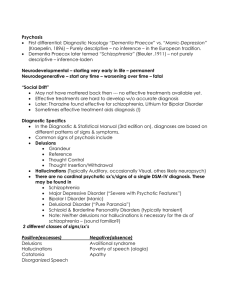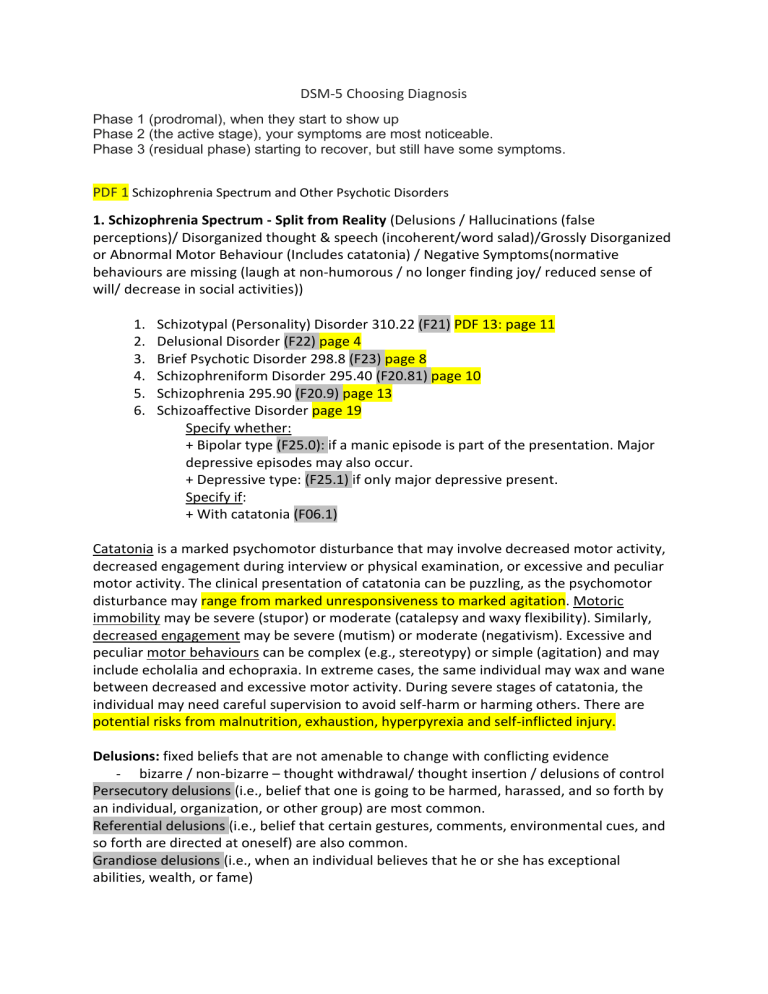
DSM-5 Choosing Diagnosis Phase 1 (prodromal), when they start to show up Phase 2 (the active stage), your symptoms are most noticeable. Phase 3 (residual phase) starting to recover, but still have some symptoms. PDF 1 Schizophrenia Spectrum and Other Psychotic Disorders 1. Schizophrenia Spectrum - Split from Reality (Delusions / Hallucinations (false perceptions)/ Disorganized thought & speech (incoherent/word salad)/Grossly Disorganized or Abnormal Motor Behaviour (Includes catatonia) / Negative Symptoms(normative behaviours are missing (laugh at non-humorous / no longer finding joy/ reduced sense of will/ decrease in social activities)) 1. 2. 3. 4. 5. 6. Schizotypal (Personality) Disorder 310.22 (F21) PDF 13: page 11 Delusional Disorder (F22) page 4 Brief Psychotic Disorder 298.8 (F23) page 8 Schizophreniform Disorder 295.40 (F20.81) page 10 Schizophrenia 295.90 (F20.9) page 13 Schizoaffective Disorder page 19 Specify whether: + Bipolar type (F25.0): if a manic episode is part of the presentation. Major depressive episodes may also occur. + Depressive type: (F25.1) if only major depressive present. Specify if: + With catatonia (F06.1) Catatonia is a marked psychomotor disturbance that may involve decreased motor activity, decreased engagement during interview or physical examination, or excessive and peculiar motor activity. The clinical presentation of catatonia can be puzzling, as the psychomotor disturbance may range from marked unresponsiveness to marked agitation. Motoric immobility may be severe (stupor) or moderate (catalepsy and waxy flexibility). Similarly, decreased engagement may be severe (mutism) or moderate (negativism). Excessive and peculiar motor behaviours can be complex (e.g., stereotypy) or simple (agitation) and may include echolalia and echopraxia. In extreme cases, the same individual may wax and wane between decreased and excessive motor activity. During severe stages of catatonia, the individual may need careful supervision to avoid self-harm or harming others. There are potential risks from malnutrition, exhaustion, hyperpyrexia and self-inflicted injury. Delusions: fixed beliefs that are not amenable to change with conflicting evidence - bizarre / non-bizarre – thought withdrawal/ thought insertion / delusions of control Persecutory delusions (i.e., belief that one is going to be harmed, harassed, and so forth by an individual, organization, or other group) are most common. Referential delusions (i.e., belief that certain gestures, comments, environmental cues, and so forth are directed at oneself) are also common. Grandiose delusions (i.e., when an individual believes that he or she has exceptional abilities, wealth, or fame) Erotomanic delusions (i.e., when an individual believes falsely that another person is in love with him or her) are also seen. Nihilistic delusions involve the conviction that a major catastrophe will occur, and somatic delusions focus on preoccupations regarding health and organ function. Hallucinations: perception-like experiences - No external stimulus - Vivd + clear - Appear completely real to patient (full force of normal perceptions) - Involuntary - Any sensory modality (schizophrenia related disorders – mostly auditory) - Distinct from own thoughts - Must occur in clear sensorium context, not when waking up (hypnopompic) or falling asleep (hypnagogic). Disorganized Thought / speech Disorganized thinking (formal thought disorder) - (derailment or loose associations) - Tangentially – answers to questions not really relatable - Incoherence / world salad (very severe) resembling receptive aphasia - Symptoms must be severe enough to effect function Grossly Disorganized or Abnormal Motor Behaviour - Childlike silliness – unpredictable agitation ( symptoms lead to function difficulty) - Catatonia (marked decrease in reactivity to environment) o ranges from resistance to instructions to maintaining bizarre posture, to lack of motor (stupor) or verbal responses (mutism) o nonspecific to schizophrenia Negative Symptoms - morbidity (mostly schizophrenia disorder) - Avolition – decrease in motivated self-initiated purposeful activities (sit for long periods / little interest in activities / social events) - Diminished emotional expression – reduction in expression of emotions in the face / eye contact / intonation of speech (prosody) / hand/head/face movements that show emotion. - Alogia – diminished speech output - Anhedonia - decreased ability to experience pleasure from positive stimuli or a degradation in the recollection of pleasure previously experienced. - Asociality - refers to the apparent lack of interest in social interactions and may be associated with avolition, but it can also be a manifestation of limited opportunities for social interaction. 1. Schizotypal (Personality) Disorder 310.22 (F21) PDF 13: page 11 - Pervasive pattern of social/interpersonal deficits marked by acute discomfort and reduced capacity for close relationships + cognitive / perceptual distortions and eccentricities of behaviour – start early adulthood – indicated by 5 or more factors… Differential Diagnosis: - Paranoid / Schizoid personality disorder: (also show detachment and restricted affect, but Schizotypal P shows presence of cognitive/perceptual distortions and marked eccentricity or oddness. - Avoidant personality disorder: Limited close-relationships - Schizotypal - lack of desire in creating relationships / avoidant personality disorder has active desire to form relationships but fear of rejection gets in the way. - Borderline personality disorder: - Transient, psychotic-like symptoms (related to affective shifts in response to stress, anxiety / more dissociative – derealisation / depersonalization) / SchizoPD- enduring psychotic symptoms that worsen under stress. - social isolation (secondary due to angry outburst – there is desire to connect) Impulsive and manipulative / schizotypal not. Narcissistic PD: suspiciousness, social withdrawal, or alienation – Narcissistic PD – fear of having imperfections revealed Example: F21 Schizotypal personality disorder (premorbid); F20.9 Schizophrenia (primary); 2. Delusional Disorder (F22) page 4 - - Presence of one or more delusions for a month or longer in a person who, except for the delusions and their behavioural ramifications, does not appear odd and is not functionally impaired. Prominent hallucinations and other psychotic or marked mood symptoms are absent. Non-prominent hallucinations and odd behaviours related to the delusional theme may be present. Look at types / specifiers / severity 3. Brief Psychotic Disorder 298.8 (F23) page 8 - Presence of 1 or more of following, at least 1 must be in top 3. 1. Delusions, 2. Hallucinations, 3. Disorganized Speech, 4. Grossly disorganized / catatonic behaviour At least 1 day – less than 1 month – full return to premorbid functioning Not better explained by Major Depressive Disorder / bipolar with psychotic features / schizophrenia / catatonia. Look at specifiers / severity 4. Schizophreniform Disorder 295.40 (F20.81) page 10 - Two (or more) of the following, each present for a significant portion of time during a 1month period (or less if successfully treated). At least one of these must be (1), (2), or (3): 1. Delusions. 2. Hallucinations. 3. Disorganized speech (e.g., frequent derailment or - incoherence). 4. Grossly disorganized or catatonic behaviour. 5. Negative symptoms (i.e., diminished emotional expression or avolition). lasts at least 1 month but less than 6 months Schizoaffective disorder and depressive or bipolar disorder with psychotic features have been ruled out 1) no major depressive or manic episodes occurred + if they have occurred (minor) - Specifiers 5. Schizophrenia 295.90 (F20.9) page 13 - 2 positive symptoms – at least one symptom must be from 1, 2 or 3 (1. Delusions. 2. Hallucinations. 3. Disorganized speech (e.g., frequent derailment or incoherence). 4. Grossly disorganized or catatonic behaviour. 5. Negative symptoms (i.e., diminished emotional expression or avolition) - - Persist for at least 6 months (1 month within these 6 month worth of symptoms) Schizoaffective disorder and depressive or bipolar disorder with psychotic features have been ruled out 1) no major depressive or manic episodes occurred + if they have occurred (minor) If there is a history of autism spectrum disorder or a communication disorder of childhood onset, the additional diagnosis of schizophrenia is made only if prominent delusions or hallucinations, in addition to the other required symptoms of schizophrenia, are also present for at least 1 month Specifiers Patients lack awareness of their symptoms Deficit in executive functioning/ memory/attention Psychosis – losing contact with reality Rarely violent or aggressive – more likely to inflict harm on self or be victim of violence 6. Schizoaffective Disorder page 19 Specify whether: + Bipolar type (F25.0): if a manic episode is part of the presentation. Major depressive episodes may also occur. + Depressive type: (F25.1) if only major depressive present. Specify if: + With catatonia (F06.1) - An uninterrupted period of illness during which there is a major mood episode (major depressive or manic) AT some time during this period – schizophrenia criterion A must be met. No social dysfunction No exclusion of Autism or Communication D of childhood onset The major depressive episode must include Criterion A1: Depressed mood. B. Delusions or hallucinations for 2 or more weeks in the absence of a major mood episode (depressive or manic) during the lifetime duration of the illness. C. Symptoms that meet criteria for a major mood episode are present for the majority of the total duration of the active and residual portions of the illness. - If the mood symptoms are present for only a relatively brief period, the diagnosis is schizophrenia, not schizoaffective disorder. In bipolar disorder, you have mood swings that include depression and mania. If you have schizoaffective disorder, you can have these bipolar symptoms. But separate from those, you also get psychotic symptoms similar to schizophrenia for at least 2 weeks at a time.