The International Center for Spinal Cord Injury, Hugo W. Moser
advertisement

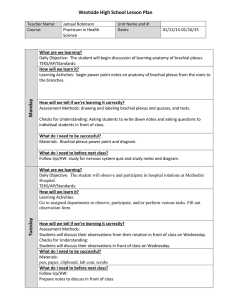
Novel Approaches to Management of Brachial Plexus Injuries Jennifer Wingrat, ScD, OTR/L1, Rebecca Martin, OTR/L, OTD1, Glenaliz Bosques, MD3, Daniel Becker, MD1,2 The International Center for Spinal Cord Injury, Hugo W. Moser Research Institute at Kennedy Krieger¹, The Johns Hopkins University School of Medicine2, Baltimore, Maryland; University of Texas and TIRR Memorial Hermann Hospital3, Houston, Texas INTRODUCTION PARTICIPANT Neonatal brachial plexus injuries (NBPI) account for 0.38-5/1000 live births1. While 60% of infants recover function by 6 months of age2, 30% are left with residual deficits resulting in decreased range of motion, strength, sensation, and overall functional use of the affected extremity. Traditional OT intervention for patients with brachial plexus injuries includes active, active assisted, and passive ROM, splinting, and therapeutic taping4, often within the framework of developmental play. While these methods are an important part of the rehabilitation process, more aggressive methods may provide greater benefits. Activity-Based Rehabilitation (ABR) is the use of repeated, near normal activity to optimize the nervous system for recovery while offsetting chronic complications incurred as the result of paralysis. It is a more aggressive therapy approach that differs from traditional therapies in frequency and intensity. The goals of ABR are to optimize development, decrease risk of developmental apraxia, and maximize growth (limb length and muscle bulk). ABR can be an effective approach to treating brachial plexus injuries across the lifespan. This is important because aging may lead to additional limitations due to loss of muscle units, leading to new onset of weakness, fatigue and changes in function. This case study illustrates the application of ABR principles in the treatment of an adult with neonatal brachial plexus injury. The participant is a 43-year old woman with history of left upper extremity (LUE) weakness from birth due to NBPI. She was born with a flaccid (L) arm; spontaneous finger movement started a couple of weeks after birth. She reports weak elbow movement during childhood. She underwent release of the pectoralis and subscapularis at age 6, but received minimal therapy following. She initially presented to clinic for evaluation of (R) UE pain, in the shoulder, elbow, and hand, and fasciculations in the scapular region and low back. She denied any functional limitations due to (L) UE weakness, but reported that she avoids activities because of her (R) UE pain. She is a pediatrician and lives with her husband and two teenage children. She is active outside the home and enjoys yoga. Initial examination revealed active ROM limits in the (L) UE at shoulder flexion, abduction, external rotation and elbow extension. Strength was grossly 4-5/5. The symptoms she was experiencing in her (R) UE were felt to be related to overuse and aberrant kinematics of the (L) side. The treatment plan focused on using ABR principles across two 12 week bouts of care to improve the kinematics and ROM of the (L) UE to reduce the load and impingement of the (R) UE. Botox was administered to the (L) pectoralis major and subscapularis during the 2nd bout of ABR. KEY COMPONENTS OF ACTIVITY-BASED REHABILITATION • Functional Electrical Stimulation: Use of NMES to facilitate desired actions • Self-feeding using triggered NMES to biceps • Stimulation to rhomboids to improve scapular stability during prone • Weight Bearing: Systematic loading along long bones and across joints • Prone on elbows with or without proximal support • Facilitation of crawling on open hand • Massed Practice: High volume repetition of task components • Facilitated grasp and release patterns during Connect Four • Repeated elbow flexion without trumpeting during self-feeding • Task-Specific Practice: Context specific training for skill acquisition. • UE dressing • Locomotor Training: Use of particular neural cues to drive reflexive motor response • Reciprocal patterned activities with bilateral UE SYMMETRY OF MOVEMENT IMPROVED ACTIVE RANGE OF MOTION IMPROVED 120 Botox 100 80 60 40 Sh. Flexion Sh. Abduction Sh. External Rotation 20 0 eval 1 eval 2 eval 3 eval 4 IMPLICATIONS FOR PRACTICE • Short high intensity bouts of OT using ABR yields improved outcomes for those with NBPI across the lifespan including: • increased ROM throughout the affected extremity • increased strength, muscle bulk/muscle mass • increased functional use of the affected extremity • increased awareness, bilateral integration, and development of the affected side • decreased use of compensatory movements • decreased pain and decreased contractures. • Modalities are appropriate and practical interventions for treating deficits related to NBPI across the lifespan.