Dialectical Behavior Therapy (DBT)
advertisement
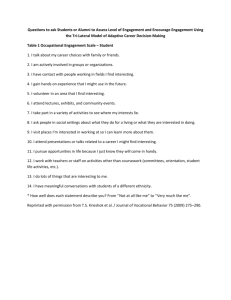
DBT for Substance Abuse: A New Approach to Helping Clients Struggling with BPD and Addictions October 28, 2015 Alina Gorgorian, Ph.D. Michael Roy, LCSW Clearview Women’s Center Los Angeles, Calif. © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Why are we here? More BPD and substance abuse than BPD or substance abuse In substance abuse programs: In studies between 1986 and 1997, among patients seeking treatment for substance abuse disorders, 5-65% have also had BPD dx (Trull et al., 2000) Among 615 heroin users documented in Sydney Austrailia, 42% also had BPD (Drake et al., 2004) © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Why are we here? Among BPD samples: In studies between 1986 and 1997, among pts receiving tx for BPD, SUDs ranged from 26-84% (Trull et. Al., 2000 © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Implications of Comorbidity • Severe psychopathology predict poorer outcomes and early relapse among drug abusers • Patients with severe psychopathology are screened out of tx outcome studies • Suicide attempts are highest for individuals with both BPD and SUDs (Rossow and Lauritzen, 1999) • Co-occurrence of an SUD and BPD was the factor most closely associated with poor tx outcomes (Zanarini et al. 2004) © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Who Is DBT for? • Severe, chronic, multi-diagnosed, “difficult to treat” patients • Axis I and II patients – BPD – Substance Abuse – Eating Disorders © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. DBT vs. TAU • With DBT – Fewer drop out – Less drug use – Greater global adjustment – Greater social adjustment – DBT gains continued at follow-up © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Borderline Personality Disorder • A pervasive disorder of the emotion regulation system • Criterion behaviors function to regulate emotions or are a natural consequence of emotion dysregulation © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. DSM 5 Criteria for BPD At least 5 . . . 1. Frantic efforts to avoid real or imagined abandonment 2. A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation 3. Identity disturbance: markedly and persistently unstable self-image or sense of self 4. Impulsivity in at least two areas that are potentially self-damaging 5. Recurrent suicidal behavior, gestures, or threats, or self-mutilating behavior 6. Affective instability due to a marked reactivity of mood 7. Chronic feelings of emptiness 8. Inappropriate, intense anger or difficulty controlling anger 9. Transient, stress-related paranoid ideation or severe dissociative symptoms © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Criteria Reorganized • Emotional Dysregulation – Mood swings – Intense anger/rage • Interpersonal Dysregulation – Interpersonal chaos – Fear of being abandoned • Self Dysregulation – Struggle with identity and sense of self – Feelings of emptiness • Behavioral Dysregulation – Self-injury – Suicidality – Impulsivity • Cognitive Dysregulation – Dissociation – Paranoia – Obsessions Linehan, 1993 © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Biosocial Model of BPD Biological Dysfunction in Emotion Regulation System Pervasive Emotion Dysregulation Invalidating Environment 10 EMOTION DYSREGULATION EMOTIONAL VULNERABILITY INABILITY TO MODULATE EMOTIONS 11 Emotional Vulnerability • High sensitivity – Immediate reactions – Low threshold for emotional reaction • High reactivity – Extreme reactions – High arousal dysregulates cognitive processing • Slow return to baseline – Long-lasting reactions – Contributes to high sensitivity to next emotional stimulus Linehan, 1993 © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. The “Social” Part: Invalidating Environments • Behaviors and communication of private experiences are pervasively rejected as invalid. • Emotional displays are met by punishment; escalation is met by erratic, intermittent reinforcement. • Problem-solving is oversimplified. © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Consequences of Chronic Invalidation • Environment fails to teach individual to: – Effectively label private experiences – Effectively regulate emotions – Trust experiences as valid responses to events (gut instinct) • Instead, environment teaches individual to: – Self-invalidate and search environment for cues about how to respond © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. DBT aims to modulate emotions by… • Decreasing (or increasing) physiological arousal associated with emotion • Re-orienting attention • Inhibiting mood-dependent behaviors • Experiencing emotions without escalating or blunting • Organizing behavior in the service of non-mood dependent goals (i.e., opposite action) Linehan, 1993 © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Assumptions about the patient • Patients are doing the best they can • Patients want to improve • Patients need to do better, try harder, and be more motivated • Patients may not have caused all their own problems, but they have to solve them anyway • The lives of suicidal, borderline individuals are unbearable as they are currently being lived • Patients must learn new behaviors in all relevant contexts • Patients can not fail in DBT Linehan, 1993 © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Assumptions about therapy • The most caring thing a therapist can do is help patients change in ways that bring them closer to their own ultimate goals • Clarity, precision, and compassion are of the utmost importance in the conduct of DBT • The therapeutic relationship is a real relationship between equals • Principles of behavior are universal, affecting therapists no less than patients • Therapists treating borderline patients need support • DBT therapists can fail • DBT therapy can fail even when therapists do not Linehan, 1993 © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Standard Modes of Therapy • • • • • Outpatient Individual Session Outpatient Skills Training Class Phone Coaching Consultation Team Ancillary Treatments – Pharmacotherapy – Acute inpatient psychiatric © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Responsibilities of Individual Therapist • • • • Treatment planning Integrating all modes of therapy Consulting to client Managing crises and life-threatening behaviors © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. But first… Pre-treatment 1. Agreement on Goals a) To stop using drugs now. Get a verbal commitment. 2. Agreement to Recommended Treatment a) Patient agreement b) Therapist agreements 3. Agreement to therapist-client relationship © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. First Four Sessions • Get client’s goals – Orient to the overarching goals of DBT: Building a life worth living • Get history of suicidal and substance use – assess current risk • Help client prepare for the difficulty of stopping problem behaviors • Look for positives © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. First Four Sessions • Orient to structure of program • Orient to protocols – 24-hour rule – 4 miss rule • Review – Diary card – Dialectics in DBT – Imminent Risk Assessment and Treatment Plan if needed – Biosocial Theory of BPD © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. First Session 1. Assess client’s – History – Current problems – Reason for coming to tx 2. Get their goals – Weave DBT targets into their goals 3. Get commitment to – Stop life-threatening behaviors – Participate in all sessions, UAs 4. Caution them about – Butterfly syndrome – Replacement meds and taper © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Stage 1 Primary Targets: Severe Behavioral Dyscontrol Behavioral Control •Decrease – Life-threatening behaviors – Therapy-interfering behaviors – Quality of life-interfering behaviors •Increase – Mindfulness – Distress tolerance – Interpersonal effectiveness – Emotion dysregulation – Self-management Linehan, 1993 © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Core Theories in DBT 1. Behavioral Science 2. Zen Practice 3. Dialectical Philosophy 25 Behaviorism: Chain-Analysis Excellent tool to identify key areas to be worked on Identify… • Prompting Event • Vulnerabilities • Cognitions • Emotions • Behaviors • Body Sensations • Problem Behavior • Consequences © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Chain Analysis Vulnerability Problem Behavio r Prompting Event Links Consequences Linehan, 1993 © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Solution Analysis Identify what needs to be done at each point on the chain to prevent the problem behavior from recurring • • • • • • • • Prompting Event Vulnerabilities Cognitions Emotions Behaviors Body Sensations Problem Behavior Consequences © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Problem Solving Vulnerability Effective Behavior Consequences Problem Behavior Prompting Event Links Consequences Linehan, 1993 © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Diary Cards • Provides a general overview of client’s week • Reduces risk of overlooking target behaviors • Keeps more accurate record of client’s daily emotions and behaviors • Enables client and therapist to perceive potential links between emotions © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Zen Practice • Contemplative practice, not a religion • Mindfulness – acceptance of the moment – Change requires acceptance – Acceptance of one set of problems to work on identified problems – Radical acceptance of the pat and limitations of the future 31 Dialectical Approach Balancing change/problem-solving and acceptance/validation Eliminating painful events with accepting painful events © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Dialectics: Find Balance Between • • • • Skill enhancement vs. Self-acceptance Problem solving vs. Problem acceptance Affect regulation vs. Affect tolerance Self-efficacy vs. Help-seeking © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. What Is Validation? “The action of validating or making valid…a strengthening reinforcement, confirming; establishing or ratifying as valid” • • • • • To Confirm To Authenticate To Corroborate To Substantiate To Verify © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Why Add Validation? Self-Verification Theory: people want to be known and understood by others according to their firmly held beliefs and feelings about themselves, that is self-views • Validation = Self-verification • Invalidation Arousal; sense of out-of-control • Arousal + Out-of-control Inability to process new information • Failure to process new info = no new learning © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. What Should we Validate? • • • • • • • Importance of a problem Emotional pain Difficulty of change Sense of out-of-control Dysregulation Inner strength and capabilities Behavior – Emotions, pain, and suffering – Physiological responses – Cognitive appraisals, thoughts, beliefs, and values – Actions © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Phone Coaching • If patient calls individual therapist: – Decrease crisis behaviors – Increase generalization of DBT behavioral skills – Decrease sense of conflict, alienation, distance with therapist © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Polarities in Substance Abuse Tx Abstinence only model Vs. Harm-reduction model © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Zen Practice: States of Mind Emotional Mind Wise Mind Reasonable Mind Linehan, 1993 © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. DBT-SUD Path to Clear Mind Clean Mind Clear Mind Addict Mind Linehan, 1993 © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Path to Clear Mind Decrease substance use Decrease physical discomfort from abstaining Decrease urges and cravings to use drugs Decrease options, contacts, and cues to use drugs Decrease capitulation to use drugs Increase community reinforcement of clear mind behaviors © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Decrease Physical Discomfort: Pain Management • Rationale: • Reduce risk of early termination • Prevent drug use • How: • Replacement meds • DBT skills, including distress tolerance, mindfulness, and PLEASE skills © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Decrease Urges and Cravings • Mindfully self-monitor urges (diary cards) • Normalize presence of urges (didactic strategy) • Label urges and detach from them (observe & describe skills) • Develop and use imagery • Urge surfing © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Didactic on Urges • Urges are episodic and not constant; they come and go • Urges may fluctuate in intensity during an episode and do not, by themselves, predict lapse • Urges do not decrease dramatically upon cessation, but gradually decrease over time (so long as they’re not reinforced) © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Decrease the options, contacts, and cues to use drugs • Target all overt and covert behaviors that maintain possibilities for drug use • Change phone numbers • Get rid of drugs, paraphernalia, and drug contacts • Move away • No stealing, lying, selling drugs • Making public commitment not to use © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Increase Community Reinforcement “Clear Mind” Behaviors • • • • Working for pay Socializing with non-drug addicts Joining groups where non-addicts go Becoming involved in and participating in AA/NA © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Finding your patients when they’re lost: Attachment Strategies 1. 2. 3. 4. 5. 6. 7. 8. 9. Orient client to attachment problem Increase contact during initial trimester Contact using VM Conduct therapy in vivo Shorten or lengthen sessions Conduct supportive family and friends network meetings Phone to break avoidance Find clients when they’re lost – utilize worksheet Give replacement medications © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Family Work • Utilize families as agents of change – Skills – Contingency management • Utilize families as agents of validation • Families striking dialectical balance © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Additional Skills BEHAVIORS TO INCREASE Mindfulness Skills BEHAVIORS TO DECREASE • Identity confusion • Emptiness • Cognitive dysregulation Interpersonal Skills • • • • • • • Emotion Regulation Skills Distress Tolerance Skills Interpersonal chaos Fears of abandonment Labile affect Excessive anger Impulsive behaviors Suicidal threats Self-harm © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission. Recommended Readings Dimeff, L. (n.d.). Dialectical behavior therapy in clinical practice: Applications across disorders and settings. Koerner, K. (2012). Doing dialectical behavior therapy: A practical guide. New York: Guilford Press. Linehan, M. (1993). Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press. Linehan, M. (2014). DBT Skills Training Manual (2nd ed.). Guilford Press. Linehan, M. (1993). Skills training manual for treating borderline personality disorder. New York: Guilford Press. © 2013 Clearview Treatment Programs. Not to be reprinted or reused without permission.