Frank Röhricht Body Psychotherapy
advertisement

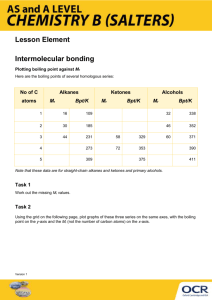
Therapeutic processes and outcomes in body psychotherapy research Dr. Frank Röhricht MD Unit for Social and Community Psychiatry Queen Mary University of London London / UK Crossing Borders: Symposium: “other therapy” EAP congress 2008 in Nice Integral self-therapy (“novel approach”) Utilization of therapeutic dogs for depression and anxiety Autogenic psychotherapy Packing therapy in children and adolescents with autism: “Wrapping the patient with his under-clothes, using towels previously wet in clod water. The patient is then wrapped with blankets to help the body warm up.” There is more wisdom in your body than in your deepest philosophy. -Friedrich Nietzsche. German classical Scholar, Philosopher and Critic of culture, 1844-1900. Outline Some basic facts Findings from other research areas relevant for the evaluation of BPT Outcomes from research re efficacy and processes in BPT 1. overview, 2. examples (SD/schizophrenia) Outlook/The way forward Body psychotherapy – basic facts Google: >25000 hits (first 765 pages relevant) USABP (> 500 members), peer-reviewed journal EABP (>600 members in 21 countries) 8th International Congress of BPT 11/2008 in Paris 3x MA Somatic Psychology in USA Medline: 20 hits (one relevant); PsyInfo 179 (89) Term BPT not fully established No state accreditation Not represented on mainstream congresses On the outside: Focussing Hakomi Functional Relaxation Biodynamic psychotherapy Psychomotricity Body mind approach Tai-Chi Analytical Body psychotherapy Eutonie Character Analytic Vegetotherapy Biosynthesis Dance & Movement Rolfing Therapy Thymopraktik Concentrative Movement therapy Feldenkrais BodyBehaviour therapy Yoga Bioenergetics Core-Energetics Shiatsu What is Body Psychotherapy? The common underlying assumption is that the body is the whole person and there is a functional unity between mind and body. (EABP) Based on an holistic view of the human being, on the unity of body and mind, psychomotricity integrates the cognitive, emotional, symbolical and physical interactions in the individual’s capacity to be and to act in a psychosocial context. (EFP) DMT is the psychotherapeutic use of movement and dance through which a person can engage creatively in a process to further their emotional, cognitive, physical and social integration. (ADMT-UK) Therapist’s perspective I am doing a good job, because my patients get better I am an experienced therapist and know best what to do when For BPT: “I can sense the blocked energy, and I will make it flow again” Randomised controlled trial of physiotherapy versus advice for low back pain (N=286) Oswestry disability index P=.17 2-months P=.31 P=.28 6-months 12-months Frost et al. BMJ 2004 Improvement 3.0 2.5 2.0 1.5 1.0 0.5 0.0 -0.5 -1.0 -1.5 -2.0 -2.5 -3.0 Advice only (N=142) Worsening Mean Change From Baseline Physiotherapy (N=144) RCT physiotherapy/advice for low back pain: Patient’s perceived benefit Patient perceived benefit P=.006 P=.025 6.0 5.5 5.0 4.5 4.0 3.5 3.0 2.5 2.0 1.5 1.0 0.5 0.0 Improvement Mean Change From Baseline P=.001 2-months 6-months Physiotherapy Frost et al. BMJ 2004 12-months Advice only Re-Search Scientific research relies on the application of the scientific method, a harnessing of curiosity. This research provides scientific information and theories for the explanation of the nature and the properties of the world around us. It makes practical applications possible. . Probability is the likelihood or chance that something is the case or will happen. Wikipedia – the free encyclopaedia From inside What do we know already? – a systematic overview: Thematic emphasis for theory of Body psychotherapy Developmental psychology (body-ego) Phenomenology of body experience Specific illness characteristics (i.e. Body image disorders) Methodological considerations re Intervention technique (Affective) neuroscience and motor behaviour Neuroscience and Psychotherapy “From the perspective of neuroscience, psychotherapy can be understood as a specific kind of enriched environment designed to enhance the growth of neurons and the integration of neural networks” Cozolino, 2002 Neural growth and integration on psychotherapy are enhanced by: 1. Establishment of a safe and trusting relationship 2. Gaining new information and experiences across the domains of cognition, emotion, sensation, behaviour 3. Simultaneous or alternating activation of neural networks, that are inadequately integrated 4. Moderate levels of stress or emotional arousal alternating with periods of calm and safety. 5. Integration of conceptual knowledge with emotional and bodily experience. Body psychotherapy How does it work? – the intervention strategy: Intervention techniques common to all BPT’s Body/experience regarded as important therapeutic medium Therapeutic relationship centered around immediate self/body experience, involving touch and psychomotor expression Gestures, posture, spontaneity and movement pattern therapeutically utilised Emphasis on ‚healthy‘ personality traits, ressources, self-regulation Working with tension dynamics and affect regulation Basic hypotheses, BPT offers/acts upon: specific tools for specific problems, symptoms a unique, interactive therapeutic relationship a multidimensional approach BPT operates at the centre of emotional processing and motor (expressive) behaviour BPT relates directly and intrinsically to strengths, capabilities and creativity Outline Some basic facts Findings from other research areas relevant for the evaluation of BPT Outcomes from research re efficacy and processes in BPT 1. overview, 2. examples (SD/schizophrenia) Outlook/The way forward Anxiety disorder Body perception negatively correlated with anxiety levels (Compton 1969, Röhricht & Priebe 1996) Phobic anxietydepersonalisation syndrome (Tucker et al. 1973, Noyes et al. 1977) Body image satisfaction low in anxiety patients (Marsella et al. 1981, Löwe & Clement 1998) Bermuda-Triangle: Anxietytension headache-anger Grounding, body-awareness, boundary articulation, fightflight impulses Depression Range of somatisation symptoms (chest pressure, pain, etc.) Motor retardation, lack of drive energy and motivation Negative body cathexis, somatic depersonalisation and boundary loss correlated with degree of anxiety symptoms (Röhricht et al. 2002) Anorexia Nervosa: Severe body image aberration, overestimation of body sizes Negative body cathexis with hostile attitudes Control and manipulation of bodily functions (e.g. excessive exercising, vomiting) Movement analysis: What else do we know? Neuropsychology: movement and emotional experiences are biologically and experientially associated ( ‘a moving experience’ Trimble 1997) Outline Some basic facts Findings from other research areas relevant for the evaluation of BPT Outcomes from research re efficacy and processes in BPT 1. overview, 2. examples (SD/schizophrenia) Outlook/The way forward Evaluation of BPT-1 Numerous cohort studies with various methods 1970 - 1998 in healthy samples, neurosis, drug abuse: increase in body satisfaction, self-perception, self-esteem and muscular tension (Fisher 1996) Dance/Movement therapy vs. waiting list: Reduction in depression and anxiety for BPT group (Brooks & Stark 1989) Movement therapy for patients with depression, neurosis, mania, schizophrenia: general wellbeing improved, complaints reduced in BPT group, no effect on specific symptoms (Weber et al. 1994) Dance/Movement therapy vs. waiting list in depression and anxiety 80 75 70 pre BEC pre CG post BEC post CG 65 60 55 50 SOM O-C ins-soc DEPR ANX Inpatient body oriented psychotherapy in Eating disorder Evaluation of the Effectiveness of BodyPsychotherapy in Out-Patient Settings EEBP-study main outcome: Specific examples: Evaluation of BPT in psychosomatic disorders Bioenergetic exercises in inpatient treatment of Turkish immigrants with chronic somatoform disorders: A randomized, controlled study Bioenergetic exercises versus : mean changes pre-post P=.28 3.0 2.5 2.0 1.5 1.0 0.5 0.0 -0.5 -1.0 -1.5 -2.0 -2.5 -3.0 SCL-90 scales BEC CG Frost et al. BMJ 2004 Improvement SCL-90 P=.31 Worsening Mean Change From Baseline P=.17 Functional relaxation versus Terbutaline/Placebo in Asthma 60 days before/after therapy Diagnostic headache diary Change of intensity and duration pain Functional relaxation versus unspecific isotonic relaxation in chronic tension headache 16 14 12 10 8 6 4 2 0 15.7 11.711.4 13 10.1 9.8 5.8 UIR eFR 0.6 pain days before pain days after pain hours before pain hours after Pilot study: Bodymind approach (group work) for patients with medically unexplained symptoms CORE-OM mean scores for subscales MYMOP mean scores for each element from baseline to follow-up baseline to follow up Payne et al. in preparation Specific example 2: Evaluation of BPT in schizophrenia CMT-study, Jung 2002 N=18 acute schizophrenia inpatients BPI: Gesunde, Schizophrene im Verlauf n=18 120 BPI in % 110 100 90 80 1 Gesunde 2 Schiz Aufnahme 3 Schiz 4 Wochen Evaluation of BPT in schizophrenia Body-ego-technique” vs. Music therapy: improvement of psychopathology scores and sign. > re. affective contact as well as motility (Goertzel et al. 1965) Movement and Drama therapy vs. SC in chronic sch. (RCT): for BPT sign. improvement of social behaviour and restlessness; psychopathology better in both groups (Nitsun et al. 1974) Body centred PT vs. OT in acute schizophrenia (RCT): only for those patients with body image disorder in BPT group sign. > improvement of ego-disturbances (Maurer 1976) Body perception training in schizophrenia: improved social competencies/body size perception, reduced anxiety (Seruya 1977) Changes BPI following Concentrative movement therapy/TAU BPI im Verlauf: Patiennten ohne KBT 120 120 110 110 BPI in % BPI in % BPI im Verlauf: KBT-Teilnehmer 100 100 90 90 80 80 Kopf Rumpf KBT Aufn. KBT 4 Wo Beine Gesunde Kopf Rumpf N-KBT Aufn. Jung 2002 N-KBT 4 Wo Beine Gesunde From A to Z Negative symptoms in schizophrenia Sass and Parnass : These symptoms (or rather signs, since they mostly involve behavioral observations) include poverty of speech, affective flattening, apathy and anhedonia, and a general inattentiveness to the world. empirical research shows that patients who display flat affect actually report an intense emotional reactivity that contradicts their lack of overt affective expression (Bouricius 1989; Berenbaum and Oltmanns 1992; Kring, Kerr, Smith et al. 1993; Hurlbut 1990) Hypotheses: How can BPT potentially address negative symptoms in schizophrenia Self-defensive strategies, active withdrawal in response to perceived threats and/or disintegrative ego-processes (“Totstell-Reflex”)??? Hence: 1. ego-consolidation, enhanced body perception (periphery) boundary articulation as precondition for: 2. enhanced motor expression/emotional processing = enhanced social participation/QoL Demographic characteristics BOT group N=24 38.9 (21-55) 12.1 (2-31) 3.7 (1-12) 16.4 (10-21) 12/12 Age Duration of illness No admissions School left Gender f/m SC group N=21 37.7 (20-55) n.s. 10.8 (2-30) n.s. 4.4 (1-12) n.s. 17.0 (15-22) n.s. 11/10 n.s. Clinical baseline characteristics BPT group N=24 16.5 (7-24) 23.4 (16-35) 39.1 (26-54) 11.4 (6-15) 11.6 (0-23) 49.3 (28-70) 1.4 (0-6) PANSS-pos PANSS-neg PANSS-gen Anergia EPP-total MANSA EPS-total SC group N=21 13.1 (7-29) n.s. 24.6 (12-34) n.s. 38.6 (21-62) n.s. 11.8 (7-16) n.s. 8.2 (0-23) n.s. 47.8 (28-62) n.s. 1.7 (0-8) n.s. Outcome measures 1 PANNS-negative scores 25 24 23 22 21 20 19 18 17 16 15 24.6 23.4 23.3 23.2 18.9 initial after treatment 6-month follow-up 18.2 P<.001 T=5.3, df=22 BPT (N=24) n.s. SC (N=21) Outcome measures 2 BPRS anergia scores 15 14 13 12 11 10 9 8 7 6 5 11.9 11.4 8.9 12 11.1 initial after treatment 6-month follow-up 8.4 P<.001 T=5.3, df=22 BPT (N=24) SC (N=21) Outcome measures 3 Reduction psychopathology scores / % 20 19.4 24.1 15 8.4 9.1 10 5 3.9 3.6 3.2 0 -5 -10 BPT SC 1.4 PANSS-neg Anergia PANSS-pos PANSS-gen Outcome measures 4 MANSA scores 60 55 50 52.9 49.3 49.4 47.8 49.8 51.1 initial after treatment 6-month follow-up 45 40 35 30 n.s. BPT n.s. SC Outcome measures 5 clients assessment of treatment 40 38 36 34 32 30 28 26 24 22 20 44 39 36 31 P=.07, t=1.9 df=25 CAT after treatment P<.05, t=2.4 df=27 HAS-P after treatment 32 25 P=.05, t=2.0 df=27 HAS-T after treatment BPT SC Outcome measures 6 Reduction Ego-psychopathology scores In experimental group significant reduction in EPP-scores pre/post for the subscales: demarcation, consistency, activity and body (p<.05, t=2.2-3.6, df=23) No significant reduction in EPP-scores within the control group Predictors of Treatment Response Dependent variable: % reduction BPRS anergia: Independent variables: No of attended sessions, number prev. hospitalisation, age, gender, VAS-scores, EPP-scores, employment status, age leaving education, MANSA-scores, PANSS-scores at admission 85% of total variance explained by: onset of illness (beta .57, p<.01), EPP-demarcation (beta -.57, p<.01) and VAS-small (beta .35, p<.05) Summary of findings: The next step: BPT-RCT Assessments 2 Mediating/Process measures: Movement Psychodiagnostic Interview (MPI), (analysis of movement behaviour on the basis of videotapes from assessment interview) Rating scale for emotional blunting (SEB) Differential Emotions Scale (DES−IV) Semi−structured phenomenological interview Video observation of therapy sessions Outline Some basic facts Why is there a need for more/other and nonverbal/BPT therapies Findings from other research areas relevant for the evaluation of BPT Outcomes from research re efficacy and processes in BPT Outlook/The way forward Advances: Neuroimaging and BPT Process research: What are the active ingredients? Differential therapeutics When is which therapy working better? When is combined therapy working better? Which therapists characteristics work? BPT Thank you!