362 Heart Failure
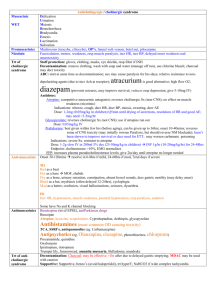
advertisement

Heart Failure 1 – This is the ability to increase CO during increased activity Cardiac Reserve 2 – Decr in pumping ability with consequent decr in cardiac reserve & adaptive mechanisms that serve to maintain CO contributes to progression of? Heart Failure (HF) 3 – HF involves what 2 interactions? a. These interactions involve what patho changes? 1) Decr in pumping ability with decr cardiac reserve consequently 2) Adaptive mechanisms fail to maintain CO a. 4 – Define CO a. b. What regulates HR? What factors affect SV? LV. dilates LV. hypertrophy Neurohormonal stimulation (SNS, RAAS) V. remodeling CO = HR x SV (bpm x how much pumped per beat) a. SNS incr HR Para NS decr HR b. Preload, afterload & cardiac contractility 5 – This is loading of the heart at the end of diastole / Volume of blood stretching the resting heart a. Determined by? b. Maximum volume of this causes tension in heart walls which is called what? Preload a. Venous return b. End Diastolic Volume (EDV) - provides estimate of preload status - measured clinically 6 – Overstretched ventricles due to extra volume causes- incr intraventricular pressure, decr SV, & overstretched muscle fibers- describe what? a. So what if muscles fibers are overstretched? (elevated) Preload in HF 7 – What happens overall to preload in HF? Ventricles are overstretched due to incr volume - Intraventricular pressure rises - SV decr - Muscle fibers overstretch impaired pumping & elevates preload even more 8 – Preload = ? EDV 9 – Impaired pumping action of ventricles can elevate what? a. Examples of impaired pumping action: a. Impaired pumping/ ejecting blood & preload elevates Preload a. Damage from MI Dilated cardiomyopathy Myocarditis Valvular heart disease Hypertension Renal failure with excess circulatory vol. 10 – A pt with preload has impaired ventricle pumping acting due to what possible causes? HTN Renal failure w/ excess vol. Myocarditis Valvular heart disease Dilated cardiomyopathy MI damage 11 – This is the force that the contracting heart generates to eject blood from filled ventriclesa. Components include? Afterload a. Systemic vascular resistance (SVR) b. Ventricular wall tension 12 – SVR and Ventricular wall tension are components to afterload, force that ejects blood from the heart. What SVR issues lead to afterload problems? Aortic stenosis Arterial HTN Peripheral vasoconstriction 13 – Ventricular ejection & incr ventricular wall stress is impaired by what? Excessive afterload 14 – A pt with an excessive afterload causes impaired… Ventricular ejection Incr wall stress 15 – This is the mechanical performance of the heart- Cardiac Contractility 16 – A pt’s change in developed tension at a given resting fiber length, ability of heart muscle to shorten, pumping, contract & relax, and ability of contractile elements (actin, myosin) to interact with & shorten against a load determines what? Cardiac Contractility 17 – What determines cardiac contractility in a pt? -Pumping -Contract & shorten -Change in developed tension -Ability of heart muscles to shorten -Ability of contractile elements to interact/shorten against a load 18 – What increases CO INDEPENDENT of preload & muscle strength? a. What can affect this^ Cardiac contractility a. Inotropic influence 19 – What causes a +, - Inotropic influence? (+) Inotropic effect – Sympathetic stimulation - Digoxin, dobutamine - Incr strength of contraction (-) Inotropic effect –Hypoxia, Ischemia - MI, cardiomyopathy - Decr contractility 20 – A pt with MI and/or has cardiomyopathy has which inotropic effect? Negative, decr contractility 21 – This is an adaptive/compensatory mechanism used in HF- Frank-Starling Mechanism - Supports CO - Incr SV 22 – Frank-Starling is an adaptive mechanism used in HF, what does it do/when is it ineffective? Ineffective when heart is overfilled & fibers overstretched -Help support CO -Incr SV by: Incr EDV Incr myocardial fiber stretch Incr force of next contraction -Ineffective when heart is overfilled and overstretched 23 – Compensatory mechanisms try to maintain CO; What is SNS role in HF to do this? Elevate catecholamine levels in late stage HF -E & NE -Directly stimulates HR & Contractility -Maintain perfusion (brain, heart, skeletal m.) Negative aspects: Incr SVR & Afterload Decr perfusion in (skin, kidney, abdom. organs) 24 – A pt’s SNS in late stage HF does what? Elevate catecholamines E & NE Directly stimulates HR & Contractility Maintain perfusion of Heart/Brain/& Skel m. RAAS System effects: Decr CO Decr Renal blood flow Incr Renin secretion from Kidneys w/ Angiotensin II Incr Vasoconstriction, Aldosterone & ADH - Aldosterone: Incr tubular absorption (retains fluid) ADH: Vasoconstrict & inhibit h2o release 25 – T/F Adaptive mechanisms don’t work when a pt has HF T 26 – This peptide is released from the atria with incr stretch & pressure that serves to: - Produce rapid, transient natriuresis, dieresis and moderate loss of K (body’s diuretic) - Inhibit adlosteron & rennin secretion - Antagonist to angiotensin II - Inhibit release of NE from presynaptic nerve terminals Atrial Natriuetic Peptide (ANP) 27 – ANP’s are released in a pt with an incr in stretch & pressure (such as HF); What do they do following release? Produce body’s diuretic components & loss of K Inhibit aldosterone & renin secretion Antagonist to angiotensin II Inhibit release of NE 28 – This is stored in Ventricular cells and functions similar to ANP’s a. BNP and ANP are elevated when? b. When a pt has HF, what levels rise? Brain Natriuretic Peptide (BNP) a. HF b. BNP & ANP 29 – What develops as compensation for an incr myocardial workload? Hypertrophy 30 – How does Hypertophy become pathologic? Structural changes in mass & dilation Functional changes impair sys & dia. Hemodynamic overload may develop Risk for morbidity & mortality HF in a nutshell –enlarge & can no longer compensate* 31 – Myocytes and Nonmyocytes compose what? (tissue hypertrophy possible) Myocardium 32 – Myocardium is composed of: a. Functional cardiac muscle units, which growth is limited in cell size not #- called? b. These are cardiac macrophages/fibroblasts/ vascular smooth muscle/ endothelial cells that provide support for myocytes; also capable to incr in cell # 33 – RAAS (angiotensin II) and some SNS drives what? a. b. Myocytes Nonmyocytes Ventricular Remodeling (refer to slide diagram) 34 – The following are causes of what? - Mi - Cardiomyopathy - Valvular heart disease - Ischemic heart disease - Excessive work demand: HTN, Volume overload, Hypermetabolic states (hyperthyroidism) HF 35- A pt with HF may be caused by what? Excessive work demands (HTN, volume overload, hypermetabolic states) - Accompanied by congestion of body tissues MI Valvular heart disease Ischemic heart disear Cardiomyopathy HF High-Output Uncommon Excessive need for CO Causes: Severe anemia Hyperthyroidism Sepsis Thyrotoxicosis Low-Output Common Caused by disorders that impair pumping: Cardiomypathy Ischemic heart disease (IDH) 36 – A pt with an impaired pumping ability due to cardiomyopathy has which common HF? Low-output 37 – An excessive need for cardiac output due to severe anemia, hyperthyroidism, sepsis or thyrotoxicosis is which kind of HF? High-output Systolic o Impaired pumping/ ejection: EF 55-65% o Declines progressively with myocardial dysfunction - Incr diastolic volume, ventricular dilation & wall tension -Incr end diastolic pressure o Decr in cardiac contractility o Causes: Impaired Contractile performance Vol. & pressure overload Diastolic o Smaller ventricular chamber size, ventricular hypertrophy & poor ventricular compliance (@ rest) o Causes: Restrict diastolic filling Incr ventricle wall thickness Reduce chamber size Delayed diastolic relaxation 38 – This pt has what dysfunction: ejection fraction of 55%, contractility impaired due to hypoxia (neg inotropic effect), volume and pressure over load Systolic dysfunction 39 – A pt with smaller chamber size, ventricular hypertrophy, and poor ventricular compliance caused by restricted filling, wall thickness, delayed relaxation and decr chamber size has which dysfunction? Diastolic Right-side HF Left-side HF Venous* Define Causes Accum blood in systemic VENOUS sys. / congestion in peripheral tissues Incr in RA, RVEDP, Systemic Venous Pressures* - Persistent Left side failure Stenosis or regurgitation of tricuspid or pulmonic valves RV infarct. Cardiomyopathy Cor pulmonae –due to lung disorder (i.e. severe pneumonia, PE, pulm HTN) Pulmonary* Decr CO Incr LA & LVEDP Pulmonary Congestion circulation* Pulmonary capillary filtration pressure > capillary osmotic pressure = shift of intravascular fluid into interstitium of lung Pulmon. Edema Acute MI (AMI) Cardiomyopathy S&S Fatigue Dependent edema (both legs) JVD Liver engorgement Ascites Anorexia + complaints of GI distress (appetite loss) Cyanosis Elevation in peripheral venous pressure –fluid retention Cyanosis Blood-tinged sputum Cough -crackles Paroxysmal nocturnal dyspnea Orthopnea DOE 40 – Incr right atrial pressure (RA), right ventricle end diastolic pressure (RVEDP) and systemic venous pressure leads to accumulation? a. Possible causes? Accumulation of blood in the venous system, congestion of peripheral tissues Right-sided HF a. Cardiomyopathy Cor pulmonae Right ventricular infarction Stenosis or regurgitation of tricuspid/pulmonic valves Persistent Left-side failure 41 – A pt with an AMI and cardiomyopathy would have a decr in CO, with incr pressures in LA and LVEDP due to PULMONARY CONGESTION- has which side HF? Left-sided HF 42 – What happens in a pt with Right-sided HF? a. How can it manifest? Accumulation of blood in venous system Increased pressures Right atrial Right ventricular end-diastolic Systemic venous a. 43 – What happens in a pt with Left-sided HF a. How can it manifest? Dependent edema, cyanosis, fatigue, JVD, ascites, peripheral venous pressure elevated, fluid retention, anorexia, GI distress, loss of appetite and liver engorgement Pulmonary Congestion from decr CO Increased pressures Left atria Left ventricular end diastolic Pulmonary capillary filtration is greater than osmotic intravascular shift to interstitial pulmonary edema a. Paroxysmal nocturnal dyspnea, DOE, cyanosis, blood-tinged sputum, orothpnea and coughing Manifestations of HF Incr capillary pressures –overfill vascular system & venous congestion Nocturia (later- Oliguria) due to incr in kidneys when asleep Fluid retention & edema o o Respiratory Dyspnea –due to pulmonary congestion DOE Orthopnea Paroxysmal Noctural Dyspnea (PND) –sudden attack of SOB while asleep Chronic, dry, nonproductive cough (worse supine) Fatigue & ltd’ exercise tolerance Low LV output Progressive with incr daily activity Advanced HF –confusion, memory, anxiety, insomnia Cachexia & malnourished Due to - Cyanosis –Late sign* fatigue, malnutrition Liver & GI congestion –lead to impaired digestion/absorption (bloaty full feeling) Circulating toxins & mediators released from poorly perfused tissues Lips & peripheral extremities Refer to R & L HF diagram* Cause Pulmonary Edema HF –most common* Pulmonary capillary pressures > capillary oncotic pressures capillary fluid moves to alveoli lung stiffness, difficult expansion impair gas exchange Capillary injury Lymphatic block Hemoglobin leaves lungs w/o fully oxygenating SOB, cyanosis S&S Life threatening Gasp for air while seated Rapid pulse Moist cool skin -Cyanotic lips & nails Productive cough of frothy, blood-tinged sputum Crackles Worsen: confustion to stupor Terminal: death rattle –drown in own secretions 44 – A pt has pulmonary edema due to the most common cause, HF- what is happening in the lungs? Pulmonary capillary pressures exceed oncotic pressures Fluid moves to alveoli Causing lung stiffness, difficulty expanding Impairing gas exchange: Hemoglobin is leaving lungs w/o fully oxygenating #1 What manifestations are expected in a pt with only Left-sided HF? a. Hepatomegaly b. c. d. Dependent edema Pulmonary edema JVD C #2 Manifestations of Right-sided HF? a. PND b. Dependent edema c. Frothy pink sputum d. Crackles B #3 Which of the following puts a pt at risk for Highoutput HF? a. COPD b. MI c. Thyrotoxicocis d. Restrictive myocardiopathy C #4 Left-sided HF EKG shows normal LV EF; What type of HF is this? a. Diastolic HF b. High-output HF c. Systolic HF d. Total HF A