File
advertisement

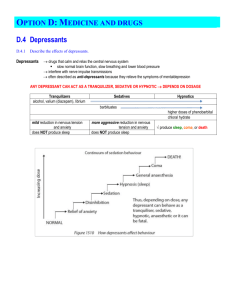
Pharmacology of Alcohols Dr Javaria Arshad History and overview • Arabs developed distillation about 800 C.E • Word Alcohol derived from Arabic for ‘something subtle’ • Alcohol abuse • Alcoholic content of beverages ranges between 4% to 6% • Wine contain 10% to 15% Alcohol. • In USA 75% of adult population drink alcohol regularly Alcoholism • People continue to drink alcohol in spite of adverse medical or social consequences • Complex disorder with genetic as well as environmental determinants • Each year tens of thousands of children are born with morphologic and functional defects because of maternal alcohol intake • Alcohol abuse: Psychiatric diagnosis describing the recurring use of alcoholic beverages despite its negative consequences Alcohol dependence: Physical dependence on alcohol (tolerance and signs and symptoms upon withdrawal ) structure • Ethanol, CH3 CH2 OH • Methanol, Methyl alcohol • Ethylene glycol Routes of Administration • Topical • Inhalation • Intravenous injection • Oral ingestion Pharmacokinetics • Ethanol rapidly absorbed from stomach and intestine • PPL are reached in 30 mins in empty stomach. • Distributed to total body water (0.5-0.7 L/Kg) • In CNS concentration rises quickly, it can readily cross biologic membranes. Metabolism • Zero order kinetics (independent of time and concentration of drug) • Constant amount of drug is eliminated in unit time • Two pathways of alcohol metabolism • 1- Alcohol dehydrogenase pathway • 2- Microsomal ethanol oxidizing system (MEOS) • Gastric metabolism of ethanol is lower in women than in men Alcohol dehydrogenase pathway • Alcohol dehydrogenase enzyme present in liver, brain and stomach • Converts alcohol to acetaldehyde and NAD+ is converted to NADH • Excess NADH production lead to metabolic disorders, lactic acidosis and hypoglycemia Microsomal ethanol oxidizing system • Mixed function oxidase system (MFO) • MEOS work when ethanol concentration rises above 100 mg/dl. • During chronic alcohol consumption, MEOs activity is induced. • As a result metabolism of other drugs which are metabolized by cytochrome P450 increases. Acetaldehyde metabolism • Acetaldehyde is oxidized in liver by mitochondrial NAD dependent aldehyde dehydrogenase • Acetate is formed which is further metabolized to CO2 and water • Disulfiram inhibit this metabolism. • Facial flushing, nausea, vomiting, dizziness and headache • Metronidazole, cefotetan and trimethoprim Excretion • Small but a consistent proportion of alcohol is excreted through lungs. • ‘Breath alcohol test’ serve as a basis for a legal definition of ‘ driving under the influence’ . Breath alcohol test • Ratio of ethanol in end-expiratory alveolar air and ethanol in the blood is relatively consistent. • Blood ethanol levels in humans can be estimated by measurement of alcohol levels in expired air • Legally allowed BELs are set below 80mg% Pharmacodynamics • • • • • GIT CVS CNS Effects on disease processes Effects on prenatal development CNS • Alcohol is a CNS depressant • Disturbs the fine balance between excitatory and inhibitory influences in the brain. • Sedation, relief of anxiety. • Slurred speech, ataxia, impaired judgment and disinhibited behaviour (drunkenness) • Coma, respiratory depression and death Molecular mechanism • Effect membrane proteins that participate in signaling pathways, neurotransmitter receptors for amines, amino acids, opioids and neuropeptides. • Na+, K+ ATPase • Adenylyl cyclase • Phosphoinositide- specific phospholipase C. • Enhance the action of GABA at GABAA receptors • Ethanol inhibits the ability of glutamate to open the NMDA subtype of glutamate receptors. Related to cognitive functions learning and memory Heart and other organs` • Significant depression of myocardial contractility. • Vasodilatation • Relaxation of uterine muscles. Chronic Alcohol Consumption • Tissue damage result from direct effect of ethanol and the effect of metabolite. • Liver: Alcoholic fatty liver Alcoholic hepatitis Cirrhosis Liver failure • Increased oxidative stress coupled with depletion of glutathione, damage to mitochondria and potentiation of cytokine induced injury • Chronic pancreatitis • Gastritis leading to blood and plasma protein loss CNS • Tolerance and dependence: Alcohol withdrawal leads to hyperexcitability, seizures, toxic psychosis and delirium tremens (hallucinations, delirium , fever and tachycardia) Psychological dependence. Neurotoxicity: Neurologic deficits. Generalized symmetric peripheral nerve injury. Wernicke-Korsakoff syndrome • Paralysis of external eye muscles, ataxia and a confused state that can progress to coma and death • Thiamine deficiency + alcoholism • korsakoff’s psychosis • Impair visual acuity CVS • • • • • Dilated cardiomyopathy Ventricular hypertrophy and fibrosis. Atrial and ventricular arrhythmias Hypertension Coronary heart disease (moderate alcohol consumption prevent heart disease) • Increased risk of hemorrhagic and ischemic stroke Blood • Inhibit the proliferation of cellular elements in bone marrow. Endocrine system and electrolyte balance Gynecomastia, testicular atrophy. Ascites, edema and effusions. Chronic alcohol use lead to increase risk of cancer of mouth, pharynx, larynx, esophagus and liver Clinical uses of alcohol • Dehydrated alcohol may be injected in close proximity to nerves and sympathetic ganglia to relieve long standing pain. • Systemically ---- poisoning by methyl alcohol and ethylene glycol Fetal Alcohol Syndrome • Chronic maternal alcohol abuse • Fetal liver has no alcohol dehydrogenase activity • Intrauterine growth retardation. • Microcephaly • Poor coordination • Underdevelopment of midfacial region • Minor joint anomalies Alcohol-Drug interactions • Induction of cytochrome P450 enzyme • Liver toxicity enhanced with parracetamol • Phenothiazines, tricyclic antidepressants and sedative hypnotics. • Additive CNS depression with sedativehypnotics. Acute alcohol intoxication • Gidddiness , muscle relaxation, impaired judgement ------ nystagmus, failing vital signs, coma and death. Management of acute alcohol intoxication • • • • • Prevent respiratory depression. Prevent aspiration of vomitus. Glucose Thiamine (Wernicke-Korsakoff syndrome) Electrolyte solutions Management of alcohol withdrawal syndrome • Substituting a long-acting sedative hypnotic drug for alcohol and then gradually reducing the dose of drug. • Benzodiazepines are preferred. Treatment of alcoholism • Naltrexone • Acamprosate • Disulfiram Cause discomfort in alcoholics Flushing, throbbing headache, nausea, vomiting, sweating, hypotension and confusion. Inhibit aldehyde dehydrogenase Acetaldehyde accumulates Naltrexone • Related to naloxone Opioid-receptor antagonist naloxone • It is given after detoxification and for several months Acamprosate • An analogue of GABA • Decreases Alcohol intake Methanol • Used in industrial production of synthetic organic compounds and as a constituent of many commercial solvents • Accidental ingestion occur when it is misguidedly ingested as ethanol substitute • Absorbed through skin, respiratory and gastrointestinal tract and well distributed • Oxidized to formaldehyde, formic acid and CO2 • Visual disturbances (like being in a snow storm) lead to blindness • Bradycardia, prolonged coma, seizures and acidosis Treatment Fomepizole (alcohol dehydrogenase inhibitor) Bicarbonate for metabolic acidosis Ethylene glycol • Used as heat exchangers in antifreeze formulations • Transient excitation followed by CNS depression , metabolic acidosis and renal insufficency • Fomepizole I/V administration •Thank you



![Alcohol metabolism []](http://s2.studylib.net/store/data/010236384_1-561c51a634a4190fbc74d978632ccd47-300x300.png)