Care Plan - HealthInsight
advertisement

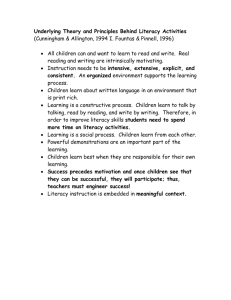
IC3 Beacon Pilot Diabetes Care Coordination Training Care Sarah Woolsey, M.D. Janet Tennison, PhD HealthInsight, August 16, 2012 This material was prepared by HealthInsight as part of our work as the Beacon Community, under Cooperative Agreement grant #90BC00006 from the Office of the National Coordinator, Department of Health and Human Services. Welcome Pre-work Today’s Objectives • Understand Care Coordination and SelfManagement • How to identify high risk patients with diabetes in your system • Assessing patients’ needs and goals – – – – – – Health Literacy Motivational Interviewing Stages of Change Teach Back Planned follow-up ProQual tool • Starting Care Coordination in your setting Definition: Care Coordination “The calculated integration of patient care activities between two or more participants, to facilitate the suitable provision of health care services” Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies (Vol. 7: Care Coordination).Technical Reviews, No. 9.7. McDonald KM, Sundaram V, Bravata DM, et al.Rockville (MD): Agency for Healthcare Research and Quality (US); 2007 Jun. Coordination--Why Do We Need It? • Determine the patients’ goals • Assist those “high-risk” patients who have been unsuccessful at managing their own care • Engage patients to improve their selfcare • Improve the exchange between providers, patients, community services We Sometimes Get Frustrated Removing Barriers to Accomplish Goals Engaging Patients in Their Own Care Traditional • Professionals are experts, patients passive • Behavior change externally motivated • Non-compliance is personal deficit Collaborative • Providers experts about disease; patients experts about lives • Behavior change internally motivated • Lack of goal achievement requires modifications Bodenheimer, T., & Abramowitz, S. (2010). Helping patients help themselves: How to implement self-management support. Oakland, CA: California HealthCare Foundation. Differences Traditional Patient Education • Technical skills • Problems with disease control • Disease-specific knowledge • Goal is compliance to improve outcomes • Health professional is educator Self-Management Education • Skills to act on problems • Problems ID‘d by patients • Improving confidence • Goal is increased selfefficacy to improve • Health team, peers, educators Bodenheimer, T., & Abramowitz, S. (2010). Helping patients help themselves: How to implement self-management support. Oakland, CA: California HealthCare Foundation. Organizational Outcomes Patient Outcomes •Culture/climate •Staff satisfaction •Efficiency/cost •Physiologic •Satisfaction •Functional status Clinical Information Systems1 Healthcare Organization6 Activated Patients Decision Support2 o Delivery System Redesign3 DSM Clinic Care Coordination Community 5 Resources SelfManagement4 Developed by Janet Tennison, PHD, Adapted from Kirsch et. al., 2008 Interprofessional Outcomes •Team Self-efficacy •Shared Perspectives •Teamwork • Attitudes towards collaboration Essential CC Tasks • • • • Identify high-risk patients Assess patient Develop care plan Identify care participants, communicate needs • Execute care plan • Monitor and adjust care • Evaluate health outcomes ESSENTIAL CARE TASKS and Associated Coordination Activity • IDENTIFY and ASSESS PATIENT Determine Likely Coordination Challenges, determine patients vulnerable to disconnected care • DEVELOP CARE PLAN Proactive Plan for Coordination Challenges and Follow-up IDENTIFY PARTICIPANTS IN CARE AND SPECIFY ROLES Specify Who is Primarily Responsible for Coordination (Medical Home) EXECUTE CARE PLAN Implement Coordination Interventions COMMUNICATE TO PATIENTS /Family AND ALL OTHER CARE PARTICIPANTS Ensure Information Exchange Across Care Interfaces MONITOR AND ADJUST CARE Monitor For and Address Coordination Failures EVALUATE HEALTH OUTCOMES Identify Coordination Problems that Impact Outcomes • • • • • Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies (Vol. 7: Care Coordination).Technical Reviews, No. 9.7. McDonald KM, Sundaram V, Bravata DM, et al.Rockville (MD): Agency for Healthcare Research and Quality (US); 2007 Jun. Case: Mr. Thomas • Mr. Thomas is a 56 -year old patient with DM II. • He has private insurance through his wife’s job. • He is here for a cough and cold visit, has not been in for 9 months. • You note he has no-shows recorded for his last 3 visits to you, both education visits and a diabetes check-up. Medical Assistant Check-In • • • • • He is taking 3/5 meds listed in the EMR by report. Metformin, Lisinopril and aspirin (unsure what kind). He is not on insulin, simvastatin as recorded here. He reports no pain or allergies. He has not had any office visits elsewhere. • Temp=98.0 • BP 152/90, pulse 88 • Weight is 224lb , BMI 29 • O2 sat is 99% • Hba1c = 10 (last time was 8.9) • Coughing • In his PJ top • Appears well otherwise What Are You Thinking Here? MA point of view Beacon point of view Doctor point of view Care Coordination point of view More Information Exam : • • • Obese Nasal congestion R toenail is ingrown (you checked) Labs today: Glucose-333 Old Labs: • • • LDL=144 Microalbumin is abnormal A1c=8.9 Other • He did not have a flu shot in 2011 • He has never had a depression screen • Non-smoker Is Mr. Thomas High Risk? • Vulnerable to disconnected care? • How do you find him in your system? • Name 3 ways Practice Analytics Tool “Hot Spot” Pilot • Diabetes Care Severity Index • Composite score of labs, diagnoses, and know risk of hospitalization • Option in the CC program What else do you want to know about Mr. Thomas? Patient Point of View? Consider… WHAT IS his GOAL for his care? Today? Overall? How do you know? ESSENTIAL CARE TASKS and Associated Coordination Activity • IDENTIFY/ASSESS PATIENT Determine Likely Coordination Challenges, determine patients vulnerable to disconnected care • DEVELOP CARE PLAN Proactive Plan for Coordination Challenges and Follow-up IDENTIFY PARTICIPANTS IN CARE AND SPECIFY ROLES Specify Who is Primarily Responsible for Coordination (Medical Home) EXECUTE CARE PLAN Implement Coordination Interventions COMMUNICATE TO PATIENTS /Family AND ALL OTHER CARE PARTICIPANTS Ensure Information Exchange Across Care Interfaces MONITOR AND ADJUST CARE Monitor For and Address Coordination Failures EVALUATE HEALTH OUTCOMES Identify Coordination Problems that Impact Outcomes • • • • • Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies (Vol. 7: Care Coordination).Technical Reviews, No. 9.7. McDonald KM, Sundaram V, Bravata DM, et al.Rockville (MD): Agency for Healthcare Research and Quality (US); 2007 Jun. Patient Assessment “Why is Mr. Thomas so non-compliant?” Three methods: The patient is not yet engaged! 1. Health Literacy 2. Stages of Change 3. Motivational Interviewing (MI) Patient and provider both have responsibility to determine and address barriers. Health Literacy • tervisealase kirjaoskuse • अनुवाद करने के लिए यहााँ पाठ दर्ज करें • • • • בריאות אוריינות alfabetizasyon sante Gesundheitskompetenz y tế biết đọc biết viết Definition Health Literacy Functional Health Literacy The capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions. The ability to read and comprehend prescription bottles, appointment slips, other essential healthrelated materials required to successfully function as a patient. Healthy People. (2010). Cited in What is Health Literacy? Retrieved from www.chcs.org Health Literacy • Only 12% of adults have proficient health literacy • 9/10 patients lack skills to manage their health/prevent disease • Ask Me 3 Advocate for Health Literacy in your organization (n. d.). Quick Guide to Health Literacy. Retrieved from http://HHS.com Determine then Support Health Literacy • Verify understanding by “teach back” • “Tell me in your own words what we just talked about” • “Why do you take this medication?” • Provide instructions like you’re speaking with a friend MOST IMPORTANT! Create a shame-free environment where low-literacy patients can seek help without embarrassment or being stigmatized Don’t Forget Culture • Ethnic/racial/population/religious differences affect perceptions, trust, access to medical care • Poverty, language and communication barriers, other demographics • Personal bias, prejudices, lack of understanding Mr. Thomas and Health Literacy • Visit Summary Example The Stages of Change Inappropriate Assumptions About Behavior Change • • • • • • • • This person ought to change, and wants to change. This patient’s health is the prime motivating factor for him/her. If he or she does not decide to change, the consultation has failed. Patients are either motivated to change, or not. Now is the right time to consider change. A tough approach is always best. I’m the expert. He or she must follow my advice. A negotiation-based approach is best. Emmons, K. M. , & Rollnick, S. (2001). Motivational Interviewing in health care settings: Opportunities and limitations. American Journal of Preventive Medicine, 20(1) How To Suppress Change • Tell patients what to do (give advice) • Misjudge sense of importance regarding behavior change • Use scare tactics, argue, blame them for no willpower and self-concern • Overestimate readiness to change and degree of confidence • Take control away and generate resistance Is Patient Ready to Change? Readiness to change: Stages of Change. (2005). Retrieved July 10, 2011, from Well-Fit Bodies Website: http://www.well-fitbodies.com/readiness_for_change Patient Assessments How ready are you (to improve a behavior)? 0 1 2 3 4 5 6 7 8 9 Not ready 10 Ready How confident are you (that you can)? 0 1 2 Not at all confident 3 4 5 6 7 8 9 10 Very Confident True Change Takes Time • Some may remain in one phase a long time or forever • Pre-contemplation—cons of quitting outweigh the pros • Relapse is expected, should be integrated to normalize it • Most don’t go from pre-contemplation to action • Goal—try to move through stages Success = Positive Relationships & Support Provider-patient relationship most important determinant of diabetes self-management Craig, C., Eby, D., & Whittington, J. (2011). Care Coordination Model: Better care at lower cost for people with multiple health and social needs. IHI Innovation Series white paper. Cambridge, Massachusetts: Institute for Healthcare Improvement. Where is Mr. Thomas? • • • • • Contemplation Pre-contemplation Preparation Action Maintenance BREAK Motivational Interviewing Motivational Interviewing “A collaborative, patientcentered form of guiding to elicit and strengthen motivation for change” Miller, W.R. & Rollnick, S. (2009). Ten things that Motivational Interviewing is not. Behavioural and Cognitive Psychotherapy, 37, 129-40. Motivational Interviewing • • • • • • Non-coercive Non-judgmental Non-confrontational Non-adversarial Explore and resolve inconsistency Help patients envision a better future, and become increasingly motivated to achieve it Why Do We Need MI? No matter what reasons we might offer to convince individuals of the need to change their behavior, or how much we want them to do so, lasting change is more likely to occur when they discover their own reasons and determination to change. Four Principles of MI 1. Express empathy 2. Explore differences 3. Roll with resistance 4. Support of self-efficacy OARS •Open-ended questions •Affirmations •Reflections •Summaries Patient Assessment Mr. Thomas Role play referral for insulin use, why was it unsuccessful before? What would you say and do? What is his goal? LUNCH 12:00-12:30 Pro Qual Tool–Patient Experience of Health Assessment and Barriers • http://informatics.mayo.edu/proqol (test) IC3 Beacon Pilot Diabetes Care Coordination Training Part 2 Care Sarah Woolsey, M.D. Janet Tennison, PhD Michelle Carlson, S.S.W. HealthInsight, 2012 This material was prepared by HealthInsight as part of our work as the Beacon Community, under Cooperative Agreement grant #90BC00006 from the Office of the National Coordinator, Department of Health and Human Services. Motivational Interview #2 • Mrs. Smith is a 48 y/o, she has had DM 2 for 5 years, since her last child was born. • She is on your list as a patient that has not come in for >12 months. • Her last A1c was 7.5, and she was up to date on DM care. • Today’s A1c=9. • You notice she has had no shows a few times for follow-up for Diabetes. WHAT MIGHT BE HAPPENING? Part 2 Learning Objectives • Developing a Care Plan • Identify roles • Communicating (information exchange) • Monitor and Adjust • Data collection • Resources ESSENTIAL CARE TASKS and Associated Coordination Activity • IDENTIFY/ASSESS PATIENT Determine Likely Coordination Challenges, determine patients vulnerable to disconnected care • DEVELOP CARE PLAN Proactive Plan for Coordination Challenges and Follow-up • IDENTIFY PARTICIPANTS IN CARE AND SPECIFY ROLES Specify Who is Primarily Responsible for Coordination (Medical Home) EXECUTE CARE PLAN Implement Coordination Interventions COMMUNICATE TO PATIENTS /Family AND ALL OTHER CARE PARTICIPANTS Ensure Information Exchange Across Care Interfaces MONITOR AND ADJUST CARE Monitor For and Address Coordination Failures EVALUATE HEALTH OUTCOMES Identify Coordination Problems that Impact Outcomes • • • • Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies (Vol. 7: Care Coordination).Technical Reviews, No. 9.7. McDonald KM, Sundaram V, Bravata DM, et al.Rockville (MD): Agency for Healthcare Research and Quality (US); 2007 Jun. The Mr. Thomas Care Plan Provider wants to re-start Insulin that patient agreed to start prior What is the current workflow at your site? How do we succeed? Care Plan Basic Clinic Example of a Working Care Plan For next visit: (To be completed by Physician /Care Coordinator and Patient) Patient Name__________________ Chart ID____________ Patient Goal: Medical Plan: • Care Coordination Needs/Referrals: __________________________________________ • Labs Needed: ___________________________________________________________ • New Meds/ Education Needed: ______________________________________________ • Ref letters/Contact needs for patient: ________________________________________ • Follow Up Needed: Call (Who/date/subject) ______________________________________________ Next Visit (Schedule period/date) _______________________________________ Next Visit agenda ___________________________________________________ Care Plan: Patient will: ____________________________________________________ By:(Date)_____________ Care Coordinator/Clinical Team will: ____________________________________________________ By:(Date)_____________ Reviewed Date __________ Care Team or Physician Signature Patient signature- plan Adapted from the Utah Medical Home Portal www.medicalhomeportal.org, 2009 Care Plan Brainstorm ESSENTIAL CARE TASKS and Associated Coordination Activity • • IDENTIFY/ASSESS PATIENT Determine Likely Coordination Challenges, determine patients vulnerable to disconnected care DEVELOP CARE PLAN Proactive Plan for Coordination Challenges and Follow-up • IDENTIFY PARTICIPANTS IN CARE AND SPECIFY ROLES Specify Who is Primarily Responsible for Coordination (Medical Home) • • EXECUTE CARE PLAN Implement Coordination Interventions COMMUNICATE TO PATIENTS /Family AND ALL OTHER CARE PARTICIPANTS Ensure Information Exchange Across Care Interfaces MONITOR AND ADJUST CARE Monitor For and Address Coordination Failures EVALUATE HEALTH OUTCOMES Identify Coordination Problems that Impact Outcomes • • Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies (Vol. 7: Care Coordination).Technical Reviews, No. 9.7.McDonald KM, Sundaram V, Bravata DM, et al.Rockville (MD): Agency for Healthcare Research and Quality (US); 2007 Jun. Roles at Your Clinic Who is going to coordinate the patients? When will the work get done? Initiation? Follow-up? Who is responsible for X patient? St Mark’s Pilot Success ESSENTIAL CARE TASKS and Associated Coordination Activity • • • • IDENTIFY/ASSESS PATIENT Determine Likely Coordination Challenges, determine patients vulnerable to disconnected care DEVELOP CARE PLAN Proactive Plan for Coordination Challenges and Follow-up IDENTIFY PARTICIPANTS IN CARE AND SPECIFY ROLES Specify Who is Primarily Responsible for Coordination (Medical Home) EXECUTE CARE PLAN Implement Coordination Interventions • COMMUNICATE TO PATIENTS/FAMILY AND ALL OTHER CARE PARTICIPANTS Ensure Information Exchange Across Care Interfaces • MONITOR AND ADJUST CARE Monitor For and Address Coordination Failures EVALUATE HEALTH OUTCOMES Identify Coordination Problems that Impact Outcomes • Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies (Vol. 7: Care Coordination).Technical Reviews, No. 9.7.McDonald KM, Sundaram V, Bravata DM, et al.Rockville (MD): Agency for Healthcare Research and Quality (US); 2007 Jun. Communication • TEMPLATE DEVELOPMENT • How will you share this information with all team members? • Where Does the Care Plan Go in the Chart? • How is a patient flagged? Communication • When should I call you or have you come in (to check on progress)? • Reinforce Change Plan at every visit/opportunity • Share plan with all team members • Assist with problem solving as needed ESSENTIAL CARE TASKS and Associated Coordination Activity • • • • • IDENTIFY/ASSESS PATIENT Determine Likely Coordination Challenges, determine patients vulnerable to disconnected care DEVELOP CARE PLAN Proactive Plan for Coordination Challenges and Follow-up IDENTIFY PARTICIPANTS IN CARE AND SPECIFY ROLES Specify Who is Primarily Responsible for Coordination (Medical Home) EXECUTE CARE PLAN Implement Coordination Interventions COMMUNICATE TO PATIENTS/FAMILY AND ALL OTHER CARE PARTICIPANTS Ensure Information Exchange Across Care Interfaces • MONITOR AND ADJUST CARE Monitor For and Address Coordination Failures • EVALUATE HEALTH OUTCOMES Identify Coordination Problems that Impact Outcomes Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies (Vol. 7: Care Coordination).Technical Reviews, No. 9.7.McDonald KM, Sundaram V, Bravata DM, et al.Rockville (MD): Agency for Healthcare Research and Quality (US); 2007 Jun. Monitor and Adjust • Set strong boundaries with patients: role/purpose, time constraints • Discuss “problem patients” with care team: decide if appropriate for care coordination • Discuss other potential failure reasons with team • Reassess patients, as needed ESSENTIAL CARE TASKS and Associated Coordination Activity • • • • • • • IDENTIFY/ASSESS PATIENT Determine Likely Coordination Challenges, determine patients vulnerable to disconnected care DEVELOP CARE PLAN Proactive Plan for Coordination Challenges and Follow-up IDENTIFY PARTICIPANTS IN CARE AND SPECIFY ROLES Specify Who is Primarily Responsible for Coordination (Medical Home) EXECUTE CARE PLAN Implement Coordination Interventions COMMUNICATE TO PATIENTS /Family AND ALL OTHER CARE PARTICIPANTS Ensure Information Exchange Across Care Interfaces MONITOR AND ADJUST CARE Monitor For and Address Coordination Failures EVALUATE HEALTH OUTCOMES Identify Coordination Problems that Impact Outcomes Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies (Vol. 7: Care Coordination).Technical Reviews, No. 9.7. McDonald KM, Sundaram V, Bravata DM, et al.Rockville (MD): Agency for Healthcare Research and Quality (US); 2007 Jun. Health Outcomes Data Collection • Excel Database • Document your success • Assist us in program evaluation • Learn to measure what you do • Develop your capacity to show the quality you deliver Knowing Your Community Resources and Referrals Beacon Website Resources Beacon Clinic Resources Public Benefit Programs • SSI (Social Security Income) • SSDI (Social Security Disability Income) • Medicare (Over 65 years-old, and disabled) • Medicaid and CHIP (Low income) Support Groups • Disease-based (Cancer, Mental Health) • On-line groups (Women’s, Grief, Addictions) • Agency-based (Red Cross, United Way) • 2-1-1 Community Resources • Religion affiliated (LDS, Catholic Community) • Aging and elder care • Pharmacy Assistance Programs • Homeless services • Donated dental Home Health • Home health referrals and criteria (Skilled need, homebound status) • Pre-authorizing services through insurers • DME (FWW’s, potty-chairs, electric WC’s) Long-Term Care • Skilled Nursing Facility (SNF) - Skilled needs vs. “custodial” • Extended Care Facility (ECF) • Independent/Assisted Living • Medicare versus private pay • Referral processes/paperwork How to Succeed • • • • • • • ID the right patients reliably Track patients Care Plan in place for patients with a patient goal in place Follow-up in place for care plan items Resources list available, if needed Improving DM measures in patients and meeting their goals for care Patient Satisfaction, experience of health and support Wrap-Up and Next Steps • HealthInsight Assistance • Feedback on self-assessments • Data collection tool assistance • Monthly visit with team (if desired) • Proqual assistance Wrap-Up and Next Steps • Action Plan • What can you do by next Tuesday? (ideas) -- Finish assessments -- Team meeting -- Begin using ProQual tool on patients Wrap-Up and Next Steps • Evaluations