Pediatric Medication Calculation

Pediatric IV Therapy
Amy E. Irwin, DNP, MS, RN
Denver School of Nursing
Purpose of IV Therapy
• Correct fluid and electrolyte imbalances
• Administer medications
• Administer blood products
• Administer nutrients
Principles of IV Access
• The largest visible vein is not necessarily the preferred one
• Consider the comfort of the patient
• Consider the position and extent restraint
• Consider the vessel’s ability to maintain a needle
• Consider the solution to be infused
Developmental Considerations
• INFANT
– Handle infant gently, speak softly
– Avoid arm used for thumb sucking
– Cuddle immediately after insertion
– Don’t feed immediately prior to insertion
– Avoid presence of extra personnel to minimize stranger anxiety
Developmental Considerations
• TODDLER/PRESCHOOLER:
– Prepare child immediately prior to procedure
– Give simple explanations in concrete terms
– Explain that you will help child hold still
– Emphasize that the IV is not punishment
Developmental Considerations
• SCHOOL-AGER
– Prepare child ahead of time, but on the day of insertion only
– Give the child choices as appropriate
– Give positive reinforcement after completion
Developmental Considerations
• ADOLESCENT
– Prepare teenager several hours to a day before procedure
– Approach discussions on a more adult level
– Discuss fears related to procedure
– Include teen in decisions
Pediatric Optimal Locations
• Hands
• Forearm
• Feet
• Scalp
**Note if the child is a thumb sucker,etc
Pediatric Catheter Gauges
• Use the largest catheter you can successfully insert
• Catheter Sizes:
Newborn: 24, 22 gauge
Infant < 1 year: 24, 22 gauge
1 – 8 years: 22, 20, 18 gauge
8 years and older: 20, 18, 16 gauge
EMLA Cream
• Minimizes or prevents pain from needle puncture for an IV, blood sample, or implanted port access.
• Apply EMLA cream to the selected site 60 minutes before the procedure.
• Cover at least two sites in case the first attempt is not successful.
Complications of PIVs
• Mechanical factors predispose IV infusion to shorter dwelling time
• Mechanical factors include:
Insertion site
Length of catheter
Size of vessel
Vessel fragility
Activity level of the patient
Forceful administration of boluses of fluid
Infusion of vessicants or irritants through small vessels
Complications of IV Therapy
• Infiltration (extravasation)
– Fluid leaks into subcutaneous tissue
Complications of IV Therapy
• Catheter Occlusion
– Blockage usually by clotted blood or precipitate
• Air Embolism
– Air enters circulation & travels to right side of heart
• Phlebitis
– Injury to vein without clot
– Inflammation of the blood vessel
Complications of IV Therapy
• Thrombophlebits
– Inflammation of a blood vessel with thrombus formation
• Infection
– Introduction of pathologic organisms locally or systemic
• Metabolic derangement
– Imbalance in electrolytes, minerals, glucose & proteins
Venous Access Devices
Intraosseous Infusion
• Used in emergency situations when a peripheral vein cannot be accessed
• Needle is inserted into the medullary cavity of a bone
• Used to administer fluid and medications
• Safe and reliable method for rapid administration
Intraosseous Infusion Site Tips
• Using aseptic technique, prep site with povidone-iodine solution
• Use 18 gauge in infants < 3 months of age
• Use firm, gentle pressure in a twisting motion to insert needle
• Insert perpendicular to site, or at a slight angle away from nearest joint
• Stop when you feel a “pop” and attempt to aspirate and/or flush
• Secure tubing to leg to prevent pulling on insertion site
• Flush meds with 5 – 10 cc NS
• Requires pressure for fluids to run
Characteristics of Pediatric
Administration Sets
• Calibrated volume & control chamber with a limited capacity & an automatic shutoff mechanism
– Ie. Buretrol, Metriset
• Standard of Practice
– All IV meds should be placed on a syringe pump if child is < 6 months
Buretrol Administration Set
Characteristics of Pediatric
Administration Sets
• Drip chamber with microdropper delivering 60 gtts/min or 60cc/hr
• Tubing compatible with pump, catheter adapter for needleless systems
• Standard of practice: All IV sites should be checked and reprogrammed every hour
• Armboards are utilized to maintain integrity of IV site (may also require restraints)
Principles of IV Fluid Therapy
• IV fluids are administered for the following reasons:
– To provide water, electrolytes, nutrients
– To replace water, correct electrolyte deficits
(replacement)
Composition of Fluids
• Isotonic: electrolyte content approximately 310 meq/L
– Examples: D5W, D10W, NS, LR
•
Hypotonic: electrolyte content less than
250meq/L (never used in children)
– Examples: No examples in pediatrics
•
Hypertonic: electrolyte content exceeds 375 meq/L
– Examples: 3% saline, D5.45NaCl, D5.9NaCl
Maintenance Fluid
Requirements
• Fluid calculations are based on weight in kilograms
Maintenance Fluid Intake
0 – 10 kg weight needs 4 cc/kg/hr
11 – 20 kg weight needs 2 cc/kg/hr additional
21 kg plus weights needs 1 cc/kg/hr additional
Example
23 kg Child
Calculate:
•
10 x 4=40
•
10 x 2=20
•
3 x 1=3
Total maintenance fluid requirements=63cc/hr
Example
22 kg Child who is “fluid-restricted” at 2/3 maintenance due to kidney failure
Calculate:
10 x 4 = 40
10 x 2 = 20
1 x 2 = 22
Total maintenance fluid = 62 cc/hr
At 2/3 maintenance = ?
Factors Influencing Pediatric Drug
Administration
• Children vs. Adults
• Physiological differences
• Immature kidney and liver function
Factors Influencing Pediatric Drug
Administration
• Slow gastric emptying time.
• Decreased gastric acid secretion in children under 3 years of age
• Lower concentration of plasma proteins
Additional Variations to consider with
Pediatric IV medications
• Patient weight in kilograms
• Patient fluid status/maintenance rate
• Patient diagnosis (fluid restriction?)
– Renal
– Cardiac
• Additional medications to administer
• Volume of IV tubing
– Need to flush med through after administration
IV Drug Administration
• 1. Calculate Safe dose (mg/kg)
• 2. Calculate amount to administer (cc)
• 3. Calculate final concentration or dilution for IV medications
• 4. Calculate rate of infusion
• 5. Set pump accordingly
• 6. Flush med! (same rate as administered)
Patient Example
• 12 kg child
– 825 mg Ancef q8h
• Follow each step!
– 1. Safe dose?
– 2. Amount to administer?
– 3. Final concentration?
– 4. Rate of infusion?
– 5. Does it make sense?
1. Calculate Safe Dosage
• Mg/kg x patient weight
• Example: 12 kg Child
Ordered: Ancef 825 mg IV q 8 h
Recommended 200-400mg/kg/Day
Dose on hand: 200mg/cc
Pt wt. = 12 kg
200 x 12 = 2400mg/Day
400 x 12 =4800mg/Day
Calculate Safe Dosage
• Divide by 3 (for Q 8 hours) for the safe dose:
– 2400 divided by 3 = 800mg/kg/dose
– 4800 divided by 3 = 1600mg/kg/dose
– Therefore the DOSE IS SAFE because it falls within the range
2. Calculate the Amount to
Administer
• Dose on hand (concentration from pharmacy) = 200mg/cc
• 200mg : 825mg =4.12cc to administer
1cc x
200x = 825 x=4.12cc
3. Calculate Final Concentration
(Dilution)
Recommended: 125 mg / 5cc infuse over 30”
125 mg : 825mg = 33.0cc dilution required
5cc x
4. Calculate Rate of Infusion
• Volume
– 4.12 cc med + 33.0cc dilution = 37.12 total
– Desired minutes: 30
37.12 x 60 = 74 cc/hr
30
Set pump at 74 cc/hr
5. Don’t Forget……
• After completing all of your calculations….
• DOES IT MAKE SENSE??
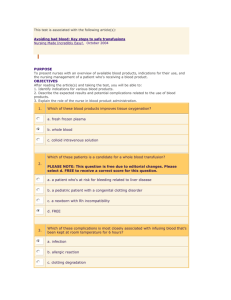
Blood Products
• It is the RNs responsibility to know
1. Why a specific product is being given
2. A safe volume over a safe time has been ordered
3. The common side effects of giving the product
• No solutions other than normal saline and 5% albumin should be in IV tubing used to administer blood products
Blood Products Continued
• Once a blood product has been issued from the blood bank, the transfusion must be completed within 4 hours
• Tubing is changed after blood products are given unless one unit is followed immediately by the next, in that case multiple units can be given with the same infusion set
Blood Products Continued
• Most infusion sets are limited to 4 units, and all infusion sets are limited to 4 hours (whichever occurs first).
• All blood components must be administered through an infusion set with an in-line filter designed to retain blood clots and particles potentially harmful to the recipient
• Platelets, fresh frozen plasma, and cryoprecipitate do not need to be cross-matched; however, a blood type is necessary to pick the appropriate products. If the patient has a blood bank history, no specimen is required.
Assessment, Administration, and
Tranfusion Reactions:
• Complete assessment prior to starting the transfusion including: Vital Signs (Temp, HR,
RR, BP), Skin (color, temp, and condition),
Breath sounds, Description of the IV infusion site
• Observe the patient during the first 5-10 minutes of the transfusion to watch for immediate signs of acute reaction
• Complete reassessment at 15 minutes into transfusion
Assessment, Administration and
Transfusion Reactions (Cont.)
• Then hourly VS and IV site checks, as well as 1 hour after transfusion
• Document: physical assessment and reason for transfusion, VS prior to and at
15 min/ and hourly
• If a transfusion reaction is suspected immediately STOP the transfusion and notify a physician.
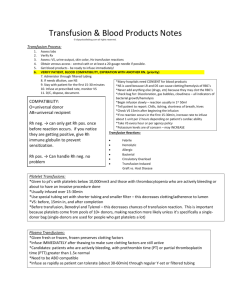
Blood Group
O
A
B
AB
Rh Type
Positive
Negative
Blood Compatibilities
Compatible RBC’s Compatible
Plasma/Platelets
O O, A, B, AB
A, O
B, O
A, AB
B, AB
AB, A, B, O AB
RBC Rh Type Plasma Rh Type for
Transfusion
Positive or Negative Positive or Negative
Negative Positive or Negative