Pharmacology 11b – Alcohol(1)
advertisement
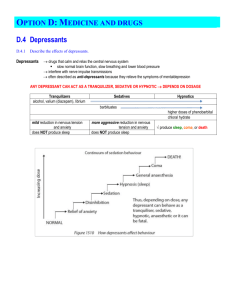
Pharmacology 11b – Alcohol Anil Chopra 1. Describe the dose-dependent effects of acute ethanol ingestion on (a) CNS function and put forward theories to explain the underlying mechanism of action (b) Other body systems 2. Describe the consequences of long-term excessive ethanol consumption 3. Outline the main pharmacokinetic features of ethanol 4. Explain how tolerance to the effects of ethanol is produced. What symptoms are associated with alcohol withdrawal in dependent subjects Alcohol Alcohol = ethanol (C2H5OH 1 unit = 8g or 10ml %ABV x 0.78 = g alcohol/100ml Units = %ABV x volume (ml) / 1000 Recommended maximums – Men = 21 units, Women = 14 units a week Responsible for 1/3 of all A&E admissions – costs £3bn a year Alcohol Related Injuries 28,000 hospital admissions/year 33,000 deaths/year Cost to NHS; £3bn/year 1/3 of all A&E attendances Dosing In order to calculate the amount of alcohol drunk, you multiply the alcohol by volume by 0.78. ABV x 0.78 = g alcohol/100ml Therefore 1 unit is 10ml or 8g of absolute ethanol. The supposed “safe level” is: - Men 21 units/week - Women 14 units/week 20-40mg/ml (Minimal effects) Up to 50mg/ml Up to 80mg/ml (Legal driving limit) Up to 150mg/ml (90% - gross intoxication) 300mg/ml (Coma) 4-500mg/ml (Death) Likelihood of car accident x4 x 25 Alcohol is absorbed in the stomach (20%) and in the duodenum (80%). First pass metabolism occurs in the liver (90%) and in the GI tract (10%): Alcohol (alcohol dehydrogenase) (mixed function oxidase) acetoaldehyde Females have 50% less alcohol dehydrogenase in their stomachs as well as less circulating water. Second pass metabolism occurs entirely in the liver: Acetoaldehyde (aldehyde dehydrogenase) Acetic Acid Effects of Alcohol Ethanol itself has a low pharmacological potency. Effects generally start occurring at 40-100mg/100ml – 10-20x this can be lethal. Longer chain alcohols are more lipid soluble and so would be more potent but are not in drinks as do not dissolve in water. Central Nervous System Its acute effects are as a CNS depressant. Its initial stimulatory effect results from depression of the INHIBITORY control pathways. The excitability may depend on the patients personality or the setting which they are in. It does this by: - increasing amounts of pre and post synaptic allopregnenolone (which has inhibitory effects on neurones), - decreasing allosteric modulation of NMDA receptors (NMDA acts like glutamate) - decreasing Ca2+ release - enhancement of GABA-mediated inhibition. Some areas of the brain are more sensitive than others: Cortical regions – impairs sensory function (mood changes, memory loss, loss of co-ordination. Euphoria, increased self confidence) and impairs motor function (slurred speech, prolonged reaction time, loss of co-ordination) Corpus callosum – passes info from left (rules, logic) to right (impulse, feelings) and vice versa Hippocampus – role in memory Hypothalamus – controls appetite, temperature, emotions and pain sensation Cerebellum – movement and co-ordination Basal ganglia – time perception Reticular activating system - conciousness It induces euphoria mainly via its effects on the ventral tegmental area. Also leads to - memory loss - mood changes - reduced powers of discrimination and concnentration Cardiovascular System It can cause cutaneous (near the skin) dilation of blood vessels by decreasing Ca2+ entry into smooth muscle cells and increasing the production of prostaglandins. It has been proven that in moderate drinkers, it is shown to have positive effect on HDL cholesterol and a reduction in mortality from heart disease and thrombosis due to its effects on reducing platelet aggregation and tPA (tissue plasminogen activator) levels. Chronic effects: » Atrial arrhythmias: o Prolongation of conductance times and increase in refractory period o Acute negative inotropic effects mediated by direct interaction with cardiac muscle cells » Alcoholic cardiomyopathy: o Myocyte and nuclear hypertrophy, interstitial necrosis and myocyte necrosis Motor Function - Slurred speech - Prolonged reaction delay - Loss of co-ordination Endocrine System Its acute effects are diuresis (polyuria) caused by reduced vasopressin secretion. In chronic use however it can lead to increase ACTH secretion (therefore increases in cortisol), as well as decreases in testosterone production (can lead to feminisation). Gastro-Intestinal Tract Chronic use is shown to cause damage to gastric mucosa and increase the risk cancer development. Acute: Increased salivary and gastric acid secretions: Taste increase salivary production Irritant effect → histamine release → increases gastric acid (may also be due to fermentation products) Also due to stimulation of sensory nerve endings Chronic: Direct damage to gastric mucosa – directly related to dose → increased risk of peptic ulcers Increased gastric bleeding – gastrititis Effects on lipid metabolism/platelet formation: In small doses – reduced thrombosis formation → reduced risk of atherosclerosis/ischaemic heart disease MOA: Increased HDL → increased cholesterol esterification → reduced plaque formation → reduced thromboxane A2 → reduced platelet aggregation Effect on Foetal Development Foetal alcohol syndrome – if mother drinks at least 4 units/day Abnormal facial development (and other anatomical abnormalities) Growth retardation Mental retardation Caused by inhibition of cell division and migration Liver Alcohol has few acute effects on the liver, however its chronic use can lead to fatty liver. In order to metabolise alcohol, its is first oxidised to acetaldehyde, which results in the production of NADH. The excess NADH can have a number of fates. It can be used to in lipogenesis, this results in more triglycerides in liver cells. It can also be used in the electron transport chain to produce ATP from ADP. This therefore means that the Krebs cycle has to slow down and therefore other fats and glucose cannot be metabolised. It can also be used in the conversion of lactic acid to pyruvic acid. This results in fat vesicles accumulating in liver cells which results in fatty liver. The acetaldehyde produced can also leak into the blood and cause a decrease in normal metabolism. The free radicals produced can also lead to an increase in the production of certain cytokines (IL-6 and TNFα) and ultimately liver inflammation – hepatitis. The increase in activation of fibroblasts and decrease in hepatocyte regeration can also cause liver cirrhosis, characterised by the replacement of liver tissue with scar tissue. Pharmacokinetics Uncharged and so highly lipid soluble Rapidly absorbed through the mucus membranes of the stomach and gut (slowed by food) Rapidly distributed throughout body tissues – dependant on tissue blood flow Substantial amounts removed in first pass metabolism Demonstrates saturation kinetics – rapid absorption → high portal vein concentration → liver enzyme saturation → escape into systemic circulation 90% metabolised in body (mainly by liver) 5-10 % is excreted unchanged in the urine (variable) and expired by the lungs (constant – 80mg/ml in blood = 35µg/100ml of expired air – hence breathalysers Metabolism of ethanol Ethanol is 90% metabolised in the body – mainly liver LIVER Ethanol C2H5OH (NAD+) 75% Alcohol Dehydrogenase (NADH) (NAD+) 75% (NAD+) 25% Mixed function oxidase Acetaldehyde CH3CHO Aldehyde Dehydrogenase Induction (NADH) 25% Aldehyde Oxidase (+ O2) EXTRA-HEPATIC (NADH) Acetic acid CH3COOH 1. Disulfiram (aversion therapy) 2. Genetic variant (50% asians) Mixed function oxidase can be increased/induced by exposure to alcohol and other compounds NAD+ is needed as a co-factor for all reactions Disulfiram inhibits aldehyde dehydrogenase → high levels of acetaldehyde → flushing, tachycardia, hyperventilation, panic/distress. Used in aversion therapy for recovering alcoholics – no effect without alcohol 50% of Asians do not have aldehyde dehydrogenas → therefore alcohol intolerant Also rare variation in alcohol dehydrogenase → increased alcoholism risk Tolerance to the effects of alcohol occurs within 1-3 weeks of continuous administration Due to: o Pharmacokinetic tolerance o Tissue tolerance o Cellular adaptation Dependence = overpowering craving for alcohol Physical withdrawal from dependence is characterised by: o Tremor o Hallucinations o Convulsions o Behaviour disturbances o Nausea o Fever The Hangover The symptoms peak as blood alcohol level tends toward 0: Nausea: caused by vagus stimulation to the vomiting centre. Headache: caused by vasodilation Fatigue: caused by sleep deprivation Tremors: “rebound” – increased glutamate production by neurones to compensate for its inhibition by the alcohol. Polyuria: caused by decreased vasopressin secretion.





![Alcohol metabolism []](http://s2.studylib.net/store/data/010236384_1-561c51a634a4190fbc74d978632ccd47-300x300.png)