File
advertisement

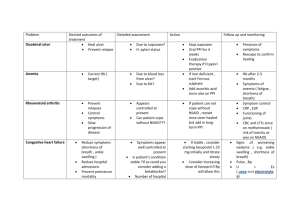
PEPTIC ULCER DISEASE Aman Sulehri Gastric Physiology Gastroduodenal Mucosal Defense:The mucosal defense system can be divided as a threelevel barrier 1. Preepithelial 2. Epithelial 3. Subepithelial Definition:“An ulcer is defined as disruption of the mucosal integrity of the stomach and/or duodenum leading to a local defect or excavation due to active inflammation.” Types of Peptic Ulcer I. Depending on the site: A. Duodenal Ulcer: Typically occurs in the first inch of 1st part of the duodenum B. Gastric Ulcer: Occurs in the lesser curvature adjacent to acid secreting parietal cell mass. C. Combined: Gastric ulcer type II Zollinger Ellison syndrome D. Anastomotic ulcer II. Depending on the duration: A. Chronic peptic ulcer B. Acute peptic ulcer Epidemiology • In US, approx 4 million people have PU and 350,000 new cases are diagnosed each year. • Around 180,000 patients are hospitalized yearly. And about 5000 people die each year as result of PUD. • The lifetime likelihood of developing PU is abt 10% for amercian males and 4% for females. • The male-to-female ratio for DU is ant 3:1, and for gastric ulcer abt 1.5 to 2:1. • DU more common between ages 30-50 years old and GU more common in people over age 60 years old Etiology • • • • Helicobacter pylori infection(90%) Drugs - anti-inflammatory(NSAIDs) & Corticosteroids Hyperacidity - e.g.. Zollinger Ellison syndrome. Food habits(Spicy food, diet poor in vitamins, smoking and alcohol) • Diabetes may increase your risk of having H. pylori • Lifestyle factors, including chronic stress, coffee drinking, may make more susceptible to damage from NSAIDs or H. pylori if one is a carrier of this organism. But these factors do not cause an ulcer on their own. • Diseases associated with an increased risk of PUD include cirrhosis, chronic obstructive pulmonary disease, renal failure, and organ transplantation. Pathogenesis H. pylori and Acid Peptic Disorders: • The bacterium is a gram-negative microaerophilic rod found most commonly in the deeper portions of the mucous gel coating the gastric mucosa or between the mucous layer and the gastric epithelium. It may attach to gastric epithelium but under normal circumstances does not appear to invade cells. • It induces an intense inflammatory & immune response. There is increased production of pro-inflammatory cytokines such as IL-1, IL6 TNF, IL-8. This cytokine is produced by mucosal epithelial cells, and it recruits and activates neutrophils • Several bacterial genes products are involved in causing epithelial cell injury and induction of inflammation. • H.pylori secrets urease that breaks down urea to form toxic compounds such as ammonium chloride and monochloramine • The organism also elaborate phospholipases that damage surface epithelial cells. • Bacterial proteases and phospholipases break down the glycoprotein-lipid complexes in gastric mucus, thus weakening 1st line mucosal defense • It also enhances gastric acid secretion and impairs duodenal bicarbonate production thus reducing pH in duodenum • Several H.pylori are immunogenic, and they cause activation of both T cells and B cells • Thromboembolic occlusion of surface capillaries is promoted by bacterial platelet-activating factor. • A specific region of the bacterial genome, the pathogenicity island, encodes the virulence factors cytotoxin-associated antigen(Cag A) associated with more severe epithelial damage, greater acute and chronic inflammation, higher likelihood of PU and gastric cancer • One important genes regulated by CagA is vacuolating toxin(VacA) which causes cell injury in vitro and gastric tissue demage.it also act as urea transporter and hence increasing permeability of epithelium to urea NSAIDs associated PU: Chronic use of NSAIDs suppresses mucosal prostaglandin synthesis by blocking COX-1 and COX-2 Zollinger-Ellison syndrome associated PU: Excess gastrin secretion by tumor and hence excess gastric acid production • Cigarette smoking impairs mucosal blood flow and healing. • Corticosteroids in high dose and with repeated use promote ulcer formation • Too-rapid gastric emptying, exposing duodenal mucosa to an excessive acid load Clinical Features • Epigastric pain (the most common symptom) it is said that gastric ulcers present with pain associated or closely followed by eating ,where-as duodenal ulcer pain is relieved by food. Burning in nature Patient awakens with pain at night. May radiate to the back (consider penetration) • Increased salivation(water brash) • Nausea • Vomiting, which might be related to partial or complete gastric outlet obstruction • Dyspepsia, including belching, bloating, distention, and fatty food intolerance • Chest discomfort • Anorexia, weight loss • Hematemesis(this can occur due to bleeding directly from a gastric ulcer, or from damage to the esophagus from severe vomiting) • Melena Complications • Gastrointestinal bleeding • Perforation • Penetration is when the ulcer continues into adjacent organs such as the liver and pancreas. • Scarring and swelling due to ulcers causes narrowing in the duodenum and gastric outlet obstruction Diagnosis • Oesophagogastroduodenoscopy(OGD): Ulcer appears as a crater with/without slough or bleeding . In GU, routine biopsy is advised to r/o malignancy while in DU biopsy is done in recurrent cases to r/o H.pylori • Barium meal study: DU: Deformed duodenal cap. Trifoliate deformity is seen when secondary duodenal diverticulum occurs GU: appears as niche in lesser curvature due to ulcer crater and as notch on greater curvature due to spasm of stomach Duodenal Ulcer Gastric Ulcer DU GU Tests for Detection of H. pylori Invasive (Endoscopy/Biopsy Required); • Rapid urease test: Simple; sensitivity and specificity of 90 to 99% Three kits (ie, CLOtest, Hp-fast, Pyloritek) are commercially available, each containing a combination of a urea substrate and a pH sensitive indicator. One or more gastric biopsy specimens are placed in the rapid urease test kit. If H pylori is present, bacterial urease converts urea to ammonia, which changes pH and produces a color change. • Histologic test: To directly ascertain presence of H. pylori • Culture: Allows determination of antibiotic susceptibility Non-invasive: • Antibodies: IgG to H pylori can be measured in serum, plasma, or whole blood. • Urea breath test: Simple; sensitivity and specificity of 90 to 99% • Stool antigen: >90 sensitivity, convenient; not established for eradication but promising D/D • • • • • • • Gastritis Stomach cancer Gastro esophageal reflux disease Pancreatitis Cholecystitis Inferior myocardial infarction Referred pain (pleurisy, pericarditis) Medical Treatment Surgical Treatment Indication: • Intractable pain in spite of treatment with H2 receptor blockers, omeprazole and not responding to anti H.pylori regime • Frequent relapses, H.pylori –ve • Complications of DU: Gastric outlet obs. Hemorrhage Highly Selective Vagotomy(HSV) • Also called parietal cell vagotomy or proximal gastric vagotomy and it causes minimal side effects • In this operation, vagi are not divided at the trunk. Both ant. & post. Vagus are identified, isolated & preserved. Their branches (i.e. ant & post greater gastric nerves of latarjet) which run along the lesser curvature are isolated. • The branches supplying parietal cell mass are divided, hence it is called parietal cell vagotomy. • The terminal fibers of nerve of Latarjet which supply pylorus are preserved Vagotomy and Drainage • Ant & post trunks of vagus are divided just below diaphragm followed by drainage procedure like gastro-jejunostomy(GJ) • Vagus is secretomotor to stomach & after vagotomy the motility of stomach is lost ang gastric stasis occurs, hence drainage is done • Post GJ is preferred because it gives a dependent drainage by food contents due to gravity, • Alternative pyloroplasty is preferred by few surgeons instead of GJ in which pylorus is incised longitudinally & sutured vertically. Thus, the pyloric ring become incompetent and wide open Truncal vagotomy Anterocolic GJ Retrocolic GJ Billroth I partial gastrectomy • Partial gastrectomy is done including removal of ulcer followed by gastroduodenal anastomosis • It has least recurrence rate of less than 1% but mortality rate is around 1-2% Billroth II gastrectomy • It is indicated when gastric ulcer is located on lesser curvature. • Here gasterctomy is done below the ulcer and remnant of stomach is anastomosed to jejunal loop(gastrojejunal anastomosis) Thank GOD it finished