Billing and Coding: How to Ensure Efficiency
advertisement

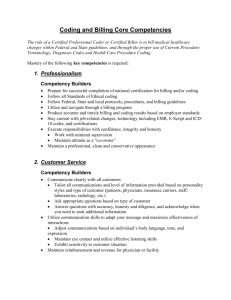
BILLING & CODING How to Ensure Efficiency Tammy W. Norville, RMC Primary Care Systems Specialist March 3, 2011 The North Carolina Office of Rural Health and Community Care (ORHCC) helps communities get lowcost access to medical care. Since it was created in 1973, ORHCC has opened 86 rural health centers across the state. Currently, ORHCC supports 28 rural health centers with funding and technical support. ORHCC also helps to place medical, psychiatric, and dental providers in communities throughout the state. Rural hospitals, as well as many statewide medical facilities that treat poor and uninsured residents, may receive help through grant funds. Qualifying patients may take advantage of drug companies’ free and low-cost drug programs through ORHCC’s medication assistance program. Road Map Preamble – Claims Management Cycle Part 1 – What is Efficiency? Part 2 – Billing & Coding Part 3 – Conclusion & Questions Preamble Claims Management Cycle Claims Management Revenue Cycle Components Registration Clinical Documentation Check-Out Coding Billing Insurer Collections Paid in Full!! Our Focus Coding – Code Verification & Review Pre-auth, Pre-cert or Pre-determination Billing – Claim Generation Claim Review Collections – Collections/Claim Follow-Up Posting Payments Appealing Claims Part 1 What is Efficiency??? Definitions The quality or degree of being efficient Effective operation as measured by a comparison of production with cost (as in energy, time and money) The ratio of the effective or useful output to the total input in any system Definitions The ratio of the useful energy delivered by a dynamic system to the energy it supplies The degree to which this quality is exercised Word Play Time to have a little fun!!! What are a few… Synonyms Antonyms Tammy’s Picks Synonyms Edge Antonyms Ineffectiveness Effectiveness Ineffectualness Productiveness Unproductiveness Competence Incompetent Question How do you know if something is efficient? The Take-Away Know the process & Know your role Let us pause for a commercial… A brief moment to meditate on FQHC/RHC Reimbursement (Sappy music playing in the background…..) FQHC/RHC Reimbursement Applies to Medicare and Medicaid Patients ONLY Payment for these Core Visits are on an ALL INCLUSIVE RATE PER VISIT created by dividing a practice’s total allowable costs by it’s total FQHC/RHC visits. In addition, other Medicaid FQHC/RHC services are reimbursed on a fee-for-service basis and are reconciled to cost at the end of the year. FQHC/RHC Reimbursement Under the FQHC/RHC program, the practice is allowed to “break even” on the cost of providing FQHC/RHC services to Medicare and Medicaid patients. The FQHC/RHC program does not affect reimbursement for private insurance and self-pay patients. Part 2 Billing & Coding What is a Coding Person’s Job? To capture what a Provider did (the service they provided the patient) and why they did it – based on the ICD-9 codes selected and documented by the Provider. What is a Billing Person’s Job? Submit timely and accurate claims the first time – get it paid!! Tell Me What You Think What does your coding/billing staff look like? How is it set up? Do you have the tasks separated? Reality Check!! Why is the information in the previous discussion relative/important?? Coding Overview Coding is the translation of services, procedures, events, circumstances and patient conditions into numeric designations which must be fully represented as documentation in the medical record. Coding Overview (con’t) Components of appropriate documentation – North Carolina Medical Board Requirements – Coding Requirements – CPT Manual Procedures must be supported by appropriate diagnosis codes – establishing medical necessity. Types of Codes Level I – CPT – Procedures Level II – HCPCS – Healthcare Common Procedural Coding System – drugs, supplies, Prosthetics, vision ICD-9 – Diagnoses – Volumes 1 and 2 Volume 3 Hospital only RBRVS – Resource Based Relative Value Scale – Fee schedule broken down into parts CCI – Correct Coding Initiative – Updated quarterly Coding Documentation - CPT Chief Complaint History of Present Illness Review of Systems Past, Family, Social History Exam – 1995 Rules Rule! Medical Decision Making Time - Sometimes The Billing Process Data Entry Electronic Insurance Claims Processing Insurance Provider Enrollment Insurance Contract Negotiation Insurance Claim Follow-Up Payment Posting Patient Invoicing Reporting & Analysis What’s The Big Deal? Inefficiencies in coding and/or billing may result in: • • • • • Loss of revenue Refunds Fines Accusations of Fraud Medicare – OIG – “Men in Black” Who Cares, Anyway? Other than the insurance companies that are paying claims – including Medicare and Medicaid Baltimore Statistical Office (aka, the National Center for Health Statistics) EVERY claim goes through this office without common knowledge. All ICD-9 codes are tracked – including trending to physician – and extracted. This information is disseminated to appropriate agencies (ex, CDC). RAC Program Mission "To reduce Medicare improper payments through efficient detection and collection of overpayments, the identification of underpayments, and the implementation of actions that will prevent future improper payments.” RAC AUDITS!!! The Centers for Medicare and Medicaid Services (CMS) awarded Connolly Healthcare the contract to provide recovery audit services mandated by the Tax Relief and Health Care Act of 2006 for Region C. The Recovery Audit Contractor (RAC) program is a cost containment effort aimed to reduce improper payments within Medicare programs as well as identify process improvements to reduce or eliminate future improper payments. Region C – RAC Connolly Healthcare is tasked with auditing Region C, which consists of the following states: AL, AR, CO, FL, GA, LA, MS, NC, NM, OK, SC, TN, TX, VA, WV and the territories of Puerto Rico and U.S. Virgin Islands. Reality Check!! Signs of Inefficiency Biller/Coder Skill Issues Incorrect/Inaccurate demographic/eligibility information Inaccurate or lack of coding Incomplete claims Lack of supporting documentation Poor communication with payer Not billing for services rendered No follow-up on A/R balance claims How Many Days in A/R? On average, how long does it take any given payer to remit payment from the date of claim processing? Total A/R Over 90 Days How much (or what percent) of your total Accounts Receivable (A/R) had a date of service/date of first billing greater than 90 days ago? 5 Steps to Increased Efficiency Tip #1 Know your team & ask for their help Strengths Weaknesses Areas needing education Areas of expertise Communicate with the team regularly!! Claims Processing & Review Discussion Tip #2 Review your internal claims process Are claims submitted accurately to the correct payer within the required timeline? Eligibility verification prior to visits? Tip #3 Review and reconcile claims payments Are claims payments received from payers? Are the payments accurate? Are they posted to patient accounts appropriately? Are denials, delays or reductions addressed? Are appeals used when appropriate? Tip #4 Run & Review Monthly Reports Collection EOB/ERA for each claim Production by user Tip #5 Know your payer fee schedules Are claims payments received from payers correct? Are the payments accurate? Are they posted to patient accounts appropriately? Do you maintain all health insurance contracts centrally and review regularly? More Information The American Medical Association is sponsoring the “Heal the Claims Process” ™ campaign. www.ama-assn.org/go/healthatclaim For educational material: www.ama-assn.org/go/pmc Other Ideas? Tell me what you think! Part 3 Why is this important?? What does the future hold?? If we’re inefficient now… What happens when we have to implement an entirely new coding system? Goodbye, ICD-9!!! Hello, ICD-10!!! Goodbye ICD-9! ICD-9-CM is outdated – – – – Technology has changed Categories are full Not descriptive enough Reimbursement – would enhance accurate payment for services rendered – Quality – would facilitate evaluation of medical processes and outcomes What do we need for a new coding system? Flexibility to quickly incorporate emerging diagnoses and procedures Exact enough to identify diagnoses and procedures precisely Hello, ICD-10!!! Incorporation of much greater specificity and clinical information which results in – Improved ability to measure health care services – Increased sensitivity when refining grouping and reimbursement methodologies – Enhanced ability to conduct public health surveillance – Decreased need to include supporting documentation with claims Development Background The new system is intended to replace ICD9-CM Volume 3 for reporting inpatient procedures ICD-10 has been around for years 1995-1996 First draft of ICD-10-PCS completed 1996-1998 Training and Testing 1998 – Present ICD-10-PCS updated annually Major Development Goals Improve accuracy and efficiency of coding Reduce training effort Improve communication with physicians Essential Attributes Completeness All substantially different procedures have a unique code Expandability The structure of the system allows incorporation of new procedures as unique codes Essential Attributes Standardized terminology Includes definitions of terminology used While the meaning of specific words can vary in common usage, ICD-10-PCS defines a single meaning for each term used in the system. General Principles Diagnostic information is not included in the code description A “not elsewhere classified” option is allowed for new devices and substances All substantially different procedures are defined Code Structure Codes are comprised of seven components. Each component is called a “character” All codes are seven characters long Individual units for each character are represented by a letter or number Each unit is called a “value” 34 possible values for each character Digits 0-9 Letters A-H, J-N, P-Z System Structure – 16 Sections Medical and Surgical Obstetrics Placement Administration Measurement and Monitoring Extracorporeal Assistance & Performance Extracorporeal Therapies Osteopathic Other Procedures Chiropractic Imaging Nuclear Medicine Radiation Oncology Physical Rehabilitation and Diagnostic Audiology Mental Health Substance Abuse Treatment Potential Implementation Issues Budgeting Personnel training Working with medical staff to ensure appropriate documentation available to reap the benefits of greater specificity Hardware and software changes Data conversion Potential Systems & Applications Affected (AHIMA) Encoding software Case mix systems Medical record abstracting Billing systems Registration and scheduling systems Accounting systems Decision support systems Clinical systems Utilization management Quality management Case management Clinical protocol Test ordering systems Performance measurement systems Medical necessity software Disease management systems Provider profiling systems Aggregate data reporting Timing OCTOBER 1, 2013 Start preparations for implementation now Estimate time frames for making needed software changes Educate Team – coders, billers, providers, etc. Web Resources CMS General ICD-10 Information http://www.cms.hhs.gov/ICD-10 • • • • • Complete version of ICD-10-PCS – updated annually User manual Mapping between ICD-9-CM and ICD-10-PCS PowerPoint speaker slides Technical paper explaining system ICD-10-PCS Coding System and Training Manual http://www.cms.hhs.gov/ICD9ProviderDiagnosticCodes/08_ICD10 .asp Web Resources CMS ICD-10-PCS Files http://www.cms.hhs.gov/ICD10/02_ICD-10-PCS.asp# ICD-10-CM Coding System http://www.cms.hhs.gov/ICD10/03_ICD_10_CM.asp# Web Resources AHA Central Office ICD-10 Resource Center http://www.ahacentraloffice.org/ICD-10 AHIMA ICD-10 General Information http://www.ahima.org/icd10 Implementation preparation Checklist The Take-Away What is the current impact of inefficiency on your organization ? The Take-Away What may be the future impact of inefficiency on your organization? The Take-Away What are your plans to deal with inefficiency in your organization? Web Resources http://www.cms.hhs.gov/ Centers for Medicare & Medicaid Services Coding/Documentation Requirements RAC Audits/Requirements HIPAA 5010 Implementation ICD-10 Implementation Web Resources http://www.ncmedboard.org/ NC Medical Board http://www.mgma.com/ Medical Group Management Association http://www.google.com/ Google **When in doubt, Google it!!** Questions/Comments?? Thank you for your participation!! Contact Info Tammy Norville Primary Care Systems Specialist tammy.norville1@dhhs.nc.gov Cell: (919) 215-0220 Office: (919) 733-2040 x 229