Drugs used in Hypertension
advertisement

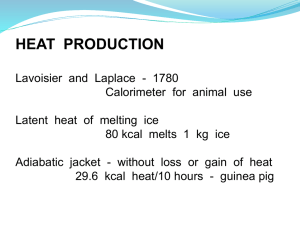
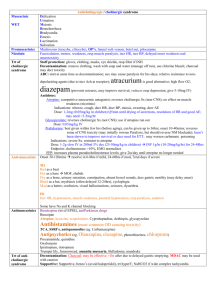
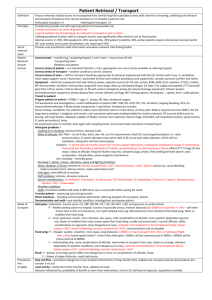
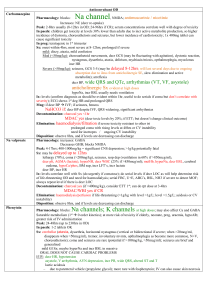
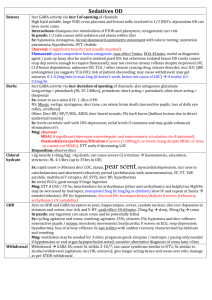
Drugs used in Hypertension This left ventricle is very thickened (slightly over 2 cm in thickness), but the rest of the heart is not greatly enlarged. This is typical for hypertensive heart disease. The hypertension creates a greater pressure load on the heart to induce the hypertrophy. The left ventricle is markedly thickened in this patient with severe hypertension that was untreated for many years. The myocardial fibers have undergone hypertrophy. See below Modulation of Renin Release Natriuretic Peptide and ADH Signaling Pathways Hypertension • High bp assoc with decr LE, stroke, CAD, and other end-organ diseases (e.g., retinopathy, renal failure). • Problem: Risk is graded. • Lowering the bp is indicated in patients if the diastole bp > 90 mm Hg and systole bp > 160 mm Hg. • Other risk factors for vascular disease may be synergistic: smoking, obesity, hyperlipidemia, DM and ventricular hypertrophy. • In cases of mild hypertension, weight loss, decr alcohol and salt may be sufficient, but… • In more severe cases, drug treatment is indicated. Drugs used for Hypertension • • • • • • β-adrenergic receptor antagonists Thiazide diuretics ACE inhibitors Ca2+ antagonists α 1-adrenergic receptor antagonists? Centrally acting drugs: α 2-adrenergic receptor agonists? • Moderate hypertention usually requires just one drug, but becoming incr more evident that >2 drugs will do the job better. Thiazide Diuretics • One of 2 1st-line of defense in treating hypertension • Mechanism of decr arterial bp – not known. • Initially, decr in blood vol, venous return, and cardiac output decr bp. • Gradually, the cardiac output returns to normal, but the hypotensive effect remains because the peripheral resistance has, in the meantime, decreased. • Diuretics have no direct effects on the vascular smooth muscle. • Rather, the small, but persistent decr in body Na+ decr in H2O decr bp. Thiazide Diuretics (cont’d) • One possible mech: decreased smooth muscle Na+ 2° decr in [Ca2+]cyto so that the muscle becomes less responsive. • These drugs may cause hypokalemia, DM, gout. • Side-effects: impotence, libido loss. • These drugs have a flat-dose response curve: **What does this mean, both response-wise and clinically? (possible exam question) β-Adrenoreceptor Antagonists • One of 2 1st-line of defense in treating hypertension. • Decr bp by decr cardiac output (CO). • With cont’d treatment, the CO returns to normal, but the bp remains low (not known how) because the peripheral vasc resistance is “reset” at a lower level. • Centrally acting mechanism? Not likely because some of these drugs do not cross the BBB. • Block of β1-adrenoreceptors in renal JG cells that secrete renin may be involved. • Adverse side-effects: cold hands, fatigue, asthma provocation, HF, or conductance block, incr serum TGs, and decr HDL levels. • All of these drugs decr bp, but at least some of these side-effects can be averted (cardioselective hydrophillic drugs (w/o liver metabolism or BBB penetration) (e.g., atenolol). Vasodilator Drugs – ACE Inhibitors • Recall angiotensin II – strong circulating vasoconstrictor. So, inhibiting its synthesis in hypertensive patients decr in peripheral resistance and bp. • ACEIs don’t impair CV reflexes and share few of the side-effects with diuretics and β-blockers. • Side-effects: incr bradykinin dry cough (ACE also metabolizes bradykinin); • More serious side effects: angioedema, proteinurea, neutropenia. • 1st dose may cause a very steep fall in bp (e.g., in patients on diuretics bec. they are Na+-depleted) • May cause renal failure in patients with bilateral renal artery stenosis: - Angiotensin II required to constrict postglomerular arterioles and maintain adequate GF. - Inhibition of angiotensin II formation does not seriously impair secretion and excessive K+ retention occurs only with K+ supplements or K-sparing diuretics (recall that aldosterone incr Na+ reabsorption and K+ excretion). Vasodilator Drugs – Angiotensin Receptor Antagonists • Losartan (e.g.) lowers bp by blocking angiotensin (AT1) receptors. • Similar properties to the ACEIs, but do not cause cough, because they do not prevent bradykinin metabolism. Vasodilator Drugs – Ca-Channel Blockers (Ca antagonists) • Vascular SM tone determined by [Ca2+]cyto. • Increased by α1-adrenoceptor activation (recall incr sympathetic tone?) that triggers Ca2+ release from the SR via ins-1,4,5-P3 (IP3) signaling. • Also, receptor-operated cation channels depolariation Ca2+ channels (L-type VG Ca2+ channels) more Ca2+ enters cell. • Nifedipine, amlopidine bind Ca2+ channels, block Ca2+ entry relaxation of arterial SM decr peripheral resistance and decr bp. • Efficacy similar to that of the thiazides, βblockers, and ACEIs • Side-effects: excessive vasodilation dizziness, headaches, hypotension, flushing, ankle edema. Vasodilator Drugs – α1-Adrenoreceptor Antagonists • Prazosin < doxazosin (longer-acting). • Selectively block vascular α1-adrenoceptors vasodilation. • Unlike non-selective α-blockers, these drugs not likely to cause tach, but may cause postural hypotension. • May be severe after 1st dose. Vasodilator Drugs – Hydrazine • Used in combination with a β-blocker and diuretic. • Side-effects: reflex tach, which may angina, headaches, fluid retention – (2° hyperaldosteronism). • In slow acetylators, hydrazine may produce lupus syndrome fever, arthralgia, malaise, and hepatitis. Vasodilator Drugs – Minoxidil • Potent vasodilator that severe fluid retention and edema. • But, when given with a β-blocker and loop diuretic, it is effective in severe hypertension resistant to other drug combinations. • Relaxes vascular SM cells by opening ATPsensitive K+ channels hyperpolarization and closing VG-Ca2+ channels. • [These K+ channels are normally kept closed by ATPintracell, which is antagonised by minoxidil Centrally-Acting Drugs • Methyldopa in adrenergic nerve endings to α-methylNE, which stimulates α2adrenoceptors in the medulla and decr sympathetic outflow. • Side-effect: drowsiness, hemoytic anemia. • Clonidine rebound hypertension if suddenly withdrawn. Acute Severe Hypertension • Hydralazine in hypertension assoc with eclampsia of pregnancy. • Nitroprusside in malignant hypertension with encephalopathy. Kidneys • Aldosterone stim Na+ reabsorption in the distal tubule and incr K+ and H+ secretion. • Cytoplasmic receptors. • Induces synthesis of the Na+/K+-ATPase in the basolateral membrane and Na+ channels in the luminal membrane. • Cell surface aldosterone receptors may mediate a more rapid incr in Na+ channel permeability. Kidneys (cont’d) • Diuretics increase the Na+ load in the distal tubules and incr K+ secretion and excretion (except for the K+sparing agents). • This effect is greater if [aldosterone]plasma are high (e.g., vigourous diuretic therapy has depleted the body of Na+ stores.) • Vasopressin (ADH) released from the Post Pit. • Incr the number of H2O channels in the collecting ducts passive reabsorption of H2O. • In cranial diabetes insipidus, absence of ADH large vols of hypotonic urine: treated with vasopressin (or desmopressin, a longer acting analogue) Diuretics – Drugs Acting on the Kidneys • Purpose: to incr the excretion of NaCl and H2O, normally controlled by aldosterone and vasopressin, respectively. • Most work by decr the reabsorption of electrolytes by the tubules. • Accompanied by an incr in H2O excretion so that osmotic balance is maintained. [recall that diuretics are used to decr edema in CHF]. But also used in some renal diseases and hepatic cirrhosis. • Some diuretics, esp thiazides, widely used in treating hypertension, but their long-term hypotension action is not only related to their diuretic properties. Thiazides • Developed from carbonic anhydrase inhibitors. • However, the diuretic effect of these drugs is not related to their actions on this enzyme. • Relatively safe, orally active, but relatively weak diuretics • Widely used for treatment for mild HF and hypertension (also decr incidence of stroke). • Many different thiazides exist, differing significantly only in their duration of action. • Bendoflumethiazide is widely used. Thiazides - Mechanism • Act mainly on the distal segments of tubules, where they inhibit NaCl reabsorption by binding to the symporter responsible for the electroneutral cotransport of Na+/Cl-. • incr excretion of Na+, Cl-, and H2O. • The increased Na+ in the distal tubule stim Na+ exchange with K+ and H+, increasing their excretion and hypokalema and metabolic acidosis. Thiazides – Adverse Effects • Hypokalemia may ppt cardiac arrhythmias, esp in patients on digitalis. Can be prevented by giving K supplements, or by combining therapy with K-sparing drugs. • Hyperuricaemia. Uric acidblood are often increased because thiazides are secreted by the organic acid secretory system in the tubules and compete for uric acid secretion. This may ppt gout. • Glc tolerance may be impaired and thiazides are contraindicated in patients with NIDD. • Lipids. Thiazides incr [cholesterol]plasma at least during the 1st 6 mos of administration, but the signif of this is uncertain. Loop Diuretics (LDs) (high ceiling) [Very Powerful] • More effective than the thiazides. • Act more rapidly, but shorter duration of action. • Ususally furosemide – used orally to decr peripheral and pulmonary edema in moderate and severe HF. • Given i.v. for pulmonary edema resulting from acute ventricular failure. • Effective in patients with decr renal function (unlike the thiazides). Loop Diuretics - Mechanism • Inhibit NaCl reaborption in the thick ascending loop of Henle. This segment has a high binding capacity for absorbing NaCl diuresis produced at this site is much greater than at other sites. Act on the luminal membrane where they inhibit the cotransport of Na+/K+/2Cl-. [Recall that the Na+ is actively transported out of the cells into the interstitium by an Na+/K+-ATPase-dependent pump at the basolateral membrane]. • Specificity of these drugs due to their high concentration in the renal tubules. • However, at higher doses, these drugs may induce changes in the electrolyte composition of the endolymph and cause deafness. Loop Diuretics – Adverse Effects • • • • Hyponatraemia Hypotension Hypovolemia Hypokalemia – may be unimportant unless there are additional risk factors for arrhythmia (e.g., digoxin). • Can cause severe electrolyte imbalance and dehydration. • Ca2+ and Mg2+ excretion often increased -> hypomagnesmia may occur. • Over-enthusiastic use (high doses, i.v.) can cause deafness, which may not be reversible. Loop Diuretics (cont’d) • Metalazone – thiazide-related drug with activity between that of the LDs and thiazides. • Synergistic with furosemide in treating resistant edema and serious renal failure. • Both thiazides and LDs incr K+ excretion. • So, K+ supplements may be required to prevent hypokalemia. K+-Sparing Diuretics (KSDs) • • • • • • • • • Weak when used alone. Given to retain K+. Often given with thiazides and LDs to prevent hypokalemia. Act on aldosterone-responsive segments of the distal nephron, where K+ homeostasis is controlled. Aldosterone stim Na+ reabsorption negative Ψ in the lumen, which drives K+ and H+ into the lumen (and hence their excretion). The KSDs decr Na+ reabsorption by either antagonizing aldosterone (spironolactone) or blocking Na+ channels (amiloride, triamterene). This causes the electrical Ψ across the tubular epithelium to fall, decreasing the driving force for K+ secretion. These drugs may cause severe hypokalemia, esp if renal impairment exists. Hypokalemia may also occur in the presence of ACEIs (e.g., catopril), because these drugs decr aldosterone secretion (and therefore K+ excretion). KSDs (cont’d) - Spironolactone • Competitively blocks the binding of aldosterone to its cytoplasmic receptor incr Na+ (Cl- and H2O) excretion and decr the ‘electrically coupled’ K+ secretion. • Weak diuretic (only ~2 % of the total Na+ reabsorption is under aldosterone control). • Used mainly in liver disease with ascites, Conn’s syndrome (1° hyperaldosteronism) and severe heart failure. KSDs (cont’d) – Amiloride and Triamterene • Decrease the luminal membrane Na+ permeability in the distal nephron by blocking Na+ channels on a 1:1 basis. • This increases Na+ (Cl- and H2O) excretion and decreases K+ excretion. Carbonic Anhydrase Inhibitors • Weak diuretics and rarely used for this purpose. • Osmotic diuretics (e.g., mannitol) are filtered, but not easily reabsorbed. • Excreted with an osmotic equivalent of H2O and are used in cerebral edema. • Depress bicarbonate reabsorption in the prox tubule by inhibiting the catalysis of CO2 hydration and dehydration reactions. • Thus, the excretion of HCO3-, Na+, and H2O are increased. • The loss of HCO3- metabolic acidosis the effects of the drug becomes self-limiting as the [HCO3-]blood falls. • The incr Na+ delivery to the distal nephron incr K+ secretion. • Acetazolamide used to treat glaucoma to decr intraocular P (decr the secretion of HCO3- and assoc H2O into the AH. Nephron anatomy and the site of action of Diuretics Proximal Convoluted Tubule Cell – Note the Action of acetazolamide Logical Combinations Diuretic b-blocker CCB Diuretic - - b-blocker - * - CCB - - ACE inhibitor - - a-blocker - * * Verapamil + beta-blocker = absolute contra-indication ACE inhibitor a-blocker Compelling and possible indications and contrindications for the major classes of antihypertensive drugs INDICATIONS CONTRAINDICATIONS CLASSS OF DRUG COMPELLING POSSIBLE POSSIBLE COMPELLING a-blockers Prostatism Dyslipidaemia Postural Hypotension Unrinary incontinence Angiotensin converting enzyme (ACE) inhibitors Heart failure Left ventricular dysfunction Chronic renal disease * Type II diabetic nephropathy Renal impairment * Peripheral vascular disease † Pregnancy Renovascular disease Angiotensin II receptor antagonists Cough induced by ACE inhibitor ‡ Heart failure Intolerance of other antihypertensive drugs Peripheral vascular disease Pregnancy Renovascular disease Myocardial infarction Heart failure b-blockers Angina Heart failure Dyslipidaemia Peripheral vascular disease Calcium antagonists (dihydropyridine) Isolated systolic hypertension (ISH) in elderly patients Angina Elderly patients Calcium antagonists (rate limiting) Angina Myocardial infarction Thiazides Elderly patients including ISH _ _ Asthma or COPD Heart block _ Combination with b-blockade Heart block Heart failure Dyslipidaemia Gout * ACE inhibitors may be beneficial in chronic renal failure but should be used with caution. Close supervision and specialist advice are needed when there is established and significant renal impairment † Caution with ACE inhibitors and angiotensin II receptor antagonists in peripheral vascular disease because of association ‡ If ACE inhibitor indicated f b-blockers may worsen heart failure, but in specialist hands may be used to treat heart failure with renovascular disease.