File - Respiratory Student Insight
advertisement

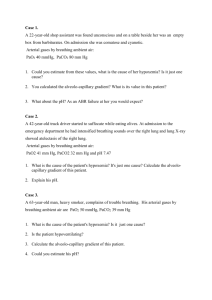
Study Guide Chapter 41- Egan’s What are the criteria for a diagnosis of respiratory failure? Inadequate alveolar ventilation pH under 7.35, PaCO2 over 45mmHg Inadequate lung expansion VT under 5ml/kg, VC under 10ml/kg RR over 20 or under 8 Inadequate muscle strength MIV under -20cmH2O, VC under 10ml/kg MVV less than 2x the VE Hypoxemia A-a gradient over 350mmHg P/F ratio under 200 PaO2 under 60mmHg PaCO2 over 45mmHg 350-450 10-25mmHg Diffusion defect V/Q mismatch Shunt Alveolar hypoventilation Low FiO2 A shunt will NOT be affected by O2. What is the normal P/F ratio? What is the normal A-a gradient on room air? What are the causes of hypoxemia? How do you tell if the problem is a shunt or V/Q mismatch via oxygen? The most severe sign of hypoxemia is Which disease is associated with perfusiondiffusion impairment? What is the normal A-a gradient on 100% O2? What happens to A-a gradient for a shunt and a V/Q mismatch? How do you treat a shunt? CNS dysfunction; comatose Cirrhosis of the liver 25-65mmHg Shunt = increase V/Q mismatch = increase With positive pressure, either noninvasive or invasive Type I-Hypoxemic = PaO2 under 60mmHg Type II-Hypercapnic = PaCO2 over 45mmHg Increased exposure Impaired respiratory control Neurological disease Increased WOB The decrease capacity of a rested muscle to generate force and decrease endurance Disease = Neuromuscular, COPD Conditions = Obesity, kyphoscoliosis Condition in which there is loss of the capacity to develop force or velocity of a muscle resulting from muscle activity under load, which is reversible by rest Conditions = hypoxemia, increase WOB, increase strength of muscle contraction, decrease muscle Classification of ABG of the 2 different ventilatory failures What are the causes of hypercapnic ventilatory failure? What is muscle weakness? What diseases cause this? What is muscle fatigue? What diseases cause this? 1 Study Guide Chapter 41- Egan’s efficiency, decrease inspiratory muscle blood flow, poor nutrition, and inability of a muscle to extract energy from supplied substrates Central = exertion-induced reversible decrease in central resp. drive Transmission = exertion-induced reversible impairment of transmission of neural impulses Contractile = reversible impairment in the contractile response to a neural impulse in an overload muscle Diseases= obstruction lung disease COPD Asthma Conditions= upper airway obstruction Obesity-hypoventilation Pneumothorax Severe burns Chest wall disorders Kyphoscoliosis Ankylosing spondylitis HCO3 What are the 3 types of muscle fatigue? What diseases cause increased WOB? How do you determine if it is an acute or chronic respiratory failure? Why do the kidneys keep HCO3? What is the cardinal sign of increased WOB? If you have the FiO2 and the PaO2 of several patients, how would you tell who was worse? In acute hypercapnic failure how much does the pH decrease? In chronic hypercapnic failure how much does the pH decrease? What should the NIF/MIV value be? If a patient’s NIF value is not large enough, what does this mean? What values can be tested at the bedside to determine if a patient needs ventilatory support? How is alveolar ventilation assessed? How is oxygenation determined? to increase pH Increased PaCO2 P/F ratio *Bigger is better* pH decreases 0.08 for every 10mmHg increase in PaCO2 pH decreases 0.03 for every 10mmHg increase in PaCO2 at least -20cmH2O Ventilatory muscles are not strong enough VT, VC, RR, VE pH and PaCO2 PAO2 equation (PB-PH2O)xFiO2 - (PaCO2 x 1.25) Respiratory center is not responding Signal is not getting to muscles Lungs and chest wall are incapable of providing adequate ventilation NIF/MIV, MVV, MEP, FRC VE (minute ventilation) VD/VT % (dead space vol/tidal vol %) physiological = natural imposed = artificial CPAP for the pressure What 3 things increase PaCO2? How is muscle strength determined? What is used to determine increased WOB? The 2 types of WOB are If a patient has CHF, what should be done? 2 Study Guide Chapter 41- Egan’s If a patient has ARDS, what should be done? If a patient has increased ICP, what should be done? Who is at the greatest risk for auto-PEEP? What is indicated by a white radiograph? What are the indications for ventilation in Type I failure? What are the indications for ventilation in Type II failure? Intubate with low volume and high pressure Hyperventilate COPD patients Shunt b/c of hypoxemia (ARDS) P/F ratio increased FiO2 and PEEP increased PaCO2 decreased pH increased HCO3 (due to compensation by kidneys) NIF/MIP MEP What measures inspiratory muscle strength? What measures cough strength and ability to maintain patent airway? What is dead space? What is a shunt? What is the normal anatomic shunt? Ventilation without perfusion Perfusion without ventilation 2-3% 3