Management of diabetes in the dialysis patient
advertisement
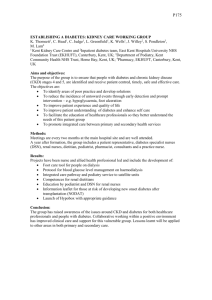
Management of diabetes in the dialysis patient Lyn Allen, Clinical Facilitator, Royal Derby Hospital Diabetes mellitus is one of the major causes of CKD ; these patients have a higher incidence of co-morbidities, particularly cardiovascular disease, tend to be older, and have an increased risk of hospitalisation, all which may have an effect when patients commence renal replacement therapy. Whilst the complications of diabetes in the context of haemodialysis is complex, it is thought that good glycaemic control and management of these complications, along with early detection, leads to the best possible outcomes. Management of the diabetes and haemodialysis treatment as one entity, rather than 2 separate issues is recommended, forging better links between renal and diabetes specialist teams, so that the patient receives as near as possible seamless care. Minimising the impact of the disease on the patient’s lifestyle is also important, which renal nurses being taught to monitor patients for the complications of diabetes whilst the patient is receiving dialysis, will minimise the number of additional hospital visits that patients have to attend. Peritoneal dialysis is associated with negative factors for patients with diabetes: continuous glucose absorption from glucose containing PD solutions may lead to hyperglycaemia, obesity, hyperlipidaemia, and increased peritoneal permeability and fibrosis. Early initiation of non-glucose solutions has been proposed to slow the progression of some of these complications Diabetic patients newly commenced on PD must regularly assess blood glucose levels, and have the integrated support from renal and diabetic teams to maximise the potential of this treatment.