principles of drug therapy in gastrointestinal diseases
advertisement
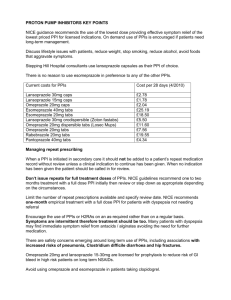
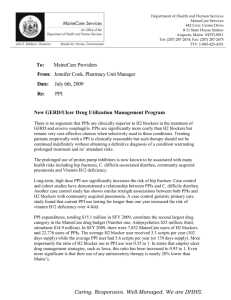
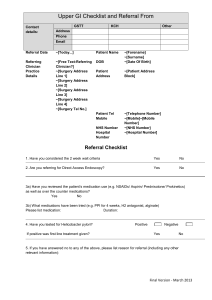
PRINCIPLES OF DRUG THERAPY IN GASTROINTESTINAL DISEASES Mohammad Minakari,MD,IUMS Dyspepsia • 25% ORGANIC • 75% FUNCTIONAL Organic Dyspepsia • • • • • • Peptic ulcer disease Gastroesophageal reflux Gastroesophageal malignancy Biliary pain Drug-induced dyspepsia Other causes Dyspepsia Indications for Testing and Treatment of Helicobacter pylori Infection Helicobacter pylori Eradication • Initial therapy: – Triple therapy: • proton pump inhibitor (PPI), amoxicillin (1 g twice daily), and clarithromycin (500 mg twice daily) for 7 to 14 days. • Metronidazole instead of amoxicillin • Increased ppi duration can increase eradication rate minimally • No ppi is better than the others for eradication Quadruple therapy • A PPI, combined with bismuth (525 mg four times daily) and two antibiotics (eg, metronidazole 250 mg four times daily and tetracycline 500 mg four times daily) given for 10 to 14 days. • In IRAN , quadruple therapy is preferred for initial therapy. Sequential therapy • Clarithromycin sequential therapy :Omeprazole (20 mg twice daily) and amoxicillin (1 g twice daily) for five days, followed by omeprazole (20 mg twice daily), clarithromycin (500 mg twice daily), and tinidazole (500 mg twice daily) for five or more days • Levofloxacin -250 sequential therapy :Omeprazole (20 mg twice daily) plus amoxicillin (1 g twice daily) for five days, followed by omeprazole (20 mg twice daily), levofloxacin (250 mg twice daily), and tinidazole (500 mg twice daily) for five or more days • Levofloxacin -500 sequential therapy :Omeprazole (20 mg twice daily) plus amoxicillin (1 g twice daily) for five days, followed by omeprazole (20 mg twice daily), levofloxacin (500 mg twice daily), and tinidazole (500 mg twice daily) for five or more days ERADICATION CONFIRMATION • Patients who have persistent symptoms after H. pylori treatment for dyspepsia • Patients who had an H. pylori associated ulcer • Patients who had gastric mucosa associated lymphoid tissue (MALT) lymphoma • Patients who had resection for early gastric cancer TREATMENT FAILURES • Clarithromycin should not be used unless resistance testing confirms the H. pylori strain is susceptible to the drug . • Antibiotics previously taken should generally be avoided. • Tetracycline may be more effective in this setting than metronidazole • A simpler treatment regimen could improve compliance and, as a result, efficacy. • levofloxacin or rifabutin or furazolidone can be considered Testing for resistance • Routine culture and testing for antibiotic susceptibility and resistance for H. pylori is not currently recommended. • Patients with refractory disease may require culture and sensitivity testing. SIDE EFFECTS • Are reported in up to 50 % of patients taking one of the triple therapy regimens . • The adverse effects are usually mild • Fewer than 10 % of patients stop treatment due to side effects. SIDE EFFECTS • Metronidazole :can cause a peripheral neuropathy, seizures, and a disulfiram-like reaction when taken with alcohol. • Clarithromycin can cause taste alteration, nausea, vomiting, abdominal pain, and rarely QT prolongation. • Tetracycline can induce a photosensitivity reaction in some cases. It should also not be administered to pregnant women or young children. • Amoxicillin can cause diarrhea or an allergic reaction with skin rash. FUNCTIONAL DYSPEPSIA • Presence of one or more of the following: postprandial fullness, early satiation, epigastric pain or burning and no evidence of structural disease (including at upper endoscopy) to explain the symptoms. • The criteria should be fulfilled for the last three months with symptom onset at least six months before diagnosis. TREATMENTS OTHER THAN ANTISECRETORY • • • • • • Antidepressants Prokinetic agents Fundic relaxant drugs Antinociceptive agents Psychological therapy Complementary and alternative medicine GERD ACID SUPPRESSIVE MEDICATIONS Over-the-counter antacids and/or H2 receptor blockers Prescription H2-blockers (twice daily) Intermittent (2 weeks) use of a PPI Omeprazole (20 mg daily) or equivalent dose of the other PPIs Omeprazole (20 mg twice daily or 40 mg daily) or equivalent doses of the other PPIs METHODS OF TREATMENT • STEP DOWN THERAPY: Rapid symptom removal Higher cost • STEP UP THERAPY: Slower symptom removal Lower cost ACID SUPPRESSIVE MEDICATIONS • The H2 receptor antagonists offer a therapeutic gain of 10 to 24 % relative to the placebo for healing esophagitis. • The PPIs are more effective in healing esophagitis than the H2 receptor antagonists. • PPIs lead to more rapid healing and symptom relief than H2 receptor antagonists • PPIs exhibit a dose-response curve for healing high-grade esophagitis as evidenced by higher healing rates with higher doses and/or more potent compounds unlike H2RA. Nonerosive gastroesophageal reflux disease • Esophageal hypersensitivity • Abnormal acid exposure but have not developed overt mucosal injury • Functional heartburn – The first two groups, but not the third group of patients, may respond to antisecretory therapy. – PH metry can help for differentiation WHAT PPI? • The difference between various PPIs is small and clinically non-significant • Esomeprazole is the most potent • Pantoprazole is the least interactive • Interaction with clopidogrel is an unresolved issue PPI DOSE SAFETY • Prolonged hypochlorhydria and hypergastrinemia • Possible association of PPIs with gastric atrophy SAFETY • a 2008 guideline on gastroesophageal reflux disease (GERD) management developed by the AGA found insufficient evidence to recommend for or against bone density studies, calcium supplementation, H. pylori screening, or any other routine precaution in patients taking proton pump inhibitors . • However, studies subsequent to that guideline continue to raise concerns about possible infectious complications, electrolyte disturbances, and metabolic bone disease associated with PPI use. Infections • Clostridium difficile and other enteric infections • Pneumonia : both community acquired pneumonia (CAP) and health care associated pneumonia (HCAP) Malabsorption • • • • Magnesium absorption Hip fracture and calcium malabsorption Vitamin B12 malabsorption Iron malabsorption Hypergastrinemia • Gastric carcinoid tumors in rats. • No dysplasia or neoplastic changes in patients treated with omeprazole for up to 11 years. • The clinical significance of other theoretical risks related to hypergastrinemia (such as colon cancer) has not been established. Atrophic gastritis/Gastric cancer • Not proven • Controversy about eradication of H.pylori • Most experts believe that it is unnecessary ADJUNCTIVE THERAPY • Prokinetic agents • Reflux inhibitors MAINTENANCE THERAPY • Maintenance acid suppressive therapy is often necessary • A trial off medications should be considered in all patients with gastroesophageal reflux disease (GERD) who have a good clinical response to acid suppression with the exception of those with severe esophagitis on upper endoscopy (Los Angeles classification Grade C and D) and Barrett’s esophagus MAINTENANCE THERAPY • Rapidity of recurrence : – less than three months: continuous therapy – more than three months : on demand therapy MAINTENANCE THERAPY • PPIs at a standard dose or a lower dose (usually one-half of the standard dose) were more effective than H2RAs in resolving GERD symptoms at four weeks and promoting healing esophagitis at eight weeks. • PPIs at a standard dose were more effective than a lower dose in preventing relapse of symptoms. • PPIs at a standard dose were more effective than PPIs at a lower dose in maintaining healing of esophagitis. ULCERATIVE COLITIS METHODS OF TREATMNT • Step-up • Step-down • Severity based Severity of UC GOALS OF MEDICAL Tx IN UC • • • • To induce remission To maintain remission To maintain adequate nutrition To minimize disease- and treatment-related complications • To improve the patient’s quality of life Induction of remission in UC CHOOSING MEDICATION 5-ASA ORAL 5-ASA 5-ASA • Are effective in remission induction in mild to moderate UC • Are effective in maintaining remission • Are usually safe and well tolerated • Are not effective in doses < 2 g/day • Have dose dependent response Side effects of sulfasalazine • Side effects of sulfasalazine • 15% of patients stop sulfasalazine intake due to adverse effects • 90% of them can tolerate other 5-ASAs Glucocorticoids • At doses equivalent to 40 to 60 mg/day of oral prednisone,glucocorticoids are effective first-line therapy for moderateor severe flares of UC. • The use of doses higher than60 mg/day is associated with increased side effects without appreciable clinical benefit and thus should be avoided. • The addition of sulfasalazine to corticosteroids in moderately to severely active UC does not offer any incremental benefit. Side Effects of Glucocorticoids Glucocorticoids • Should not be used for maintenance therapy • Should be tapered and discontinued in a few months Immunomodulators:Azathioprine and 6-Mercaptopurine • Probably effective in induction of remission • Need 2-3 months for appearance of benefits • Effective in maintaining remission AZA/6MP METABOLISM AZA/6MP • • • • AZA:2-3 mg/kg/day 6MP:1-1.5 mg/kg/day Leukopenia is not necessary for effectiveness Checking 6TG/6MMP is useful in nonresponders Cyclosporine • Cyclosporine A is a potent inhibitor of cellmediated immunity. • Its use in UC is primarily in patients with severe,steroid-refractory disease. • Intravenous cyclosporine 2-4 mg/kg • The addition of azathioprine or 6-MP in patients who have responded to intravenous cyclosporine reduces the rate of relapse or colectomy. SIDE EFFECTS OF CYCLOSPORINE SIDE EFFECTS OF CYCLOSPORINE • During intravenous therapy,cyclosporine levels should be monitored daily, and the dose should be adjusted to achieve a trough concentration (measured one hour before dosing) between 200 and 400 ng/mL,determined by high-pressure liquid chromatography. • Serum electrolytes and serum creatinine levels should be monitored daily or every other day. OTHER THERAPIES • • • • • Methotrexate Tacrolymus Probiotics/prebiotics/synbiotics Nicotine Heparin Anti-Tumor Necrosis Factor Antibodies INFLIXIMAB INDICATION • Patients with moderately to severely active UC who have had an inadequate response to conventional therapy. • Infliximab is now accepted as part of the standardtreatment options in patients with UC. DOSAGE • 5mg/kg IV infusion • 0,2,6 weeks ,then continue if there is clinical response,every 8 weeks MANAGEMENT OF MILD TO MODERATE UC MANAGEMENT OF MILD TO MODERATE UC Management of severely active ulcerative colitis. IMPORTANT POINTS • Empiric therapy(WITHOUT COLONOSCOPY) is not acceptable in patients who might have IBD. • Maintenance therapy is almost always needed in UC patients • IBS is not colitis! • IBD treatment is usually long term/lifetime,the patients must know it THANK YOU