Revised Brachial Plexus Poster
advertisement

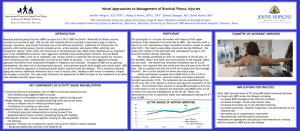
Physical Therapy Interventions to Improve Function in Children with Brachial Plexus Palsy Nick Pucillo SPT & Erik Rice SPT Background • Obstetric brachial plexus palsy is a complication of childbirth characterized by one or more nerve conduction blocks within the brachial plexus.1 • Brachial Plexus injuries occur in .15 – 3 out of every 1000 live births.2 • Common risk factors of Brachial Plexus injuries include: Previous deliveries with Brachial plexus injuries Prolonged labor Breech Delivery Assisted Delivery (vacuum or forceps) Gestational Diabetes2 • • • • • Clinical Evidence Electrical stimulation • 16 subjects were randomly assigned into electrical stimulation and conventional physical therapy group. • Both groups were seen three times weekly for 6 weeks. E-stim was provided to shoulder abductors, elbow flexors, and wrist extensors for 15 minutes on each muscle group. • The e-stim group demonstrated increased ROM compared to traditional therapy in shoulder abduction, elbow flexion, and wrist extension.3 Movement Therapy • This article looked at Modified constrained movement therapy compared to traditional treatment. • MCIMT program involved restraint of the noninvolved upper extremity to encourage movements in the affected arm. • There were significant improvements in both traditional and MCIMT groups; however, a the MCIMT group showed greater improvements in the Mallet Score Outcome Measure which assesses arm motion.1 Scapular Mobilization • Thirty children were randomly assigned to either a Scapular mobilization with traditional therapy or traditional therapy only groups. • The treatment period was 12 weeks. • There were significant improvements in shoulder flexion ROM in both groups from baseline, but the scapular mobilization group showed significantly greater improvements compared to the traditional therapy group.4 • • • A brachial plexus palsy will have different presentations depending on the involved areas. Erb’s Palsy includes an injury to the upper Brachial Plexus (C5, C6, sometimes C7) where the child will present with the elbow fully extended, internally rotated, and adducted. • These children still have good wrist flexion, but they lack extension The entire plexus (C5-T1) may be involved in which the child will present with a flail arm. Klumpke’s Palsy is more rare, but involves the lower Brachial Plexus C8T1.2 • Many studies are showing that traditional Physical Therapy interventions help improve limb function and ROM in children with Obstetric Brachial Plexus Palsy.1,3,4 • The literature describes that complementary therapy interventions such as Electrical Stimulation, Modified Constrained Movement Therapy, and Scapular Mobilization can further improve outcomes in upper limb function and ROM.1,3,4 • A thorough clinical assessment of the child’s impairments may help determine the appropriate treatment intervention. Further Research Presentation • Conclusions • • A key limitation to the previous studies is that the etiology was not specified as a neurotomesis (rupture of axon and sheath), axonotmesis (axon rupture), or neurapraxia (crush injury). Further high quality studies need to be conducted to further evaluate the efficacy of these interventions on Obstetric Brachial Plexus Palsy. References 1. Ehab M. Abdel-Kafy, Hebatallah M. Kamal, Samah A. Elshemy. Effect of modified constrained induced movement therapy on improving arm function in children with obstetric brachial plexus injury. Egyptian Journal of Medical Human Genetics. 2013; 14 (3), 299-305. Presentation of Erb’s Palsy Assisted Delivery Devices that may contribute to Brachial Plexus Palsy 2. Sebastin SJ, Chung KC. Pathogenesis and management of deformities of the elbow, wrist, and hand in late neonatal brachial plexus palsy. J Pediatr Rehabil Med. 2011;4(2):119-30. 3. Okafor UA, Akinbo SR, Sokunbi OG, Okanlawon AO, Noronha CC. Comparison of electrical stimulation and conventional physiotherapy in functional rehabilitation in Erb's palsy. Nig Q J Hosp Med. 2008;18(4):202-5. 4. Azzam AM. Effect of Scapular Mobilization on Improvement of Shoulder Flexion Range in Erb’s Palsy Children. J Nov Physiother. 2013; 3:153 www.postersession.com