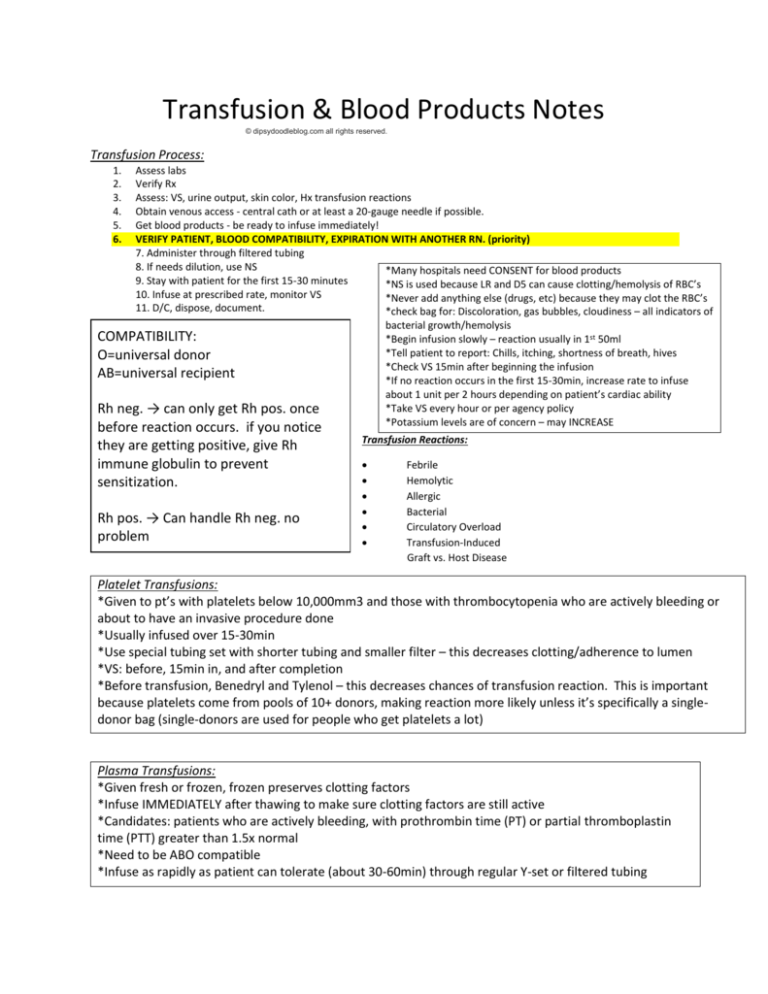
Transfusion & Blood Products Notes
© dipsydoodleblog.com all rights reserved.
Transfusion Process:
1.
2.
3.
4.
5.
6.
Assess labs
Verify Rx
Assess: VS, urine output, skin color, Hx transfusion reactions
Obtain venous access - central cath or at least a 20-gauge needle if possible.
Get blood products - be ready to infuse immediately!
VERIFY PATIENT, BLOOD COMPATIBILITY, EXPIRATION WITH ANOTHER RN. (priority)
7. Administer through filtered tubing
8. If needs dilution, use NS
*Many hospitals need CONSENT for blood products
9. Stay with patient for the first 15-30 minutes
*NS is used because LR and D5 can cause clotting/hemolysis of RBC’s
10. Infuse at prescribed rate, monitor VS
*Never add anything else (drugs, etc) because they may clot the RBC’s
11. D/C, dispose, document.
*check bag for: Discoloration, gas bubbles, cloudiness – all indicators of
bacterial growth/hemolysis
*Begin infusion slowly – reaction usually in 1st 50ml
*Tell patient to report: Chills, itching, shortness of breath, hives
*Check VS 15min after beginning the infusion
*If no reaction occurs in the first 15-30min, increase rate to infuse
about 1 unit per 2 hours depending on patient’s cardiac ability
*Take VS every hour or per agency policy
*Potassium levels are of concern – may INCREASE
COMPATIBILITY:
O=universal donor
AB=universal recipient
Rh neg. → can only get Rh pos. once
before reaction occurs. if you notice
they are getting positive, give Rh
immune globulin to prevent
sensitization.
Rh pos. → Can handle Rh neg. no
problem
Transfusion Reactions:
Febrile
Hemolytic
Allergic
Bacterial
Circulatory Overload
Transfusion-Induced
Graft vs. Host Disease
Platelet Transfusions:
*Given to pt’s with platelets below 10,000mm3 and those with thrombocytopenia who are actively bleeding or
about to have an invasive procedure done
*Usually infused over 15-30min
*Use special tubing set with shorter tubing and smaller filter – this decreases clotting/adherence to lumen
*VS: before, 15min in, and after completion
*Before transfusion, Benedryl and Tylenol – this decreases chances of transfusion reaction. This is important
because platelets come from pools of 10+ donors, making reaction more likely unless it’s specifically a singledonor bag (single-donors are used for people who get platelets a lot)
Plasma Transfusions:
*Given fresh or frozen, frozen preserves clotting factors
*Infuse IMMEDIATELY after thawing to make sure clotting factors are still active
*Candidates: patients who are actively bleeding, with prothrombin time (PT) or partial thromboplastin
time (PTT) greater than 1.5x normal
*Need to be ABO compatible
*Infuse as rapidly as patient can tolerate (about 30-60min) through regular Y-set or filtered tubing
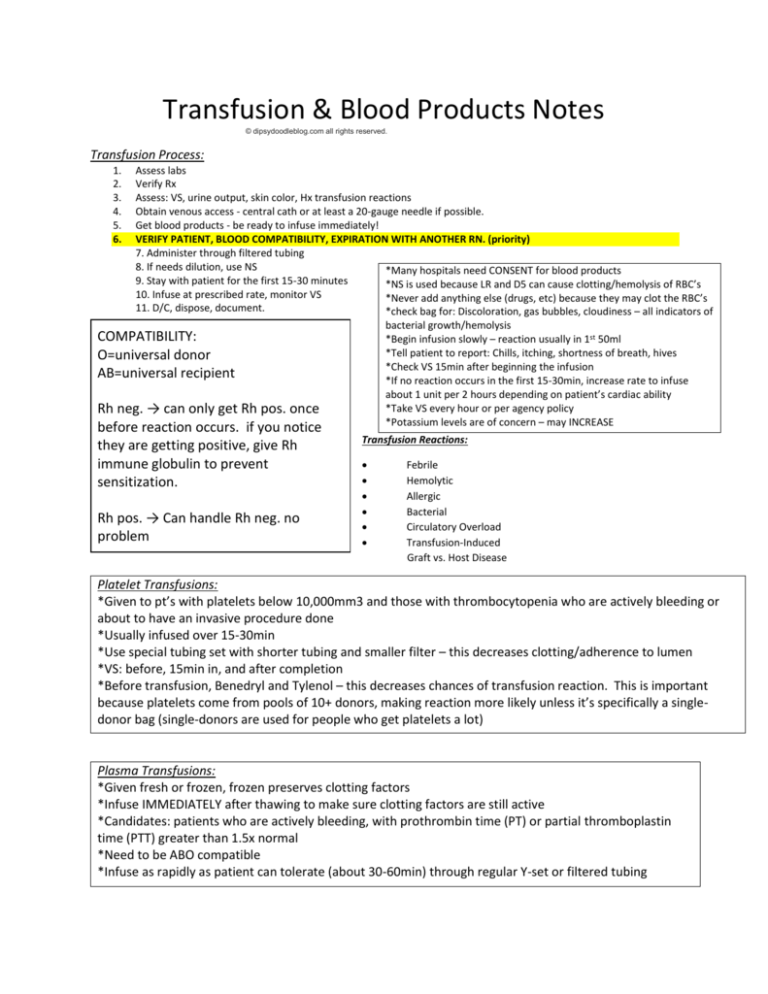
Febrile Usually after multiple transfusions.
*Chills
*Tachycardia
*Fever
*HYPOtension
*Tachypnea
Prevention: leukocyte reduced blood or single pool plasma. Also use
WBC filter.
Hemolytic Caused by ABO/Rh incompatibility. Reaction may be
mild (fever, chills) or severe (DIC)
*Fever
*Chills
*Apprehension
*Headache
*Chest pain
*Low back pain
*Tachycardia
*Tachypnea
*HYPOtension
*Hemoglobinuria
*Sense of doom
Allergic Usually in pts with Hx allergy. Shows up up to 24hr after
transfusion.
*Urticaria
*Itching
*Bronchospasm
*Anaphylaxis
Bacterial Result of infusion of contaminated blood/products
*Tachycardia
*HYPOtension
*Fever
*Chills
*Shock
Circulatory Overload Infused too quickly, usually w/ whole
blood or multiple transfusions. Older adults @ risk.
*HYPERtension
*Bounding pulse
*Distended jugular veins
*Restless
*Dyspnea
*Confusion
Nursing Action: Monitor I&O’s, Slow infusion, Give diuretics
Transfusion Induced Graft Vs Host Disease life threatening.
Manifestations within 1-2 weeks.
*Thrombocytopenia
*Anorexia, N&V
*Chronic hepatitis
*Recurrent Infection
*Weight loss