Psychotic Symptom De-Escalation - Illinois Critical Access Hospital
advertisement

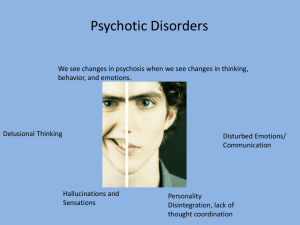
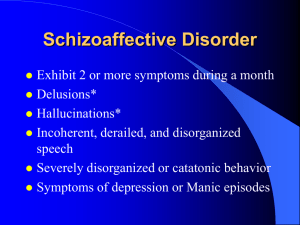
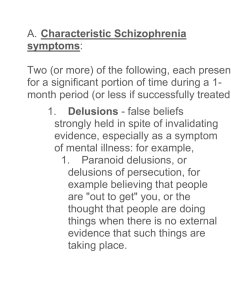
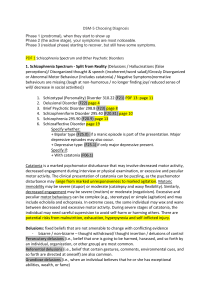
Rhonda Nelson, M.S. Ed, LCPC Aimee Anderson, MS A serious mental disorder characterized by thinking and emotions that are so impaired that they indicate that a person experiencing them has lost contact with reality Difficulties concentration Depressed mood Sleep changes – sleeping too much or not enough Anxiety Suspiciousness Withdrawal from family and friends Ongoing unusual thoughts and beliefs Delusions Hallucinations Disorganized speech – switching topics erratically Depression Anxiety Suicidal thoughts or actions Difficulty functioning A firmly held false belief or impression even when contrived by reality and what is commonly known as true. Delusions of Paranoia Grandiose delusions Somatic delusions A sensory perception in the absence of outside stimulus. Seeing Hearing Smelling Feeling Delusions and Hallucinations are the positive symptoms of psychotic disorders. They seem real to the person experiencing them Negative symptoms include: Loss of motivation Social withdrawal Blunted emotions Thinking difficulties Schizophrenia Delusional Disorder Brief Psychotic Disorder Schizophreniform Disorder Schizoaffective Disorder Bi-polar disorder During periods of mania Major Depressive Disorder During periods of severe depression Brain diseases: Parkinson’s, Huntington’s, and some chromosomal Brain tumors or cysts Dementia (including Alzheimer's disease) HIV, syphilis, and other infections that attack the brain Some types of epilepsy Stroke Alcohol Illegal drugs: Simulants Methamphetamine Cocaine Hallucinogenic Drugs (LSD) Bath salts; synthetic drugs (K2) Long periods without sleep Prescription drugs: steroids and stimulants Possibly genetic 50% chance of developing a psychotic disorder if identical twin has been diagnosed Higher risk if immediate family (parent/sibling) member has been diagnosed Brief reactive psychosis Response to an extreme situation, death of family member, short-lived response (days) Rapid tranquilization Medications Therapy Psycho-education Case Management Approach the person in a caring and nonjudgmental way to discuss your concerns Allow the person to talk about their experiences and beliefs if they want to, but do not force them Choose a private time and place, free from distractions Let the person know you are concerned and want to help- state the specific behaviors that concern you Let the person know you are available to talk in the future Be sensitive to the way the person is behaving Respect the person’s privacy and confidentiality Let the person set the pace and style of interaction Do not touch the person without permission Assist the person by remaining calm Talk in a clear, concise way Use short, simple sentences Speak quietly in a non-threatening tone at a moderate pace Answer questions calmly Comply with reasonable requests Maintain your safety and access to an exit Do not do anything to further agitate the person Understand the symptoms for what they are Empathize with how the person is feeling about his/her beliefs and experiences Be patient and allow plenty of time for responses Be aware that just because the person may be showing a limited range of emotions this does not mean they are not feeling anything Do not assume the person cannot understand you, even if the response is limited Give the person hope for recovery Provide practical help Do not make any promises that you cannot keep Doctors – Primary Care Physicians Psychiatrists Social workers, counsellors & other mental health professionals Certified Peer Specialists + Peer support groups + Family, friends, faith and other social networks + Family support groups + Discontinuation of alcohol and other drugs Encourage the person to talk with someone he/she trusts Never threaten the person with hospitalization Remain patient Remain friendly and open The person may want your help in the future