Blood-Replacement-KEY
advertisement

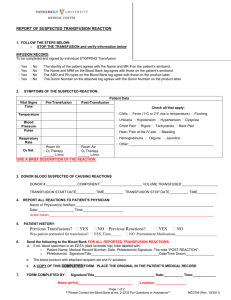
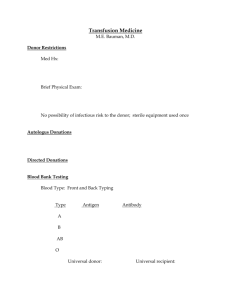
SURGICAL SKILLS LAB BLOOD REPLACEMENT 1. List 3 objectives for blood transfusion. Replace lost volume Replace low Hgb Improve oxygenation if low 2. Define the following terms a. Agglutinin An agglutinin is a substance that causes particles to coagulate to form a thickened mass Agglutinins can be antibodies that cause antigens to aggregate by binding to the antigen-binding sites of antibodies b. Antigen An antigen is a substance/molecule that, when introduced into the body, triggers the production of an antibody by the immune system, which will then kill or neutralize the antigen that is recognized as a foreign and potentially harmful invader. c. Autologous donor Self donor of blood for own surgery d. ABO Universal blood typing system that identifies antigens on RBC’s e. Rh Individuals either have, or do not have, the "Rhesus factor" on the surface of their red blood cells. The Rh blood group system currently consists of 50 defined blood-group antigens 3. The universal donor has the blood group _____O neg_______________. 4. The blood group of the universal recipient is ___AB+_______________. 5. The nurse must check which of the following with another nurse before initiating the transfusion? a. ABO and Rh b. Patient name. c. Unit number on compatibility tag. d. Expiration date. e. All of the above. Copyright 2011, Keith Rischer/www.KeithRN.com 6. The recommended rate of infusion for a unit of whole blood or packed RBC’s is ___2____ hrs, but not longer than ______4____hrs. 7. Clients particularly at risk for circulatory overload are _renal disease_____________, ____heart failure____________, and __elderly____________________ 8. Needle size for blood transfusion is #____18_____ to #__20___________ gauge. 9. Infusion for blood must always have a ___NS___________ and a __blood__________ administration set. 10. The client is particularly at risk for a transfusion reaction during the first 15 minutes. List nursing action you will do to monitor the client for signs/symptoms of a reaction. 1. double check all required components with second RN 2. VS at baseline especially temp and 15”, every hour of infusion, and end 3. Slow rate to ½ ordered first 15” 4. Stay with patient first 15” to observe 11. List 5 signs and symptoms most commonly associated with transfusion reaction. a.fever-febrile b.chills-febrile c.rash/hives-allergic d.SOB-hemolytic e. hypotension-hemolytic 12. IV tubing should always be primed with which IV solution? ___NS___________. Why? Cell lysis 13. Nursing actions for blood transfusion reaction STOP transfusion stat & disconnect Maintain IV site-disconnect from IV and flush with NS Recheck ID Notify blood bank/MD Monitor VS Treat sx per MD orders Save bag and tubing-send to blood bank Document per policy