across the superior thorax The acromial (lateral) end articulates with the scapula, and the sternal (medial) end articulates with the sternum They provide attachment points for numerous muscles, and act as braces to hold the scapulae and arms out laterally away from the body Scapulae (Shoulder Blades) The scapulae are triangular, flat bones lying on the dorsal surface of the rib cage, between the second and seventh ribs Scapulae have three borders and three angles Major markings include the suprascapular notch, the supraspinous and infraspinous fossae, the spine, the acromion, and the coracoid process The Upper Limb The upper limb consists of the arm (brachium), forearm (antebrachium), and hand (manus) Thirty-seven bones form the skeletal framework of each upper limb Arm The humerus is the sole bone of the arm It articulates with the scapula at the shoulder, and the radius and ulna at the elbow Forearm The bones of the forearm are the radius and ulna They articulate proximally with the humerus and distally with the wrist bones They also articulate with each other proximally and distally at small radioulnar joints Interosseous membrane connects the two bones along their entire length Hand Skeleton of the hand contains wrist bones (carpals), bones of the palm (metacarpals), and bones of the fingers (phalanges) Carpus (Wrist) Consists of eight bones – – Scaphoid, lunate, triquetral, and pisiform proximally Trapezium, trapezoid, capitate, and hamate distally Metacarpus (Palm) Five numbered (1-5) metacarpal bones radiate from the wrist to form the palm – – Their bases articulate with the carpals proximally, and with each other medially and laterally Heads articulate with the phalanges Phalanges (Fingers) Each hand contains 14 miniature long bones called phalanges Fingers (digits) are numbered 1-5, beginning with the thumb (pollex) Each finger (except the thumb) has three phalanges – distal, middle, and proximal The thumb has no middle phalanx Pelvic Girdle (Hip) The hip is formed by a pair of hip bones (os coxae, or coxal) Together with the sacrum and the coccyx, these bones form the bony pelvis The pelvis – – – Attaches the lower limbs to the axial skeleton with the strongest ligaments of the body Transmits weight of the upper body to the lower limbs Supports the visceral organs of the pelvis Ilium The ilium is a large flaring bone that forms the superior region of the coxal bone It consists of a body and a superior winglike portion called the ala The broad posterolateral surface is called the gluteal surface The auricular surface articulates with the sacrum (sacroiliac joint) Major markings include the iliac crests, four spines, greater sciatic notch, iliac fossa, arcuate line, and the pelvic brim Ilium: Medial View Ischium The ischium forms the posteroinferior part of the hip bone The thick body articulates with the ilium, and the thinner ramus articulates with the pubis Major markings include the ischial spine, lesser sciatic notch, and the ischial tuberosity Pubis The pubic bone forms the anterior portion of the hip bone It articulates with the ischium and the ilium Major markings include superior and inferior rami, the pubic crest, pubic tubercle, pubic arch, pubic symphysis, and obturator foramen (along with ilium and ischium) Pubis: Medial View Comparison of Male and Female Pelvic Structure Comparison of Male and Female Pelvic Structure Characteristic Female Male Bone thickness Lighter, thinner, and smoother Heavier, thicker, and more prominent markings Pubic arch/angle 80˚–90˚ 50˚–60˚ Acetabula Small; farther apart Large; closer together Sacrum Wider, shorter; sacral curvature is accentuated Narrow, longer; sacral promontory more ventral Coccyx More movable; straighter Less movable; curves ventrally The Lower Limb The three segments of the lower limb are the thigh, leg, and foot They carry the weight of the erect body, and are subjected to exceptional forces when one jumps or runs Femur The sole bone of the thigh is the femur, the largest and strongest bone in the body It articulates proximally with the hip and distally with the tibia and fibula Major markings include the head, fovea capitis, greater and lesser trochanters, gluteal tuberosity, lateral and medial condyles and epicondyles, linea aspera, patellar surface, and the intercondylar notch Leg The tibia and fibula form the skeleton of the leg They are connected to each other by the interosseous membrane They articulate with the femur proximally and with the ankle bones distally They also articulate with each other via the immovable tibiofibular joints Tibia Receives the weight of the body from the femur and transmits it to the foot Major markings include medial and lateral condyles, intercondylar eminence, the tibial tuberosity, anterior crest, medial malleolus, and fibular notch Fibula Sticklike bone with slightly expanded ends located laterally to the tibia Major markings include the head and lateral malleolus Foot The skeleton of the foot includes the tarsus, metatarsus, and the phalanges (toes) The foot supports body weight and acts as a lever to propel the body forward in walking and running Tarsus Composed of seven bones that form the posterior half of the foot Body weight is carried primarily on the talus and calcaneus Talus articulates with the tibia and fibula superiorly, and the calcaneus inferiorly Other tarsus bones include the cuboid and navicular, and the medial, intermediate, and lateral cuneiforms Calcaneus Forms the heel of the foot Carries the talus on its superior surface Point of attachment for the calcaneal (Achilles) tendon of the calf muscles Metatarsus and Phalanges Metatarsus and Phalanges Metatarsals – – Five (1-5) long bones that articulate with the proximal phalanges The enlarged head of metatarsal 1 forms the “ball of the foot” Phalanges – – The 14 bones of the toes Each digit has three phalanges except the hallux, which has no middle phalanx Arches of the Foot The foot has three arches maintained by interlocking foot bones and strong ligaments Arches allow the foot to hold up weight The arches are: – – – Lateral longitudinal – cuboid is keystone of this arch Medial longitudinal – talus is keystone of this arch Transverse – runs obliquely from one side of the foot to the other Developmental Aspects: Fetal Skull Infant skull has more bones than the adult skull At birth, fetal skull bones are incomplete and connected by fontanels Fontanels – – Unossified remnants of fibrous membranes between fetal skull bones The four fontanels are anterior, posterior, mastoid, and sphenoid B. The appendicular skeleton includes the bones of the arms and legs and structures associated with them (shoulder, hip, wrist, ankle, fingers, toes). Upper Limb Lower Limb Classification of Bones: By Shape Long bones – longer than they are wide (e.g., humerus) Classification of Bones: By Shape Short bones – – Cube-shaped bones of the wrist and ankle Bones that form within tendons (e.g., patella) Classification of Bones: By Shape Flat bones – thin, flattened, and a bit curved (e.g., sternum, and most skull bones) Classification of Bones: By Shape Irregular bones – bones with complicated shapes (e.g., vertebrae and hip bones) Shapes of Bones Video Joints Chapter 8 C. Joints are where two or more bones meet. Joints (Articulations) Weakest parts of the skeleton Articulation – site where two or more bones meet Functions of joints – – Give the skeleton mobility Hold the skeleton together Classification of Joints: Structural Structural classification focuses on the material binding bones together and whether or not a joint cavity is present The three structural classifications are: – – – Fibrous Cartilaginous Synovial Classification of Joints: Functional Functional classification is based on the amount of movement allowed by the joint The three functional classes of joints are: – – – Synarthroses – immovable Amphiarthroses – slightly movable Diarthroses – freely movable Fibrous Structural Joints The bones are joined by fibrous tissues There is no joint cavity Most are immovable There are three types – sutures, syndesmoses, and gomphoses Fibrous Structural Joints: Sutures Occur between the bones of the skull Comprised of interlocking junctions completely filled with connective tissue fibers Bind bones tightly together, but allow for growth during youth In middle age, skull bones fuse and are called synostoses Fibrous Structural Joints: Sutures Fibrous Structural Joints: Syndesmoses Bones are connected by a fibrous tissue ligament Movement varies from immovable to slightly variable Examples include the connection between the tibia and fibula, and the radius and ulna Fibrous Structural Joints: Gomphoses The peg-in-socket fibrous joint between a tooth and its alveolar socket The fibrous connection is the periodontal ligament Cartilaginous Joints Articulating bones are united by cartilage Lack a joint cavity Two types – synchondroses and symphyses Cartilaginous Joints: Synchondroses A bar or plate of hyaline cartilage unites the bones All synchondroses are synarthrotic Examples include: – – Epiphyseal plates of children Joint between the costal cartilage of the first rib and the sternum Cartilaginous Joints: Symphyses Hyaline cartilage covers the articulating surface of the bone and is fused to an intervening pad of fibrocartilage Amphiarthrotic joints designed for strength and flexibility Examples include intervertebral joints and the pubic symphysis of the pelvis Synovial Joints Those joints in which the articulating bones are separated by a fluid-containing joint cavity All are freely movable diarthroses Examples – all limb joints, and most joints of the body Synovial Joints: General Structure Synovial joints all have the following – – – – – Articular cartilage Joint (synovial) cavity Articular capsule Synovial fluid Reinforcing ligaments Synovial Joints: Friction-Reducing Structures Bursae – flattened, fibrous sacs lined with synovial membranes and containing synovial fluid Common where ligaments, muscles, skin, tendons, or bones rub together Tendon sheath – elongated bursa that wraps completely around a tendon Synovial Joints: Movement The two muscle attachments across a joint are: – – Origin – attachment to the immovable bone Insertion – attachment to the movable bone Described as movement along transverse, frontal, or sagittal planes Synovial Joints: Range of Motion Nonaxial – slipping movements only Uniaxial – movement in one plane Biaxial – movement in two planes Multiaxial – movement in or around all three planes Gliding Movements One flat bone surface glides or slips over another similar surface Examples – intercarpal and intertarsal joints, and between the flat articular processes of the vertebrae Angular Movement Flexion — bending movement that decreases the angle of the joint Extension — reverse of flexion; joint angle is increased Dorsiflexion and plantar flexion — up and down movement of the foot Abduction — movement away from the midline Adduction — movement toward the midline Circumduction — movement describes a cone in space Gliding Movement Angular Movement: Flexion/Extension Hypertension/Flexion Dorsiflexion/Plantar flexion Abduction/Adduction/Circumduction Rotation Rotation The turning of a bone around its own long axis Examples – – Between first two vertebrae Hip and shoulder joints Special Movements Supination and pronation Inversion and eversion Protraction and retraction Elevation and depression Opposition Supination/Pronation Inversion/Eversion Protraction/Retraction Elevation/Depression Opposition Joints Video Hinge Joint: Hinge joints – – – – Cylindrical projections of one bone fits into a troughshaped surface on another Motion is along a single plane Uniaxial joints permit flexion and extension only Examples: elbow and interphalangeal joints Condyloid, or Ellipsoidal, Joints Oval articular surface of one bone fits into a complementary depression in another Both articular surfaces are oval Biaxial joints permit all angular motions Examples: radiocarpal (wrist) joints, and metacarpophalangeal (knuckle) joints Saddle Joint Condyloid, or Ellipsoidal, Joints Oval articular surface of one bone fits into a complementary depression in another Both articular surfaces are oval Biaxial joints permit all angular motions Examples: radiocarpal (wrist) joints, and metacarpophalangeal (knuckle) joints Ball and Socket Joint A spherical or hemispherical head of one bone articulates with a cuplike socket of another Multiaxial joints permit the most freely moving synovial joints Examples: shoulder and hip joints Gliding Joint Pivot Joint Rounded end of one bone protrudes into a “sleeve,” or ring, composed of bone (and possibly ligaments) of another Only uniaxial movement allowed Examples: joint between the axis and the dens, and the proximal radioulnar joint Synovial Joints: Knee Largest and most complex joint of the body Allows flexion, extension, and some rotation Three joints in one surrounded by a single joint cavity – – Femoropatellar Lateral and medial tibiofemoral joints Synovial Joints: Knee – Other Supporting Structures Anterior cruciate ligament Posterior cruciate ligament Medial meniscus (semilunar cartilage) Lateral meniscus Synovial Joints: Knee – Posterior Superficial View Adductor magnus tendon Articular capsule Oblique popliteal ligament Arcuate popliteal ligament Semimembranosus tendon Synovial Joints: Shoulder Stability Hip Elbow Bones and Cartilage Video Ligaments D. Ligaments are tough bands of connective tissue that attaches one bone to another. Tendons E. Bands of cartilage that binds muscle to bone. Bursae E. Bursae act to decrease friction and keep bones and tendons from rubbing against each other. Structure of Bone F. Anatomy of a bone: – 1. Compact bone a. Found in the middle of long bones Structure of Long Bone Long bones consist of a diaphysis and an epiphysis Diaphysis – – – Tubular shaft that forms the axis of long bones Composed of compact bone that surrounds the medullary cavity Yellow bone marrow (fat) is contained in the medullary cavity The medullary cavity is the space within the diaphysis. Structure of Long Bone Epiphyses – – – – Expanded ends of long bones Exterior is compact bone, and the interior is spongy bone Joint surface is covered with articular (hyaline) cartilage Epiphyseal line separates the diaphysis from the epiphyses Structure of Long Bone Bone Membranes Periosteum – doublelayered protective membrane – – – – Outer fibrous layer is dense regular connective tissue Inner osteogenic layer is composed of osteoblasts and osteoclasts Richly supplied with nerve fibers, blood, and lymphatic vessels, which enter the bone via nutrient foramina Secured to underlying bone by Sharpey’s fibers Endosteum – delicate membrane covering internal surfaces of bone Structure of Short, Irregular, and Flat Bones Thin plates of periosteum-covered compact bone on the outside with endosteum-covered spongy bone (diploë) on the inside Have no diaphysis or epiphyses Contain bone marrow between the trabeculae Structure of a Flat Bone Location of Hematopoietic Tissue (Red Marrow) In infants – Found in the medullary cavity and all areas of spongy bone In adults – Found in the diploë of flat bones, and the head of the femur and humerus Microscopic Structure of Bone: Compact Bone Haversian system, or osteon – the structural unit of compact bone – – – Lamella – weight-bearing, column-like matrix tubes composed mainly of collagen Haversian, or central canal – central channel containing blood vessels and nerves Volkmann’s canals – channels lying at right angles to the central canal, connecting blood and nerve supply of the periosteum to that of the Haversian canal Microscopic Bone Microscopic Structure of Bone: Compact Bone Osteocytes – mature bone cells Lacunae – small cavities in bone that contain osteocytes Canaliculi – hairlike canals that connect lacunae to each other and the central canal Microscopic Structure of Bone: Compact Bone – 2. Spongy bone a. Found at the ends of long bone Cartilage Video Chemical Composition of Bone: Organic Osteoblasts – bone-forming cells Osteocytes – mature bone cells Osteoclasts – large cells that resorb or break down bone matrix Osteoid – unmineralized bone matrix composed of proteoglycans, glycoproteins, and collagen Chemical Composition of Bone: Inorganic Hydroxyapatites, or mineral salts – – – Sixty-five percent of bone by mass Mainly calcium phosphates Responsible for bone hardness and its resistance to compression – 4. Your bones grow in length and diameter. a. Growth occurs are growth plate Bone Development Osteogenesis and ossification – the process of bone tissue formation, which leads to: – – – The formation of the bony skeleton in embryos Bone growth until early adulthood Bone thickness, remodeling, and repair How Bones Change Video Formation of the Bony Skeleton Begins at week 8 of embryo development Intramembranous ossification – bone develops from a fibrous membrane Endochondral ossification – bone forms by replacing hyaline cartilage Intramembranous Ossification Formation of most of the flat bones of the skull and the clavicles Fibrous connective tissue membranes are formed by mesenchymal cells Stages of Intramembranous Ossification An ossification center appears in the fibrous connective tissue membrane Bone matrix is secreted within the fibrous membrane Woven bone and periosteum form Bone collar of compact bone forms, and red marrow appears Stages of Intramembranous Ossification Stages of Intramembranous Ossification Stages of Intramembranous Ossification Stages of Intramembranous Ossification Endochondral Ossification Begins in the second month of development Uses hyaline cartilage “bones” as models for bone construction Requires breakdown of hyaline cartilage prior to ossification Stages of Endochondral Ossification Long Bone Growth and Remodeling Appositional Growth of Bone Importance of Ionic Calcium in the Body Calcium is necessary for: – – – – – Transmission of nerve impulses Muscle contraction Blood coagulation Secretion by glands and nerve cells Cell division Hormonal Mechanism Rising blood Ca2+ levels trigger the thyroid to release calcitonin Calcitonin stimulates calcium salt deposit in bone Falling blood Ca2+ levels signal the parathyroid glands to release PTH PTH signals osteoclasts to degrade bone matrix and release Ca2+ into the blood Hormonal Mechanism Importance of Ionic Calcium in the Body Calcium is necessary for: – – – – – Transmission of nerve impulses Muscle contraction Blood coagulation Secretion by glands and nerve cells Cell division Response to Mechanical Stress Wolff’s law – a bone grows or remodels in response to the forces or demands placed upon it Observations supporting Wolff’s law include – – Long bones are thickest midway along the shaft (where bending stress is greatest) Curved bones are thickest where they are most likely to buckle Bone Fractures (Breaks) Bone fractures are classified by: – – – – The position of the bone ends after fracture The completeness of the break The orientation of the bone to the long axis Whether or not the bones ends penetrate the skin Types of Bone Fractures Nondisplaced – bone ends retain their normal position Displaced – bone ends are out of normal alignment Complete – bone is broken all the way through Incomplete – bone is not broken all the way through Linear – the fracture is parallel to the long axis of the bone Types of Bone Fractures Transverse – the fracture is perpendicular to the long axis of the bone Compound (open) – bone ends penetrate the skin Simple (closed) – bone ends do not penetrate the skin Common Types of Fractures Comminuted – bone fragments into three or more pieces; common in the elderly Spiral – ragged break when bone is excessively twisted; common sports injury Depressed – broken bone portion pressed inward; typical skull fracture Compression – bone is crushed; common in porous bones Common Types of Fractures Epiphyseal – epiphysis separates from diaphysis along epiphyseal line; occurs where cartilage cells are dying Greenstick – incomplete fracture where one side of the bone breaks and the other side bends; common in children Stages in the Healing of a Bone Fracture Hematoma formation Torn blood vessels hemorrhage A mass of clotted blood (hematoma) forms at the fracture site Site becomes swollen, painful, and inflamed Stages in the Healing of a Bone Fracture Fibrocartilaginous callus forms Granulation tissue (soft callus) forms a few days after the fracture Capillaries grow into the tissue and phagocytic cells begin cleaning debris Bones produce blood cells in the red marrow. – a. Found in 1. 2. 3. 4. 5. 6. humerus femur sternum ribs vertebrae pelvis Stages in the Healing of a Bone Fracture The fibrocartilaginous callus forms when: – – – – Osteoblasts and fibroblasts migrate to the fracture and begin reconstructing the bone Fibroblasts secrete collagen fibers that connect broken bone ends Osteoblasts begin forming spongy bone Osteoblasts furthest from capillaries secrete an externally bulging cartilaginous matrix that later calcifies Stages in the Healing of a Bone Fracture Bony callus formation New bone trabeculae appear in the fibrocartilaginous callus Fibrocartilaginous callus converts into a bony (hard) callus Bone callus begins 3-4 weeks after injury, and continues until firm union is formed 2-3 months later Stages in the Healing of a Bone Fracture Stages in the Healing of a Bone Fracture Bone remodeling Excess material on the bone shaft exterior and in the medullary canal is removed Compact bone is laid down to reconstruct shaft walls Homeostatic Imbalances Osteomalacia – – – Bones are inadequately mineralized causing softened, weakened bones Main symptom is pain when weight is put on the affected bone Caused by insufficient calcium in the diet, or by vitamin D deficiency Homeostatic Imbalances Rickets – – – Bones of children are inadequately mineralized causing softened, weakened bones Bowed legs and deformities of the pelvis, skull, and rib cage are common Caused by insufficient calcium in the diet, or by vitamin D deficiency Homeostatic Imbalances Osteoporosis – – – – Group of diseases in which bone reabsorption outpaces bone deposit Spongy bone of the spine is most vulnerable Occurs most often in postmenopausal women Bones become so fragile that sneezing or stepping off a curb can cause fractures Osteoporosis: Treatment Calcium and vitamin D supplements Increased weight-bearing exercise Hormone (estrogen) replacement therapy (HRT) slows bone loss Natural progesterone cream prompts new bone growth Statins increase bone mineral density Paget’s Disease Characterized by excessive bone formation and breakdown Pagetic bone with an excessively high ratio of woven to compact bone is formed Pagetic bone, along with reduced mineralization, causes spotty weakening of bone Osteoclast activity wanes, but osteoblast activity continues to work Paget’s Disease Usually localized in the spine, pelvis, femur, and skull Unknown cause (possibly viral) Treatment includes the drugs Didronate and Fosamax Developmental Aspects of Bones Mesoderm gives rise to embryonic mesenchymal cells, which produce membranes and cartilages that form the embryonic skeleton The embryonic skeleton ossifies in a predictable timetable that allows fetal age to be easily determined from sonograms At birth, most long bones are well ossified (except for their epiphyses) Developmental Aspects of Bones By age 25, nearly all bones are completely ossified In old age, bone reabsorption predominates A single gene that codes for vitamin D docking determines both the tendency to accumulate bone mass early in life, and the risk for osteoporosis later in life – 6. Yellow bone marrow contains fat and is found in many bones. – 7. Bones store minerals. a. Calcium and phosphate needed to form strong bones. – 1. Found in: Milk Yogurt Cheese Lettuce Spinach Leafy vegetables Care – 8. Bones can become more brittle with age: osteoporosis. Caused by loss of bone volume and content. Quiz