the role of developmental therapy in a surgical neonatal unit

THE ROLE OF DEVELOPMENTAL POSITIONING IN NEONATES K F Lyons
Preterm Neonate
Congenital Abnormalities
5% of Neonates 95% Survive
Evidence to support developmental delay in Surgical Neonates with normal neurology
Laing S et al (2011). Early development of children with major birth defects requiring newborn surgery. Journal of Paediatrics and Child Health. 47:140-147 118 infants with congenital abnormalities following surgery during the neonatal period 26% had motor delay, 20% global delay
Newborn
• Physiological flexion • Protraction of shoulders and posterior pelvic tilt • Vital for development of normal body movement and control
Surgical neonate
• Ventilated • Sedated for long periods • Muscle relaxed
Muscle weakness
Muscle imbalance
• Take up surface • Lack of movement against gravity • Stay where placed • Poor co-contraction • Head turning preference • Poor feeding pattern
Developmentally delayed
Evidence of low central stability
Danser E et al (2013).Preschool neurological assessment in congenital diaphragmatic hernia survivors: Outcome and perinatal factors associated with neurodevelopmental impairment. Early human dev.
89: 393-400.
CDH survivors 22% motor delay, additional 14% severe delay.
Hypotonicity was found in 33% of patients
Postures
Risk factors
• Low birth weight • Critical illness • Multiple surgery • Ventilation time • Prolonged oxygen requirement • Poor nutrition • Interrupted sleep patterns • Prolonged hospitalisation
Positionally and Environmentally Challenged
Extended
Floppy
Asymmetrical
• Head turning preference • Plagiocephaly • No midline development • Poor communication
Cognitive Sensory Medically stable Posture Development Communication Feeding
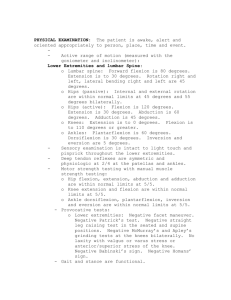
Current Practice
Support in flexion
Positioning Aids
Z-Flo/ Tortoise
The Leckey Infant Positioning System (IPS)
Enhanced supine support • Greater amount of containment • Consistent flexion • Mechanical advantage abdominals
Audit of infants requiring additional support
Poddle pod
Problem solve
Minimise abnormal postures for maximum function
• No midline development • No self consoling • Affecting vision and communication • Inhibiting skill acquisition • Contracture formation
Unsupported v supported
Enable midline and symmetry
Support in consistent flexion
Support in consistent flexion
Additional support
Contain and inhibit
Additional support
Contain and inhibit
Head turning preference
Orthopaedic problems
Risk assessment
• Environment • Support required
Check equipment
• Support when needed and allow for difficulties
Normalise Handling
Facilitate movement
Be inventive
Minimise Risk
Thanks for Listening