Using Cases to Teach Biology UW-Madison 2012
advertisement

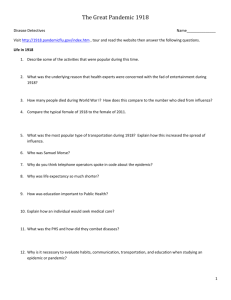
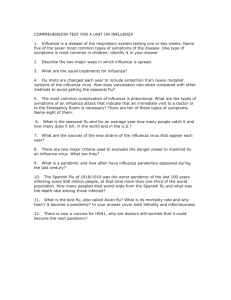
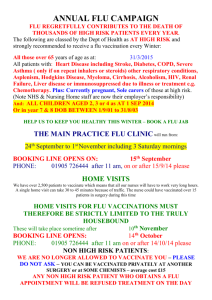
Using Cases to Teach Biology UW-Madison October 18, 2012 >Texas2009227831823 ATGAATCCAAACCAAAAGATAATAACCATTGGTTCGGTCTGTATGACAATTGGAATGGCTAACTTAATAT TACAAATTGGAAACATAATCTCAATATGGATTAGCCACTCAATTCAACTTGGGAATCAAAATCAGATTGA AACATGCAATCAAAGCGTCATTACTTATGAAAACAACACTTGGGTAAATCAGACATATGTTAACATCAGC AACACCAACTTTGCTGCTGGACAGTCAGTGGTTTCCGTGAAATTAGCGGGCAATTCCTCTCTCTGCCCTG TTAGTGGATGGGCTATATACAGTAAAGACAACAGTGTAAGAATCGGTTCCAAGGGGGATGTGTTTGTCAT AAGGGAACCATTCATATCATGCTCCCCCTTGGAATGCAGAACCTTCTTCTTGACTCAAGGGGCCTTGCTA AATGACAAACATTCCAATGGAACCATTAAAGACAGGAGCCCATATCGAACCCTAATGAGCTGTCCTATTG GTGAAGTTCCCTCTCCATACAACTCAAGATTTGAGTCAGTCGCTTGGTCAGCAAGTGCTTGTCATGATGG CATCAATTGGCTAACAATTGGAATTTCTGGCCCAGACAATGGGGCAGTGGCTGTGTTAAAGTACAACGGC ATAATAACAGACACTATCAAGAGTTGGAGAAACAATATATTGAGAACACAAGAGTCTGAATGTGCATGTG TAAATGGTTCTTGCTTTACTGTAATGACCGATGGACCAAGTAATGGACAGGCCTCATACAAGATCTTCAG AATAGAAAAGGGAAAGATAGTCAAATCAGTCGAAATGAATGCCCCTAATTATCACTATGAGGAATGCTCC TGTTATCCTGATTCTAGTGAAATCACATGTGTGTGCAGGGATAACTGGCATGGCTCGAATCGACCGTGGG TGTCTTTCAACCAGAATCTGGAATATCAGATAGGATACATATGCAGTGGGATTTTCGGAGACAATCCACG CCCTAATGATAAGACAGGCAGTTGTGGTCCAGTATCGTCTAATGGAGCAAATGGAGTAAAAGGATTTTCA TTCAAATACGGCAATGGTGTTTGGATAGGGAGAACTAAAAGCATTAGTTCAAGAAACGGTTTTGAGATGA TTTGGGATCCGAACGGATGGACTGGGACAGACAATAACTTCTCAATAAAGCAAGATATCGTAGGAATAAA TGAGTGGTCAGGATATAGCGGGAGTTTTGTTCAGCATCCAGAACTAACAGGGCTGGATTGTATAAGACCTAGCGG GAGCAGCATAT CCTTTTGTGGTGTAAACAGTGACACTGTGGGTTGGTCTTGGCCAGACGGTGCTGAGTTGCCATTTACCAT TGACAAGTAA Ethel Stanley, BioQUEST Science Case Network This workshop focuses on the use of cases and PBL (problem based learning) as pedagogical strategies to support collaborative, open-ended inquiry in biology. In addition, we will use the Science Case Network website to share both the resources and participant responses at: http://sciencecasenet.org/using-cases-to-teach-biology/ The international Commission on Biology Education (CBE) raised the bar for scientists and educators: “Influencing almost all our activities, from inception to the grave, this (biological) revolution will require profound decisions with respect to the ethical, legal, social, cultural, educational, and development issues that are sure to arise, affecting our personal lives and society in ways that we have never experienced before.” (Vohra 2000) Criticism of the way we teach science “Build into every course inquiry*, the processes of science, a knowledge of what practitioners do, and the excitement of cutting edge research.” “involving the student in asking questions and finding answers” Shaping the Future: New Expectations for Undergraduate Education in Science, Mathematics, Engineering and Technology NSF, 1996. (p. 53) Entry into an age of cyberlearners Our students engage early as self-directed learners: Less reliant on authority/experience Instant information retrieval Social construction/collaboration Preparing students to be scientifically literate citizens as well introducing what it means to be a scientist is a challenging role for faculty. Teaching biology is becoming increasingly interdisciplinary and global in terms of methodology, tools, and data. (NSF, 2008; NRC, 2009; AAAS, 2010; UNESCO, 2010; MOE, 2010) One strategy to address contemporary biology education is to use investigative cases. “Crossing the Chasm” of Curricular Reform: BioQUEST Curriculum Consortium Invites CAL-laboration CAL-laborate Volume 4 June 2000 http://historymatters.gmu.edu/d/107 “There Wasn’t a Mine Runnin’ a Lump O’ Coal”: A Kentucky Coal Miner Remembers the Influenza Pandemic of 1918–1919 . . you ain't old enough to remember the year the flu struck the people so bad in this . . . in this country, do you? HAWKINS: Yeah, I think that both my… both my great-grandparents died in that. T. BARTLEY: It was the saddest lookin‘ time then that ever you saw in your life. My brother lived over there in the camps then and I was working over there and I was dropping cars onto the tipple. And that, that epidemic broke out and people went to dyin’ and there just four and five dyin‘ every night dyin’ right there in the camps, every night. And I began goin‘ over there, my brother and all his family took down with it, what’d they call it, the flu? Yeah, 1918 flu. And, uh, when I’d get over there I’d ride my horse and, and go over there in the evening and I’d stay with my brother about three hours and do what I could to help ’em. And every one of them was in the bed and sometimes Doctor Preston would come while I was there, he was the doctor. And he said “I’m a tryin‘ to save their lives but I’m afraid I’m not going to.”And they were so bad off. And, and every, nearly every porch, every porch that I’d look at had—would have a casket box a sittin’ on it. And men a diggin‘ graves just as hard as they could and the mines had to shut down there wasn’t a nary a man, there wasn’t a, there wasn’t a mine arunnin’ a lump of coal or runnin' no work. Stayed that away for about six weeks. . T. BARTLEY: Case Analysis 1. What is this narrative about? 1. What do you already know? What would you like to know more about? KNOW NEED TO KNOW Group work time: One person from each group should post case analysis results using web page: http://sciencecasenet.org/using-cases-to-teach-biology/ 1. What is this case about? Flu of 1918 and its effects on coal mining, community Know There was a pandemic of flu in 1918. It killed many people. It interrupted work, mines closed. Some people lived in camps. It lasted about 6 weeks, according to the transcript. The doctor felt he couldn’t help people get better. Dealing with the dead was a huge issue. In 1918, World War I was ending. There were no vaccines then. Viruses were unknown. Influenza is caused by a virus. There’s a flu shot that you get every year. Need to Know Did soldiers/sailors bring the flu from elsewhere? Was there flu in other countries besides the US? How long did it last? What treatments were available then? What treatments were available now? How is flu spread? Why did so many people die of it? What made this particular flu so deadly? Do people die of flu today, like the annual flu? Have there been other epidemics of flu? Could it happen again? Next? •Focus on the questions raised by groups •Introduce relevant lecture/lab content •Open inquiry experience •… Data http://www.demog.berkeley.edu/~andrew/1918/ Year 1911 Male 50.9 Female 54.4 1912 1913 1914 1915 51.5 50.3 52 52.5 55.9 55 56.8 56.8 1916 1917 1918 49.6 48.4 36.6 54.3 54 42.2 1919 53.5 56 Average Age at Death from 1911 until 1919 (Noymer 2007) Age <1 1917 2944.5 1918 4540.9 1--4 5--14 15-24 422.7 47.9 78 1436.2 352.7 1175.7 25-34 35-44 45-54 117.7 193.2 292.3 1998 1097.6 686.8 US Deaths per 100,000 Attributed to Influenza and Pneumonia in 1917 and 1918 (Noymer 2007) Strategies In 1918, Seattle public health officials required all passengers and employees mass transit systems wear masks. At that time no one knew what caused the influenza and vaccines were not available. It was understood that coughing and sneezing contributed to the spread of the disease. Spitting was also prohibited in many cities. Street car conductor in Seattle not allowing passengers aboard without a mask. Record held at: National Archives at College Park, MD. 165-WW-269B-11 Tools 200 180 160 # People 140 120 100 80 60 40 20 0 0 20 Susceptible # 40 Time Infected # 60 80 Recovered # Predict generally what changes you’d expect to see in the SIR model results with respect to S, I, and R individuals if you were to simulate the use of masks. (Hint: Assume a 10% decrease in transmission.) 100 Simulation Results for Scenario 2 of Avian Influenza with 200 people (200 susceptible) and the use of masks with a 10% reduction in transmission. Masks are used starting on day 30, when the epidemic has already nearly run its course. Simulation Results for Scenario 3 of Avian Influenza with 200 people (200 susceptible) and the use of masks with a 10% reduction in transmission. Masks are used starting on day 10, when the epidemic is still in its growth phase. The effect of public health measures on the 1918 influenza pandemic in U.S. cities. Bootsma MC, Ferguson NM. Mathematical Institute, Faculty of Sciences, Utrecht University, Budapestlaan 6, 3508 TA Utrecht, The Netherlands. During the 1918 influenza pandemic, the U.S., unlike Europe, put considerable effort into public health interventions. There was also more geographic variation in the autumn wave of the pandemic in the U.S. compared with Europe, with some cities seeing only a single large peak in mortality and others seeing double-peaked epidemics. Here we examine whether differences in the public health measures adopted by different cities can explain the variation in epidemic patterns and overall mortality observed. We show that city-specific per-capita excess mortality in 1918 was significantly correlated with 1917 per-capita mortality, indicating some intrinsic variation in overall mortality, perhaps related to sociodemographic factors. In the subset of 23 cities for which we had partial data on the timing of interventions, an even stronger correlation was found between excess mortality and how early in the epidemic interventions were introduced. We then fitted an epidemic model to weekly mortality in 16 cities with nearly complete intervention-timing data and estimated the impact of interventions. The model reproduced the observed epidemic patterns well. In line with theoretical arguments, we found the time-limited interventions used reduced total mortality only moderately (perhaps 10-30%), and that the impact was often very limited because of interventions being introduced too late and lifted too early. San Francisco, St. Louis, Milwaukee, and Kansas City had the most effective interventions, reducing transmission rates by up to 30-50%. Our analysis also suggests that individuals reactively reduced their contact rates in response to high levels of mortality during the pandemic. http://www.pnas.org/cgi/reprint/0611071104v1 Fig. 2. Effects of transient imperfect health interventions on epidemic dynamics. Results derived from a simple deterministic susceptible–infected– recovered (SIR) epidemic model. Weekly infection incidence over 6 months from a SIR model with 3.5-day infectious period, R0 = 2, 100,000 population, two seed infections at time 0, and controls imposed from day 25. Green curve, no controls; red curve, over-effective controls that reduce R by 40% and stop on day 75 (leading to a second wave); blue curve, controls that reduce R by 32.5% and stop on day 110 (giving the minimal possible epidemic size). Interventions Pharmacological Interventions • • Vaccination Antivirals as prophylactics Nonpharmacologic interventions (NPIs) – efficacy and gaining compliance • • • • • Community mitigation (school closures, restrictions on movements) Quarantine and isolation of healthy and sick individuals Travel restrictions locally and globally Social distancing Use of masks and increased hygiene • Poultry industry (CAFO placement and regulation) Concentrated Animal Feeding Operations • • Swine production (CAFO placement and regulation) Importers and exporters of other goods and services • Pharmaceutical industry Antiviral availability • • Health insurance industry Health care industry Hospital space limitations for isolation and treatment • Loss of personnel to pandemic Margaret Waterman (Southeast Missouri State) Suggested resources related to pandemic planning: Pandemicplanning.gov Avianflu.gov National Governor’s Association document on Preparing for Pandemic Influenza Centers for Disease Control and Prevention (cdc.gov) World Health Organization (www.who.int/en/) PubMed (www.ncbi.nlm.nih.gov/ Mapping the flu in the 21st century Many of the maps that track the current H5N1 avian flu in humans and birds are interactive http://www.pbs.org/newshour/indepth_coverage/health/birdflu/map_flash.html http://news.bbc.co.uk/1/shared/spl/hi/world/05/bird_flu_map/html/1.stm http://online.wsj.com/public/resources/documents/infoflash05a.html?project=avianflumap05&h=500&w=780&hasAd=1 First install Google Earth from http://earth.google.com . Next load the Bird Flu layer: http://www.daden.co.uk/newsglobe/birdflu.kmz Please see the website for resources.