Female Reproductive System
advertisement
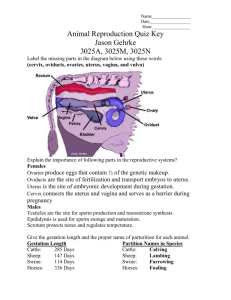
Female Reproductive System Adolescence Puberty Burst of hormones activate maturation of the gonads: ovaries Begins: 8-13 yrs of age Abnormally early = precocious puberty Delayed =Primary Amenorrhea Function of Female Reproductive System Produce sex hormones Produce functioning gamates [ova] Support & protect developing embryo General Physical Changes Axillary & pubic hair growth Changes in body conformation [widening of hips, development of breasts] Onset of first menstrual period [menarche] Mental changes Data from the 1998 Canadian GSS. Students living at home aged 15-19. THE EMOTIONAL HEALTH OF ADOLESCENT GIRLS A CONCERN Our analyses show that adolescent girls in the 15 to 19 age group may be more emotionally vulnerable today than they were in the 1980s. Girls surveyed in 1998 reported higher levels of time pressure and stress, and were less satisfied with their life, self-esteem, and the way they spent time than boys. they assessed their health lower than the boys, and reported having more difficulty falling asleep. The most surprising finding is, that girls' levels of life satisfaction and satisfaction with their self-esteem were in 1998 lower than those reported by adult employed women, who face considerably greater work challenges and time pressures. Source: Zuzanek, J. (2000). The effects of time use and time pressure on child-parent relationships. Waterloo: Otium Publications . Major Organs Ovaries [ gonads] Uterine tubes [ fallopian tubes] Uterus Vagina Accessory glands External genitalia Breasts ovaries Each ovary is about the size and shape of an almond. In young women the ovaries are about 1½ - 2 inches long, 1 inch wide & 1/3 inch thick. After menopause they tend to shrink. they produce eggs (also called ova) every female is born with a lifetime supply of eggs they also produce hormones: Estrogen & Progesterone Male Homolog = testes oogenesis when the girl becomes sexually mature, the primary oocytes recommence their development, usually one at a time and once a month. The primary oocyte grows much larger and completes the meiosis I, forming a large secondary oocyte and a small polar body that receives little more than one set of chromosomes. oogenesis In humans (and most vertebrates), the first polar body does not go on to meiosis II, but the secondary oocyte does proceed as far as metaphase of meiosis II and then stops. Only if fertilization occurs will meiosis II ever be completed. Entry of the sperm restarts the cell cycle fallopian tubes [uterine tubes] stretch from the uterus to the ovaries and measure about 8 to 13 cm in length. range in width from about one inch at the end next to the ovary, to the diameter of a strand of thin spaghetti. The ends of the fallopian tubes lying next to the ovaries feather into ends called fimbria Millions of tiny hair-like cilia line the fimbria and interior of the fallopian tubes. The cilia beat in waves hundreds of times a second catching the egg at ovulation and moving it through the tube to the uterine cavity. Fertilization typically occurs in the fallopian tube uterus pear-shaped muscular organ in the upper female reproductive tract. The fundus is the upper portion of the uterus where pregnancy occurs. The cervix is the lower portion of the uterus that connects with the vagina and serves as a sphincter to keep the uterus closed during pregnancy until it is time to deliver a baby. the uterus expands considerably during the reproductive process. the organ grows to from 10 to 20 times its normal size during pregnancy. uterus The main body consists of a firm outer coat of muscle (myometrium) and an inner lining of vascular, glandular material (endometrium). The endometrium thickens during the menstrual cycle to allow implantation of a fertilized egg. Pregnancy occurs when the fertilized egg implants successfully into the endometrial lining. If fertilization does not occur, the endometrium sloughs off and is expelled as menstrual flow. endometrium Functional zone – layer closest to the cavity – contains majority of glands. Thicker portion – undergoes changes with monthly cycle Basal zone – layer just under myometrium, attaches functional layer to myometrial tissue, has terminal ends of glands. Remains constant Uterine arteries Arcuate arteries - encircle endometrium Radial arteries – connect arcuate to straight Straight arteries – deliver blood to basilar zone Spiral arteries – deliver blood to functional zone The Cervix the lower portion or neck of the uterus. The cervix is lined with mucus, the quality and quantity of which is governed by monthly fluctuations in the levels of the estrogen and progesterone. When estrogen levels are low, the mucus tends to be thick and sparse, hindering sperm from reaching the fallopian tubes. But when an egg is ready for fertilization, estrogen levels are high, the mucus then becomes thin and slippery, offering a “friendly environment” to sperm at the end of pregnancy, the cervix acts as the passage through which the baby exits the uterus into the vagina. The cervical canal expands to roughly 50 times its normal width in order to accommodate the passage of the baby during birth The Vagina vagin = sheath a muscular, ridged sheath connecting the external genitals to the uterus. functions as a two-way street, accepting the penis and sperm during intercourse and roughly nine months later, serving as the avenue of birth through which the new baby enters the world External genetalia vulva—which runs from the pubic area downward to the rectum. Mons pubis or "mound of Venus" is the V-shaped area covered with hair Labia majora or "greater lips" are the part around the vagina containing two glands (Bartholin’s glands)which helps lubrication during intercourse. Male Homolog = scrotum Labia minora or "lesser lips" are the thin hairless ridges at the entrance of the vagina, which joins behind and in front. In front they split to enclose the clitoris The clitoris is a small pea-shaped structure (equivalent to penis in males ) It plays an important part in sexual excitement in females. Male Homolog = penis External genetalia The urethral orifice or external urinary opening is below the clitoris on the upper wall of the vagina and is the passage for urine The introitus or opening of the vagina is separate from the urinary opening (unlike males) and located below it. The hymen is a thin cresentic fold of tissue which partially covers the opening of the vagina. medically it is no longer considered to be a 100% proof of female virginity. Mammary Glands [ breasts] Present in both sexes - normally only functional in females Developmentally they are derived from sweat glands Contained within a rounded skin-covered breast anterior to the pectoral muscles of the thorax Slightly below center of each breast is a ring of pigmented skin, the areola - this surrounds a central protruding nipple Internally - they consist of 15 to 25 lobes that radiate around and open at the nipple Each lobe is composed of smaller lobules- these contain alveoli that produce milk when a women is lactating non-pregnant women - glandular structure is undeveloped - hence breast size is largely due to the amount of fat deposits glands Lesser Vestibular (Paraurethral, Skene's) Male Homolog = prostate located on the upper wall of the vagina, around the lower end of the urethra. They drain into the urethra and near the urethral opening Function - mucus production to aid lubrication during intercourse Greater Vestibular (Bartholin's) Male Homolog = bulbourethral glands located slightly below and to the left and right of the opening of the vagina. They secrete mucus to provide lubrication, especially when the woman is sexually aroused Table 1. Production Rate of Sex Steroids in Women at Different Stages of the Menstrual Cycle DAILY PRODUCTION RATE SEX STEROIDS* Early Follicular Preovulatory Midluteal Progesterone (mg) 1 4 25 17-Hydroxyprogesterone (mg) 0.5 4 4 Dehydroepiandrosterone (mg) 7 7 7 2.6 4.7 3.4 144 171 126 Estrone (mg) 50 350 250 Estradiol (mg) 36 380 250 Androstenedione (mg) Testosterone (mg) From Baird DT. Fraser IS. Blood production and ovarian secretion rates of esuadiol-17b and estrone in women throughout the menstrual cycle. J Clin Endocri-nol Metab 38: l009-1017. 1974. @ The Endocrine Society. *Values are expressed in milligrams or micrograms per 24 hours. Hormones and the menstrual cycle The female hormones that control the cyclic growth and shedding of the endometrium are estrogen and progesterone. Estrogen and progesterone are produced by the ovaries. Estrogen causes the growth or proliferation of the endometrium during the first 2 weeks of the menstrual cycle. After ovulation, the ovary produces progesterone. http://www.sumanasinc.com/webcontent/anisamples/majorsbiology/ ovarianuterine.html When does ovulation occur? The timing of ovulation varies with the length of a woman's menstrual cycle. In the average 28 day menstrual cycle, the LH surge usually occurs between cycle days 11-13 and ovulation follows about 36-48 hours later, on or close to cycle day 14. Women with shorter menstrual cycle lengths tend to ovulate earlier and women with longer cycle lengths tend to ovulate later than cycle day 14. Despite the variations in menstrual cycle length, the time from ovulation to the onset of the next menstrual period is usually constant (2 weeks). This principle is the basis for the use of ovulation calendars that take into account an individual's shortest and longest cycle lengths.