Pathophysiology of Complications of Diabetes
advertisement

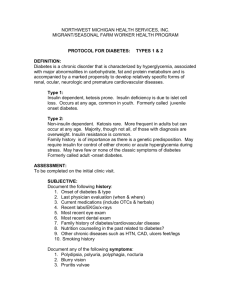
Complications of Diabetes: An Overview of the Pathophysiology Megha Poddar PGY - 4 Endocrinology 10/2013 OBJECTIVES 1. To understand the pathophysiology of acute complications of DM due to: • Diabetic Ketoacidosis • Hyperosmolar state 2. To understand the pathophysiology of chronic complications of DM due to hyperglycemia (micro vascular and macro vascular complications) 3. To gain an understanding of the mechanisms that lead to glucose induced vascular damage. Diabetes • Group of metabolic disorders that share a common feature of HYPERGLYCEMIA • Type 1 DM: absolute deficiency of insulin cause by beta cell destruction • Type 2 DM: combination of peripheral resistance to insulin action and inadequate secretory response • Results from defects in Insulin secretion, action or most commonly both • Leading cause of end stage renal disease, adult onset blindness and non traumatic lower extremity amputation Pathogenesis of Type 1 DM • Lack of insulin is caused by an immunologically mediated destruction of the beta cells • Genetic susceptibility: multiple loci are associated, most commonly MHC class II • The autoimmune insult is chronic by the time the patients first presents, 80-90% b cell destruction has already occurred Development of Type 1 Diabetes Pathogenesis of Type 2 DM • Environmental factors play a large role (lifestyle, dietary habits etc.) • Twin-twin concordance shows a stronger genetic relationship than DM2 • 2 Metabolic defects • Decreased ability of peripheral tissues to respond to insulin • b-cell dysfunction that is manifested as impaired insulin secretion Development of Type 2 Diabetes Complications of Diabetes Though the pathogenesis of DM differs, the complications are the same and are the main cause of mortality and morbidity Acute complications due to hyperglycemia • Diabetic ketoacidosis • HHS Chronic complications due to vascular damage • Microvascular complications: • Neuropathy, Nephropathy, Retinopathy • Macrovascular complications: • Coronary artery disease, peripheral vascular disease, stroke Diabetic Ketoacidosis • MEDICAL EMERGENCY!!! • Due to lack of insulin • Most often seen in Type 1 DM but also can be present in Type 2 DM who have predominantly secretory defects • Common in younger patients (<65), Women>Men • Mortality 5% • Most often due to the underlying illness and not the metabolic complications Hyperosmolar Hyperglycemic State • Less common than DKA • Seen in Type 2 DM • Age group is often older (>65 years) • Mortality 5-20%! • Often present with altered level of consciousness due to hyperosmolar state (when sOsm > 300mosm/kg) HHS • Hyperglycemia, hyper osmolality and dehydration without ketosis • Most frequent precipitants: • Acute Stressors (5 I’s) • Renal Failure • Hyperglycemic inducing medications Precipitating Factors • Acute stressors or illness increase the secretion of glucagon, cortisol and epinephrine precipitating hyperglycemia • 5 I’s: • • • • • Infection Infarction Insulin (compliance/omission) Ischemia Intoxication (alcohol, drug abuse) Regulatory Hormones • 2 main hormones responsible to hyperglycemia and ketoacidosis • Insulin - deficiency or resistance • Glucagon - excess Normal Response • Glucose is ingested during a meal, stimulates the release of Insulin from b-cells of the pancreas • Insulin action is to restore normoglycemia: • • • • Decreasing hepatic glucose production Inhibiting glycogenolysis and gluconeogensis Increases the skeletal muscle and adipose tissue uptake Inhibits glucagon secretion and production Hyperglycemia • Overall net reduction in effective circulation insulin with a net increase in counter regulatory hormones (epinephrine, cortisol, glucagon) • Hyperglycemia is due to: • Impaired peripheral utilization in tissue (post prandial) • Increased gluconeogenesis (fasting state) • Insulin deficiency is more prominent in DKA over HHS • HHS ketoacidosis is not seen • Glucose levels are much higher in HHS than in DKA Ketoacidosis • Insulin deficiency results in loss of uptake of glucose by peripheral glucose transporters Hyperglycemia • Insulin deficiency activates hormone dependent lipase Increased lipolysis (unregulated) • This leads to conversion of triglycerides to free fatty acids and glycerol Fatty acids are converted to acetyl CoA which is shuttled into 1) Krebs cycle (insulin dependent) 2) Ketones bodies (without insulin) including BHB and acetoacetate. Ketoacidosis • Inadequate insulin leads to energy stores from fat and muscle to be broken down into fatty acids and amino acids • These precursors are transported to the liver for conversion to glucose and ketones Diagnostic criteria for diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) Pathophysiology of Chronic Complications Macrovascular Complications • Main cause of mortality • large and medium vessel disease due to accelerated atherosclerosis Microvascular Complications • Significant source disability and decrease in quality of life • Capillary dysfunction in target organs Macrovascular Complications • Coronary Artery Disease • 2-4 times increased risk compared to general population • Greater incidence of “Silent MI” • Likely due to sensory neuropathy • May present as CHF • Peripheral Vascular Disease • Cerebrovascular disease Microvascular Complications • Retinopathy • Neuropathy • Nephropathy Retinopathy • Diabetes is the most common cause of blindness in the US • Retinopathy has the highest correlation with severity and duration of diabetes • Hyperglycemia is the primary cause of diabetic retinopathy but the specific pathophysiologic mechanisms are not well understood. • thought to be death of microvascular contractile cells (pericytes) and the loss of intracellular contacts which leads to microaneurysms and leakage. • Growth factors have been implicated in the development of the next phase - proliferative retinopathy. • Vascular Endothelium Growth Factor (VGEF) Classification of Diabetic Retinopathy • Pre proliferative • • • • • • increased vascular permeability venous dilation Microaneurysms intraretinal hemorrhage Fluid leakage Retinal ischemia. • Proliferative • Neovascularization • Vitreous hemorrhage • Fibrous proliferation (scarring). Nephropathy • Both the DCCT and the UKPDS showed that near euglycemia can decrease the development of microalbuminuria and progression of diabetic nephropathy. • However, tight glycemic control has no effect in reducing proteinuria or improving GFR if clinical nephropathy is present. • Early recognition of nephropathy is crucial Neuropathy • Diabetic neuropathy can present as mononeuropathy or polyneuropathy and can also be divided in sensory, motor and autonomic. • The pathogenesis is not well elucidated, but it is believed that the mononeuropathies, such as the acute cranial nerve palsies and diabetic amyotrophy, are due to ischemic infarction of the peripheral nerves. • The peripheral sensori-motor neuropathies and autonomic neuropathies may be caused by a metabolic factor or osmotic toxicity secondary to hyperglycemia. Hyperglycemia Induced Complications • Many proposed mechanisms of vascular damage from hyperglycemia • • • • Aldose reductase pathway Reactive Oxygen Species Advanced Glycation Endproducts theory Protein Kinase Theory Aldose reductase pathway • Certain cells are unable to regulate glucose uptake in hyperglycemic states (ex. Endothelial cells) • In a hyperglycemic state glucose is metabolized intracellularly by an enzyme aldose reductase into sorbitol and eventually into fructose • Intracellular NADPH is used as a cofactor in the pathway but is also used to regenerate glutathione • Glutathione is an antioxidant which prevent which decreases cellular susceptibility to oxidative stress Aldose Reductase Pathway Reactive Oxygen Species • The depletion of NADPH by aldose reductase leads to inability to regenerate GSH leading to oxidative stress reactions and cell death • Increased Sorbitol causes a decrease in nitric oxide – vasoconstriction in neuronal tissue and eventually ischemia Advanced Glycation End products theory • AGE’s are formed from nonenzymatic reactions between high levels of intracellular glucose, defects in the glucose metabolism pathway due to reactive oxygen species and build up of precursors • AGE’s effect extracellular matrix (collagen, laminin) – causes cross link between polypeptides and abnormal matrix and interrupts normal cell interactions • Ex: cross linking type 1 collagen in large vessels may lead to increase endothelial injury and atherosclerotic plaque build up • Ex: Cross linking type IV collagen in basement membrane decreases endothelial adhesion and increases fluid filtration AGE effects on Protein • AGE’s cross link proteins – causing them to be resistant to degradation • Increases protein deposition • Plasma proteins may bind to glycated basement membrane – may cause increased basement membrane thickness seen in nephropathy • proteins bind to AGE receptors and activate nuclear transcription of NF-Kb, cytokines, inflammatory markers Advanced glycation products in vascular pathology. Advanced glycation products in nephropathy Advanced glycation products are metabolized to small peptides Goh S , Cooper M E JCEM 2008;93:1143-1152 ©2008 by Endocrine Society Biological effects of Activating AGE receptors • Release cytokines and growth factors from macrophages (VEGF, IGF-1) • Increases endothelial permeability • Increases procoagulant activity • Enhances proliferation of synthesis of extracellular matrix by fibroblasts and smooth muscle cells Protein Kinase Theory • Activating PKC and DAG pathway by calcium ion is an important signalling pathway for many intracellular systems • Hyperglycemia stimulates the DeNovo synthesis of DAG and causes unregulated activation of PKC Effects of PKC activation • Production of VEGF – proangiogenic, implicated in neovascularization in retinopathy • Increased vasoconstrictor endothelin-1 and decreased vasodilator NOsynthetase • Production of profibrogenic molecules- leading to deposition of extracellular matrix • Procoagulant molecule plasminogen activator inhibitor -1 – leading to fibrinolysis and possible vaso-occlusive episodes • Production of pro-inflammatory cytokines Pathways of micro vascular complications initiated by hyperglycemia. AGEs, advanced glycation end products; DAG, diacylglycerol; PKC, protein kinase C. Hyperglycemia-induced production of superoxide by the mitochondrial electron transport chain. Hyperglycemic damage by inhibiting NAPDH. From Brownlee M: Biochemistry and molecular cell biology of diabetic complications. Nature 414:813–820, 2001. Effects of glycemic control on microvascular complications • The importance of tight glycemic control for protection against micro vascular disease in diabetes was established in the DCCT/EDIC study for type 1 diabetes • Reduction (42% in any cardiovascular event), decrease in LDL • Coronary calcification and carotid intimal thickness (measures of atherosclerosis were reduced in the IT group) • Nephropathy/albuminuria was related to higher rates of cardiovascular event • The role of glycemic control on micro vascular disease in type 2 diabetes was documented in the United Kingdom Prospective Diabetes Study (UKPDS), its role in reducing cardiovascular risk has not been established as clearly for type 2 diabetes. Pathogenesis Diabetic macrovascular disease? • In contrast to diabetic microvascular disease, data from the UKPDS have shown that hyperglycemia is not the major determinant of diabetic macrovascular disease. • Consequence of insulin resistance is increased free fatty acid (FFA) flux from adipocytes leading to plaque deposition in arterial endothelial cells. • In macrovascular, but not in microvascular endothelial cells, this increased flux results in increased FFA oxidation by the mitochondria. ? Similar Mechanism • Oxidation of fatty acids and FFA-derived acetyl CoA generate the same electron donors (NADH and FADH2) • Hypothesized that the increased FFA oxidation causes mitochondrial overproduction of ROS by the same mechanism described for hyperglycemia. • In addition to hyperglycemia FFA-induced increase in ROS activates the same damaging pathways: AGEs, PKC, Aldose pathway Insulin resistance causes mitochondrial overproduction of ROS in macrovascular endothelial cells by increasing FFA flux and oxidation. Glycemic control and vascular complications in DM • Hyperglycemia is an important risk factor for the development of micro vascular disease in patients with type 2 diabetes, as it is in patients with type 1 diabetes • Many trials have shown microvascular benefit with intensive glycemic control • • • • DCCT/EDIC UKPDS Advance/Accord VADT ADVANCE • 5571 type 2 diabetes patients receiving intensive therapy to lower A1C (mean A1C 6.5 percent) • Reduction in the incidence of nephropathy and the need for renal-replacement therapy or death due to renal disease compared with patients receiving standard therapy (A1C 7.3 percent) • There was no significant effect of glycemic control on the incidence of retinopathy. ACCORD trial • 10,250 patients with long-standing type 2 diabetes were assigned to intensive or standard glycemic control. (follow-up of 3.7 years) • Intensive therapy was stopped due to a higher number of total and cardiovascular deaths in subjects assigned to intensive therapy (median A1C 6.4%) compared with the standard treatment group (median A1C 7.5%). Veteran's Affairs Diabetes Trial (VADT) • 892 veterans with long-standing type 2 diabetes receiving intensive therapy (A1C 6.9 percent) • Did not have a reduction in retinopathy or major nephropathy outcomes, which were predefined secondary endpoints, compared with 899 veterans receiving standard therapy (A1C 8.4 percent) • Perhaps due to patients with longer history of diabetes (>10 yrs versus newly diagnosed in UKPDS) • Aggressive treatment of hypertension and hyperlipidemia in all VADT participants may have contributed to the inability to show a microvascular benefit of intensive glucose control Micro vascular summary: • The results of the UKPDS, ADVANCE and ACCORD trials are consistent with those of the DCCT for patients with type 1 diabetes, taking into account the relative differences in A1C achieved between treatment groups and the differences in study duration (or exposure): intensive therapy improves the outcome of micro vascular disease. • The results of the post-trial monitoring phase of the UKPDS show that a sustained period of glycemic control in newly diagnosed patients with type 2 diabetes has lasting benefit in reducing micro vascular disease. • Despite these differences, all three trials consistently show that over the time period studied (3.5 to 6 years), near-normal glycemic control (A1C 6.4 to 6.9 percent) does not reduce cardiovascular events in patients with longstanding diabetes. • However, in patients with newly diagnosed type 2 diabetes, a goal A1C of ≤7.0 percent is reasonable and supported by the findings of the UKPDS follow-up study. Macrovascular summary: • Epidemiological studies suggest correlation between DM and cardiovascular events • RCTs have not been able to prove this association, ACCORD showed increased risk in intensive group • May be due to variety of factors with study design (A1C targets, intensive regimen, number of hypoglycemic events) Reducing risk factors has been shown to decrease cardiovascular events • • • • Aggressive hypertension management Achieving dyslipidemia targets Smoking cessation Secondary Risk Factor reduction Thank You! References 1. Uptodate 2. Robbins and Cotran Pathologic Bases of Disease – Kumar,Abbas,Fausto 3. http://www.nature.com/nrm/journal/v9/n3/fig_t ab/nrm2327_F1.html 4. http://ocw.tufts.edu/Content/14/lecturenotes/266 734