Compliance, Operation, Billing Best Practices
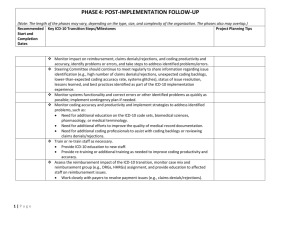
advertisement

I. COMPLIANCE & THE DIRECTORS II. UPDATE ON THE 3PB REVENUE ENHANCEMENT PROJECT III. OPERATIONS AND THE REIMBURSEMENT SYSTEM BEST PRACTICES IV. DASHBOARD FOR MANAGING THE REIMBURSEMENT SYSTEM HEALTH CARE COMPLIANCE Deliberate ignorance COMPLIANCE PROGRAMS • Voluntary in 2000…..Mandatory now • Evolved into Compliance and Ethics Programs • Affordable Care Act - Indian Health Care programs are deemed Essential Community Providers therefore ACO’s must include. ACO membership mandates the implementation of a compliance program DUTY OF CARE - BOARD RESPONSIBILITY • Must demonstrate good faith judgment • Must act in a manner an ordinarily prudent person would exercise under similar circumstances • Must act in a manner believed to be in the best interest of the corporation • Must perform reasonable inquiry – Is compliance program reporting and information system adequate from an oversight not operational perspective REASONABLE INQUIRY Ask knowledgeable and appropriate questions Structural Questions – designed to explore the adequacy of program breadth, reporting relationships and resources to implement the program Operational Questions – directed to an evaluation of the adequacy and vitality of the compliance program 2 CATEGORIES OF QUESTIONS ARE SUGGESTED FOR DIRECTORS: • Operational Questions – directed to an evaluation of the adequacy and vitality of the operations compliance program • Structural Questions –scope of the organization’s compliance program; designed to explore the adequacy of program breadth, reporting relationships and resources to implement the program STRUCTURAL QUESTIONS Compliance Infrastructure • How is the compliance program structured and who are the key employees responsible for its implementation and operation? • Do the personnel have sufficient authority, autonomy and resources to perform assessments and respond appropriately to misconduct to implement the compliance program? • Are employees held accountable for meeting these compliance-related objectives during performance reviews? STRUCTURAL QUESTIONS Measures to Prevent Violations • What is the scope of compliance-related education and training across the organization? • Has the effectiveness of such training been assessed? • What policies/measures have been developed to enforce training requirements and to provide remedial training as warranted? • How is the Board kept apprised of significant regulatory and industry developments affecting the organization’s risk? • How is the compliance program structured to address such risks? STRUCTURAL QUESTIONS Measures to Respond to Violations • What is the process by which the organization evaluates and responds to suspected compliance violations? • Does the organization have policies that address the appropriate protection of “whistleblowers” and those accused of misconduct? SMALL GROUP PRACTICE GUIDANCE OIG 2000 7 KEY COMPONENTS 1. Conducting internal monitoring and auditing 2. Implementing compliance and practice standards 3. Designating a compliance officer or contact 4. Conducting appropriate training and education 5. Responding appropriately to detected offenses and developing corrective action 6. Developing open lines of communication 7. Enforcing disciplinary standards through well publicized guidelines BOARD ACTIONS • Peer Review and Credentialing & Privileging • Policy and Procedures with controls for risk areas • Periodically evaluate the effectiveness of the compliance program • Ensure access to resources OPERATIONAL RISK AREAS • Coding and Billing Errors • Safety for patients and staff • Quality of Care • Contracting • Accuracy of reporting • Conflict of interest • Privacy and Security Rules • Harassment or intimidation • Culture of business environment • Social Networking RESOURCES • Participate with local hospital or physicians association programs • Health Care Compliance Association • American Academy of Professional Coders • American Health Information Management Association • Office of Inspector General • Center for Medicare and Medicaid Services 3PB REVENUE ENHANCEMENT PROJECT 3RD PARTY REVENUE ENHANCEMENT UPDATE • VISITED SITES • HOSTED 2 GATHERINGS • HOSTED 7 WEB-EX TRAININGS 1 MORE TO DO • 8 WEB-EX INTENSIVE SERIES FOR CODING PLANNED • IMPLEMENTING 3PB SYSTEMS AT 14 SITES • SUPPORTED SITES WITH FQHC APPLICATIONS • DEVELOPMENT OF SLIDING DISCOUNT SCHEDULES • ASSIST COORDINATION OF AREA OFFICE SUPPORT COMING UP • ACCOUNTS RECEIVABLES MANAGEMENT • INTENSIVE CODING SERIES • INTENSIVE MEDICARE SERIES • ICD-10 IMPLEMENTATION PLANNING • COMPLIANCE PROGRAM DEVELOPMENT FINDINGS • Need consistent support • Need for Electronic Health Record & Meaningful Use support • Need for regular coding and billing training • Need assistance processing Medicare/Medicaid FQHC applications • Practice Management systems being retired DASHBOARD • REAL MEANING OF ALL CAUGHT UP • PRODUCTIVITY MEASURES – Provider, Coder/Auditor, Biller • AGED RECEIVABLES – 0-30 31-60 61-90 91-120 120+ • COLLECTIONS AND REASONS FOR WRITE OFFS • SCHEDULE COLLECTION GOALS • MANAGE WARNING SIGNS AS ALERTS • BALANCE WITH FINANCE • TRAINING REQUIREMENTS • DIRECTORS 3RD PARTY REIMBURSEMENT MANAGEMENT WORKSHOP CONTRACT CAUTIONS……… • What is your reimbursement under this contract? And when are rates renegotiated? • Can the health insurer unilaterally change the terms? • Is the health insurer obliged to pay you promptly? • How is medical necessity defined? Who qualifies? • Does the contract or manual designate all services and procedures that are subject to prior authorization requirements? • Are electronic 837 claims accepted in the 5010 format (now)? • Are electronic remittance 835 available now and do they include adjustments with payments • How is eligibility determined? Online or by phone? AGE IS MORE IMPORTANT 0-30 A/R Balance 31-60 61-90 91-120 120+ $212,245.60 $77,823.39 $56,598.83 $7,074.85 $0 60% 22% 16% 2% 0% Balance $353,742.66 WHERE IS REVENUE MADE AND LOST? Revenue Made Revenue Lost Training is ongoing When rules change and no-one notices Proactive practices Fall behind – timely filing ~30-365 A/R Follow up – Denial Management No A/R management - Rebilling Front desk skilled interpreting benefits and promoting enrollment Ineffective front end management Tracking and measuring the right things Accountability is lacking Policies, Procedures and Tasks are done Everyone is doing their own thing RADAR 2012 ICD-10 Terminology & Anatomy/Physiology Process Improvements Improve denial management process MEANINGFUL USE OF E H R Stage 1 requirements ACA Hospitals outcome based payment (10/01/12) “Value Based Payment – VBP” 2013 2014 2015 10/01/2013 -2014 ICD-10 compliance date I10 coding training for providers, support and coder/billers Stage 2 requirements Payment bundling for outpatient with inpatient Insurance Exchanges & 133% Newly Eligible's Stage 3 requirements Paying physicians based on “value” not volume http://www.healthcare.gov/law/timeline/ ELIGIBLE PROFESSIONALS: MEDICARE INCENTIVE PAYMENT EXAMPLE Amount of Payment Each Year of Participation Calendar Year EP Receives a Payment CY 2011 CY 2012 CY 2013 CY2014 CY 2015 and later CY 2011 $18,000 CY 2012 $12,000 $18,000 CY 2013 $8,000 $12,000 $15,000 CY 2014 $4,000 $8,000 $12,000 $12,000 CY 2015 $2,000 $4,000 $8,000 $8,000 $0 $2,000 $4,000 $4,000 $0 $44,000 $39,000 $24,000 $0 CY 2016 TOTAL $44,000 ELIGIBLE PROFESSIONALS: MEDICAID INCENTIVE PAYMENT EXAMPLE 1st Calendar Year EP Receives a Payment Amount of Payment Each Year if Continues Meeting Requirements CY 2011 CY 2011 $21,250 CY 2012 $8,500 $21,250 CY 2013 $8,500 $8,500 $21,250 CY 2014 $8,500 $8,500 $8,500 $21,250 CY 2015 $8,500 $8,500 $8,500 $8,500 $21,250 CY 2016 $8,500 $8,500 $8,500 $8,500 $8,500 $21,250 $8,500 $8,500 $8,500 $8,500 $8,500 $8,500 $8,500 $8,500 $8,500 $8,500 $8,500 $8,500 $8,500 $8,500 CY 2017 CY 2012 CY 2018 CY 2013 CY 2019 CY 2014 CY 2020 CY 2015 CY 2021 TOTAL CY 2016 $8,500 $63,750 $63,750 $63,750 $63,750 $63,750 $63,750 Focus points… • Fundamentals • Change • Goal • Similarity of processes • 3rd Party revenue • Work to do • It’s why we are already here