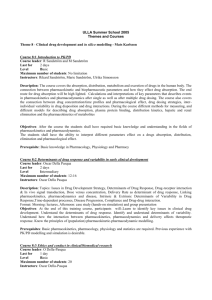
essential drug list
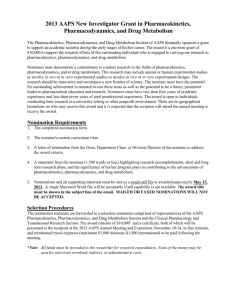
advertisement

YEAR 2 PHARMACOLOGY & THERAPEUTICS ESSENTIAL DRUG LIST Alexandra Burke-Smith 1. Drugs and the Autonomic Nervous System Overview of the ANS Sympathetic NS = “fight or flight”, Parasympathetic NS = “rest + digest” • NT = Ach + NA • Ach Receptors: nicotinic + muscarinic cholinoceptors • • • Nicotinic = ionotrophic (ligand-gated ion channel) Muscarinic – metabotrophic (G-protein) Muscarinic subtypes: • • • • M1 – neural (excitatory) M2 – cardiac (inhibitory) M3 – exocrine (excitatory) NA receptors: adrenoceptors • • • • A1 > PLC > IP3 + DAG > PKC + Ca2+ A2 > cAMP > PKA B1 > cAMP > PKA B2 > cAMP > PKA Cholinomimetics • “drugs which mimic the action of Acetylcholine (Ach agonists)” – Principally mimic parasympathetic NS – Directly acting: choline esters + alkaloids that have agonistic action at Ach receptors – Indirectly acting: anticholinesterases that potentiate the action of Ach; preventing its breakdown by inhibiting acetylcholinesterase and/or butyrylcholinesterase (plasma ezyme) • Reversible = alkaloid carbamyl esters • Irreversible = organophosphate compounds Drug Acetylcholine (choline ester; neurotransmitter) Class Directly acting cholinomimetic Pharmacodynamics (MOA) Agonist at nicotinic + muscarinic Ach receptors (parasympathetic + sympathetic action) Pharmacokinetics Metabolism: cholinesterases Duration of action: seconds Notes: No therapeutic use as non-selective and quickly degraded Drug Pilocarpine Class Directly acting cholinomimetic (alkaloid) Pharmacodynamics (MOA) Partial agonist at muscarinic Ach receptors (parasympathetic activation) Clinical Use Treat glaucoma (contraction of ciliary muscle + sphincter pupillae > miosis + improved drainage of aqueous humour) Pharmacokinetics Administration: locally as eyedrops Half-life: 3-4 hours Side Effects Predicted by PNS actions: Blurred vision, sweating, GI disturbance, hypotension, respiratory distress Drug Bethanechol (choline ester) Class Directly acting cholinomimetic Pharmacodynamics (MOA) M3 (exocrine + smooth muscle) Ach receptor agonist (parasympathetic action) Clinical Use Assist bladder emptying + enhance gastric motility Pharmacokinetics Orally active Half-life 3-4 hours Side Effects Sweating, impaired vision, nausea, bradycardia, hypotension + respiratory difficulty Other Relevant Information: Similar in structure to Ach; added methyl group means resistant to degradation Drug Phyostigmine (alkaloid carbamyl ester) Class Indirectly acting cholinomimetic (reversible anticholinesterase) Pharmacodynamics (MOA) Competitive inhibitor of cholinesterase enzyme (donates carbamyl group which blocks active site) > parasympethetic + sympathetic action (primarily acts on PNS) by prolonging Ach activity Clinical Use Treatment of glaucoma Treat atropine poisoning (Ach antagonist) Pharmacokinetics Half-life 30 minutes (carbamyl group removed by slow hydrolysis) Drug Ecothipate (organophosphate compound) Class Indirect cholinomimetic (irreversible anticholinesterase) Pharmacodynamics (MOA) inhibitor of cholinesterase enzyme (reacts with enzyme active site; blocking it with stable group ) > parasympethetic + sympathetic action (primarily acts on PNS) by prolonging Ach activity Clinical Use Treatment of glaucoma Pharmacokinetics Administered as eye drops Duration of action weeks (new cholinesterase enzyme must be synthesised) Side Effects Sweating, blurred vision, GI pain, bradycardia, hypotension, respiratory difficulty Cholinoceptor Antagonists • “drugs which show affinity but no efficacy at Ach receptors, thus preventing agonists from transducing a response and activating intracellular signalling pathways” Drug Hexamethonium Class Nicotinic receptor antagonist Pharmacodynamics (MOA) Competitive antagonistic action at all autonomic ganglia Clinical Use First anti-hypertensive (inhibition of sympathetically driven kidneys + blood vessels) No longer used clinically Side Effects Parasympethetically driven side-effects (ie what happens when you block the PNS) Loss of bladder control, pupil dilation, loss of GI motility + secretions Drug Trimetaphan Class Nicotinic cholinoceptor antagonist Pharmacodynamics (MOA) Ganglion blocking drug; not technically a nicotinic receptor antagonist, but blocks ion channels (use-dependent block; more agonist > more block) Clinical Use Controlled hypotension during surgery Pharmacokinetics IV administration Duration of action 2-3 minutes Drug Atropine Class Competitive muscarinic cholinoceptor antagonist Pharmacodynamics (MOA) Competitively inhibits parasympethetic (+ sympathetic) action at mAChR Clinical Use Anaesthetic premedication (dilate bronchi, dry throat + reduce lung secretion > easier to administer gas mask + reduced aspiration risk) Treatment of sinus bradycardia (normal, slow rhythm) Pharmacokinetics Oral administration Hepatic metabolism Duration of action 2-3 hours Side Effects Dry mouth, blurred vision, urinary retention, pupil dilation, irritability, hyperactivity Other relevant information: NB: atropine poisoning may occur in children who eat the deadly nightshade. This is treated with phyostigmine (see earlier) Drug Hyoscine Class Competitive muscarinic cholinoceptor antagonist Pharmacodynamics (MOA) Competitively inhibits parasympethetic (+ sympathetic) action at mAChR Clinical Use Anaesthetic premedication (dilate bronchi, dry throat + reduce lung secretion > easier to administer gas mask + reduced aspiration risk) Treatment of sinus bradycardia Motion sickness (reduces flow of information from Labyrinth to vomiting centre) Parkinsons (reduces inhibitory effect of M4 receptors on dopamine signalling) Pharmacokinetics Administered orally or transdermally Duration of action 2-3 hours Side Effects Decreased sweating, reduced secretions, blurred vision, agitation, restlessness, confusion Drug Tropicamide Class Competitive muscarinic cholinoceptor antagonist Pharmacodynamics (MOA) Acts on M3 receptors within the iris of the eye to cause pupil dilation (reduces ciliary + sphincter pupillae constriction) Clinical Use Dilation of pupil for retina examination Pharmacokinetics Administered as eye drops Side Effects Dry mouth, blurred vision, urinary retention Drug Ipratropium Bromide Class Competitive muscarinic cholinoceptor antagonist Pharmacodynamics (MOA) Antagonism removes PNS bronchostrictor effect in lungs Clinical Use Used to treat asthma and COPD Pharmacokinetics Administered as aerosol Other Relevant Information: Quaternary amine structure localises response as positive charge prevents crossing of lipid membrane in lungs Sympathomimetics • SNS agonists • Act on adrenoreceptors of post-ganglionic SNS neurons • Directly acting: mimic actions of NA/A by binding and stimulating adrenoceptors – used principally for actions in CVS, eyes + lungs • Indirectly acting: act at the adrenergic nerve terminal as opposed to adrenoceptor Class Directly acting sympathomimetic Pharmacodynamics (MOA) Non-selective (alpha + beta) agonists acting at adrenoceptors of SNS Clinical Use Anaphylaxis: • B2 action = dilation of skeletal blood vessels > decreased TPR, bronchodilation + reduced inflammatory mediator production • A1 action = profound subcutaneous vasoconstriction > increased BP • B1 action = positive chronotropic + inotropic COPD Acute heart block Anaesthesia (vasoconstriction used to localise effect) Glaucoma (a1 mediated vasoconstriction + B mediated decreased aqueous humour production) Pharmacokinetics Administered IV, IM or locally (eye drops) Poorly absorbed Duration of action minutes Metabolised by MAO-A (uptake 1) and COMT (uptake 2) Side Effects Dry mouth, tachycardia, arrythmias, cold extremities, hypertension, tremor, palpitations Drug Phenylephrine Class Directly acting Alpha-1 selective sympathomimetic Pharmacodynamics (MOA) Selective action on alpha-1 adrenoceptors Clinical Use Stop superficial bleeding (vasoconstrictor) Mydriasis (a1 adrenoceptors > radial muscle constriction > pupil dilation) Nasal decongestant (reduced secretions) Pharmacokinetics Administered as eye drops, IV, intranasal Duration of action minutes Broken down by MAO Other Relevant Information: Chemically related to adrenaline, but more resistant to COMT Drug Clonidine Class Directly acting Alpha-2 selective sympathomimetic Pharmacodynamics (MOA) Agonistic action at alpha-2 adrenoceptors. A2 receptors present pre-synaptically; act to autoinhibit release of noradrenaline/adrenaline (reduce SNS action) Clinical Uses Treatment of hypertension + migraine. Reduces sympathetic tone via central action in brainstem within the baroreceptor pathway (reduced pre-synaptic release of NA) Pharmacokinetics Orally active Duration of action hours Broken down by COMT + MAO-A Drug Isoprenaline Class Directly acting non-selective B adrenoceptor agonist Pharmacodynamics (MOA) Acts to potentiate action of NA/A on beta adrenoceptors Clinical Uses Treat heart block Pharmacokinetics IV administration Broken down by COMT Duration of action hours Side Effects Fatal reflex tachycardia/dysrhythmias Other relevant information Difference in structure to adrenaline means less susceptible to metabolism by MAO-A Drug Dobutamine Class Directly acting beta-1 selective adrenoceptor agonist Pharmacodynamics (MOA) Potentiates NA/A action at beta-1 receptors Clinical Uses Acute heart block Pharmacokinetics Administered IV Half-life 2 minutes Rapidly metabolised by COMT Other relevant information Lacks isoprenaline’s reflex tachycardia due to lack of B2 action Drug Salbutamol Class Directly acting beta-2 selective sympathomimetic Pharmacodynamics (MOA) Agonistic action at beta-2 adrenoceptors Clinical Uses Asthma (relaxation of bronchial smooth muscle + inhibition of pro-inflammatory mediator release from mast cells) Treatment of threatened uncomplicated premature labour (relaxes uterus) Pharmacokinetics Administration via inhalation (ventolin) or IV (for premature pregnancy) Duration of action hours Side Effects Some reflex tachycardia, tremor Contraindications Patients with diabetes (B2 receptors mobilise glycogen) Other relevant information Relative resistance to metabolism by MAO and COMT Drug Cocaine Class Indirectly acting sympathomimetic Pharmacodynamics (MOA) Acts to prevent uptake 1 (no MAO metabolism) so there is greater concentration of catecholamines in synaptic cleft Pharmacokinetics Well absorbed from all sites + crosses BBB Metabolised by plasma esterases + hepatic enzymes Half-life 30 mins Excreted in urine Side Effects CNS: excitement + increased motor activity Activation of vomiting centres, tremors, convulsions CVS: tachycardia, vasoconstriction and hypertension Drug Tyramine (dietary amino acid found in cheese, red wine + soy sauce) Class Indirectly-acting sympathomimetic Pharmacodynamics (MOA) Some weak agonistic activity at post-synaptic adrenoceptors + competitive inhibition of uptake 1 Also displaces NA from intracellular vesicles, therefore increased cytosolic [NA] > leakage into synaptic cleft Pharmacokinetics Extensive first pass metabolism Side Effects Under normal conditions, no effect as undergoes extensive first pass metabolism However when MAOs are inhibited (eg use of antidepressants), ingestion of foods containing tyramine may cause hypertensive crisis known as CHEESE REACTION SNS Antagonists • Act with antagonistic action at adrenoceptors • These may be: – Non-selective – Non-selective alpha – Alpha 1 selective – Non selective beta – Beta 1 selective Drug Labetalol Class Directly acting Non-selective b1 and a1 SNS antagonist Pharmacodynamics (MOA) Antagonism > block of SNS activity Clinical Uses Hypertension (decreased renin secretion + peripheral subcutaneous vasoconstriction > decreased peripheral resistance) Pharmacokinetics Broken down by COMT + MAO-A Other relevant information No long-term change in heart rate or cardiac output Drug Propanolol Class Directly acting Non-selective B-adrenoceptor antagonists Pharmacodynamics (MOA) B-blocker > reduced SNS effects Clinical Uses Hypertension (reduced effect of exercise or stress) Anti-arrythmic (class II) Pharmacokinetics Orally active Broken down by COMT + MAO-A Duration of action hours Side Effects Bronchoconstriction, hypoglycaemia (loss of warning signs for diabetics eg palpitations), fatigue, cold extremities, bad dreams Contraindications Asthma Other relevant information Little cardiac effects at rest Drug Atenolol Class B1 selective (cardioselective) Directly actingBb1-selective blocker SNS antagonist Pharmacodynamics (MOA) Competitive antagonist “cardioseelctive” at B1 adrenoceptors – antagonises in heart, the effect thusof preventing action noradrenaline of NA (negative on the ionotropic heart + chronotropic effect) Angina, post MI,Hypertension cardiac dysrythmias, chronic heart failure, Angina hypertension Clinical Clinical Uses Uses Pharmacokinetics Side Effects Contraindications Other relevant information Atenolol down by COMT and MAO-A Clinical doses > Broken action on B2 receptors: Worsening of cardiac failure Bradycardia, bronchoconstriction, hypoglycaemia, fatigue, Asthma (despite less b2 effect) cold extremities, CNS effects eg nightmares Also use in glaucoma, migraine, benign essential tremor Not first line treatment for hypertension as does not reduce TPR Drug Phentolamine Class Directly acting Non-selective alpha-adrenoceptor antagonist Pharmacodynamics (MOA) Blockade of a1 receptors > vasodilation > fall in TPR + BP Blockade of a2 receptors > loss of inhibition of pre-synaptic NA release Clinical Uses No longer used clinically Side Effects Postural hypotension, diarrhoea, reflex tachycardia Drug Prazosin Class Directly acting a1 selective adrenoceptor antagonist Pharmacodynamics (MOA) Blockade of a1 > vasodilation > fall in TPR + BP (less reflex tachycardia) Clinical Uses Antihypertensive (minor use in associated dislipidaemia) Pharmacokinetics Broken down by COMT + MAO-A Side Effects Hypotension Modest decrease in LDL, increase in HDL Other relevant information Lack of a2 blockade > no change in synthesis and release of NA Drug Methyldopa Class SNS false transmitter Pharmacodynamics (MOA) Indirectly acting adrenoceptor antagonist; in the same way that DOPA is taken up and packaged into vesicles, methyldopa is packaged and hydroxylated to form false NT alpha-methyl-noradrenaline A-m-NA is released into the synaptic cleft, but has greatest activity on alpha 2 receptors to reduce NT release. Clinical Uses Antihypertensives (in patients with renal insufficiency) as maintains renal blood flow. Also in pregnancy-related hypertension, as no effect on foetus. Side Effects Dry mouth, sedation, orthostatic hypotension Other relevant information Not deaminated by MAO-A, therefore accumulates in synaptic cleft Neuromuscular Blocking Drugs • Drugs which act at the NMJ To prevent depolarisation of the motor end-plate – Non-depolarising: competitive antagonsts – Depolarising: agonists Drug Tubocurarine Class Non-depolarising NM blocking drug Pharmacodynamics (MOA) Competitive nicotinic Ach receptor antagonist which produces a graded block of somatic NMJs Clinical Uses Surgery (reduces amount of anaesthetic required + allows for artificial ventilation) Pharmacokinetics Administered IV Doesn’t cross BBB or placenta Onset of action within 2-3 mins Duration of action 40-60 mins Not metabolised, excreted in bile + urine Side Effects Flaccid paralysis (onset in order…) 1. Extrinsic eye muscles > double vision 2. Small muscle paralysis of face, limbs + pharynx 3. Respiratory muscle paralysis Unwanted effects: Ganglion block + histamine release from mast cells > decreased TPR + bronchospasm Contraindications Renal/hepatic impairment Other relevant information Naturally occurring quaternary ammonium alkaloid Reversed by anticholinesterases; recovery of movement is in reverse order to effects Drug Atracurium Class Non-depolarising NM blocker Pharmacodynamics (MOA) Competitive nAChR antagonist (somatic NMJ blocked) Pharmacokinetics Shorter duration of action than Tubocurarine Drug Suxamethonium Class Depolarising NM blocker Pharmacodynamics (MOA) Post-synaptic nAChR agonist, therefore causes prolonged excitation. This prevents new action potential generation, thus inactivating ion channels (somatic NMJ blocked) Pharmacokinetics Degraded by butyrylcholinesterases (plasma enzyme) Duration of action mins (use in short term endotracheal intubation) Other relevant information Structure related to acetylcholine Different to HEXAmethonium = nAChR antagonist 2. Drugs and the Cardiovascular System RAAS • RAAS = renin angiotensin aldosterone system – Primarily responsible for fluid + BP regulation • Drugs interfering with RAAS: – ACE inhibitors – Angiotensin II receptor antagonists (ARB) – Renin inhibitors, eg Aliskiren (no significant clinical experience) Drug Enalapril Class ACE inhibitor Pharmacodynamics (MOA) Inhibits the somatic form of ACE, thus preventing the conversion of Ang I > Ang II Clinical Uses Used in conditions which confer increased CV risk: Hypertension, heart failure, post MI, diabetic nephropathy, progressive renal insufficiency Side Effects Hypotension, dry cough, urticaria + angioedema, hyperkalemia, fetal injury, renal failure (in patients with renal artery stenosis) Other relevant information Germline form of ACE is significantly different, therefore not affected Drug Captopril Class ACE inhibitor Pharmacodynamics (MOA) Inhibits the somatic form of ACE, thus preventing the conversion of Ang I > Ang II Clinical Uses Used in conditions which confer increased CV risk: Hypertension, heart failure, post MI, diabetic nephropathy, progressive renal insufficiency Side Effects Hypotension, dry cough, urticaria + angioedema, hyperkalemia, fetal injury, renal failure (in patients with renal artery stenosis) Other relevant information Germline form of ACE is significantly different, therefore not affected Drug Losartan Class Angiotensin Receptor Blocker Pharmacodynamics (MOA) Non-competitive Antagonist of type 1 receptors for Ang II, thus preventing renal and vascular actions of Ang II Clinical Uses Hypertension, chronic heart failure Side Effects Hypotension, hyperkalemia, fetal injury, renal failure (in patients with renal artery stenosis) Other relevant information Fewer side effects than ACE inhibitors Calcium Antagonists • Rise in intracellular calcium key step in excitationcontraction coupling in both cardiac and vascular myocytes • Involves L-type voltage-dependent calcium channel • 2 classes of calcium channel blockers (CCBs) – Rate limiting (bind to IC domain of receptor; exert both cardiac and smooth muscle effects) – Non-rate slowing (bind to EC domain of receptor; exerts only smooth muscle action), eg amlodipine Drug Verapamil Class Rate-limiting calcium channel blocker Pharmacodynamics (MOA) Binds to the intracellular domain of L-type calcium channel receptor, blocking influx of calcium • Negative chronotropic + ionotropic effects on heart and smooth muscle Clinical Uses Angina (arising from IHD) Antidysrhythmias Pharmacokinetics Oral administration Duration of action 6-8 hours Hepatic metabolism Side Effects Bradycardia, AV block, negative ionotropic effect (worsening of HF), constipation (effect on GI smooth muscle) Drug Diltiazem Class Rate-limiting calcium channel blocker Pharmacodynamics (MOA) Binds to the intracellular domain of L-type calcium channel receptor, blocking influx of calcium • Negative chronotropic + ionotropic effects on heart and smooth muscle Clinical Uses Angina (arising from IHD) Antidysrhythmias Pharmacokinetics Oral administration Duration of action 6-8 hours Hepatic metabolism Side Effects Bradycardia, AV block, negative ionotropic effect (worsening of HF), constipation (effect on GI smooth muscle) Beta Blockers • Sympathetic neurons innervating cardiac muscle release NA on depolarisation • NA acts on B1 receptors on cardiac myocytes, to increase heart rate, contractility and excitability • Competitive antagonists, ie beta blockers, thus tend to have a negative chronotropic and ionotropic effect Drug Atenolol Class B1 selective (cardioselective) B blocker Pharmacodynamics (MOA) Competitive antagonist at B1 adrenoceptors in heart, thus preventing action of NA (negative ionotropic + chronotropic effect) Clinical Uses Angina, post MI, cardiac dysrythmias, chronic heart failure, hypertension (not first line for hypertension as no TPR effect) Side Effects Clinical doses > action on B2 receptors: Worsening of cardiac failure Bradycardia, bronchoconstriction, hypoglycaemia, fatigue, cold extremities, CNS effects eg nightmares Other relevant information Also use in glaucoma, migraine, benign essential tremor Not first line treatment for hypertension as does not reduce TPR Organic Nitrates + Related Agents • Organic nitrite is absorbed (particularly in SMC), where it undergoes degradation into nitrite free radical, then converted to nitric oxide • Nitric oxide is an endogenous vasodilator; it acts on guanylate cyclase to increase cGMP production • cGMP then acts to vasodilate the smooth muscle Drug Glyceryl Trinitrate Class Nitrate Pharmacodynamics (MOA) Directly causes release of NO in smooth muscle cells, as well as minor release in platelets. Vasodilation reduces venous return and total peripheral resistance, thus reduces preload and afterload, and therefore the heart does not need to work as hard Clinical Uses Angina Heart failure BP control during anaesthesia (easy to titrate) Pharmacokinetics Undergoes extensive first pass metabolism by the liver, therefore administered sublingually for rapid relief, or via transdermal patch for long term use Half life approx 5 mins Side Effects Vasodilation > hypotension, headaches, flushing Other relevant information Long term use associated with tolerance; one of the reasons GTN is used for immediate relief Often used in conjunction with beta blockers for treatment of angina Drug Nicorandil Class Nitrate; stimulates guanylate cyclase to cause vasodilation Pharmacodynamics (MOA) Guanylate cyclase acts to increase cGMP production, which causes myocyte vasodilation Clinical Uses Used to increased oxygen supply to coronary vessels, and increase venous capacitance (often post MI) Pharmacokinetics Hepatic metabolism Side Effects Vasodilation > hypotension, headaches, flushing Reflex tachycardia Anti-dysrhythmics • Arrythmias/dysrhythmias = abnormalities of cardiac rhythm • Classified according to association with heart rate (tachy = increase, brady = decrease), and site of origin: – Supraventricular: arise from atria and conduction tissue – Ventricular: arise from ventricles – Complex: multiple sites of origin Drug Amiodarone Class Antidysrhythmic Pharmacodynamics (MOA) Wide spectrum anti-dysrhythmic with complex MOA involving multiple ion channel blocks Clinical Uses Supraventricular + ventricular arrythmias Pharmacokinetics Half life 10-100 days Side Effects Accumulates in the body, therefore number of adverse effects: photosensitive skin rash, hypo/hyperthyroidism, pulmonary fibrosis Drug Diltiazem Class Rate-limiting calcium channel blocker (class IV antiarrhythmic) Pharmacodynamics (MOA) Binds to the intracellular domain of L-type calcium channel receptor, blocking influx of calcium • Negative chronotropic + ionotropic effects on heart and smooth muscle Clinical Uses Angina (arising from IHD) Tachyarrythmias Pharmacokinetics Oral administration Duration of action 6-8 hours Hepatic metabolism Side Effects Bradycardia, AV block, negative ionotropic effect (worsening of HF), constipation (effect on GI smooth muscle) Drug Verapamil Class Rate-limiting calcium channel blocker Pharmacodynamics (MOA) Binds to the intracellular domain of L-type calcium channel receptor, blocking influx of calcium • Negative chronotropic + ionotropic effects on heart and smooth muscle Clinical Uses Tachyarrythmias Pharmacokinetics Oral administration Duration of action 6-8 hours Hepatic metabolism Side Effects Bradycardia, AV block, negative ionotropic effect (worsening of HF), constipation (effect on GI smooth muscle) Drug Digoxin Class Cardiac glycoside Pharmacodynamics (MOA) CVS: Inhibition of Na-K ATPase > accumulation of intracellular Ca2+ via Na/Ca exchanger = positive ionotropic CNS: increased vagal outflow > increased refractory period + reduced rate of conduction through AVN = negative chronotropic Clinical Uses Atrial fibrillation Pharmacokinetics T ½ 40 hours Narrow therapeutic index Side Effects New dysrhythmia, eg AV conduction block Other relevant information AF may cause thrombus formation in the atrium; embolus to the brain may cause a stroke High risk of digoxin toxicity; treated with immune Fab digibind, which “mops up” excess Other Cardiac Drugs Drug Doxazosin Class Competitive alpha-1 adrenoceptor antagonist Pharmacodynamics (MOA) Competes with NA for active site of alpha-1 adrenoceptors, thereby preventing vasoconstrictor action > coronary vasodilation Clinical Uses Used in conjunction with antihypertensives in resistant hypertension Side Effects Increased rate of chronic heart failure Drug Sumitriptan Class 5HT1D receptor agonist Pharmacodynamics (MOA) Acts on seratonin receptor to inhibit trigeminal nerve transmission and constrict cerebral and coronary arteries Clinical Uses Treatment of migraine Contraindications Coronary disease – causes coronary vasoconstriction Anti-Thrombotics + Anti-Coagulants • Drugs that interfere with normal haemostasis and thrombosis pathways • Haemostasis: the essential physiological process where blood coagulation prevents excess blood loss • Thrombosis: the pathophysiological process where blood coagulation occurs within an INTACT blood vessel and obstructs blood flow – venous thrombosis = red thrombi (high fibrin) – Arterial thrombosis = white thrombi (high platelet) • Virchow’s triad (addresses why thrombi may form): – Rate of blood flow – slow/stagnating – Consistency of blood – viscous [more procoagulation factors] – Blood vessel wall integrity – atherosclerotic • Drugs that target = anti-coagulants, anti-platelets, thrombolytics Anti-Coagulants • Target the initial phase of the clotting cascade, which occurs following tissue factor exposure • 4 types of drugs: – Direct thrombin inhibitors, eg Hirudin – Heparin + derivatives – Factor Xa inhibitors – Vitamin K antagonists Drug Heparin Class Anti-coagulant Pharmacodynamics (MOA) Natural anti-coagulant found on mast cells in the body; exerts a conformational change which activates antithrombin III, potently inactivating thrombin Clinical Uses Immediate anticoagulation in venous thrombosis + pulmonary embolism Pharmacokinetics Heparin = continuous infusion, short half life LMW derivatives = longer half life, not orally available but only require regular administration Side Effects Haemorrhage, hypersensitivity reactions, thrombocytopenia, osteoporosis, hypoaldosteronism Other relevant information Derivatives also inhibit Factor X, therefore preventing formation of prothrombinase complex To reverse effects. Promatine can be given IV (forms inactive complex) Drug Warfarin Class Vitamin K antagonist (anti-coagulant) Pharmacodynamics (MOA) Vitamin K is essential for clotting factor synthesis, therefore prevents normal clotting cascade Clinical Uses Long term anticoagulation following thrombosis or MI Pharmacokinetics Oral administration Delayed onset of action (5 days) Narrow therapeutic window, strongly plasma protein bound Side Effects Haemorrhage, teratogenic Other relevant information Numerous drug interactions which make pharmacokinetics more complex – requires INR monitoring. This is because highly plasma protein bound therefore changes in pp binding affect bioavailability Anti-Platelets • Used in CV disease as thrombosis prevention • If AT-III does not inactivate thrombin, thrombin activates platelets > production of clotting factors and ADP – Thrombin also releases endothelial bound vWF, which activates factor II > IIa (thrombin) • ADP acts on active platelets via P2Y receptors, leading to platelet aggregation and formation of a clot • Anti-platelets include: – – – – PAR antagonists (protease activated receptor) ADP receptor antagonists COX inhibitors Glycoprotein Iib/IIIa receptor antagonists Drug Clopidogrel Class ADP receptor antagonist Pharmacodynamics (MOA) Prevents platelet plug formation. ADP binding leads to the expression of GpIIb/IIIa, which act as a molecular glue for the formation of the unstable plug Clinical Uses Anti-platelet Pharmacokinetics Oral administration Other relevant information Drug of choice in aspirin-sensitive patients Drug Apirin Class COX inhibitor Pharmacodynamics (MOA) PAR activation liberates arachidonic acid. The action of COX on arachidonic acid in platelets generates thromboxane-A2 (pro-coagulant), therefore prevents this Clinical Uses Anti-platelet Pharmacokinetics Administered orally at low dose (75mg) Side Effects Reyes syndrome, bronchospasm, GI bleeding and stomach ulcers Contraindications Children under 16, haemophiliacs, asthmatics Drug Abciximab Class Glycoprotein IIb/IIIa antagonist Pharmacodynamics (MOA) ADP receptor binding + thromboxane A2 lead to expression of GpIIb/IIIa. These act as a molecular glue in the formation of unstable platelet plug Clinical Uses Anti-platelet Treatment of thrombotic disorders Pharmacokinetics IV administration Other relevant information Only single use, therefore used in high risk patients Thrombolytics • Large scale thrombin converts fibrinogen to fibrin. • Fibrin strands wrap around the clot, with the eventual formation of a thrombus within the intact blood vessel • Fibrinolytics are effective at removing preformed clots. They convert plasminogen to plasmin, a natural protease that digests fibrin strands Drug Alteplase Class Thrombolytic/fibrinolytic/clot buster Pharmacodynamics (MOA) Recombinant tissue type plasminogen activator (tPA) > degradation of fibrin clot and release of fibrin degradation products Clinical Uses Acute MI and ischaemic stroke Pharmacokinetics IV short infusion Duration of action hours Other relevant information Needs to be given within 12 hours of symptom onset Drug Streptokinase Class Thrombolytic/fibrinolytic/clot buster Pharmacodynamics (MOA) Bacterial product that binds to plasminogen, causing a conformational change that exposes the active site Clinical Uses Reduce mortality from acute MI Pharmacokinetics IV short infusion Half life 3-4 hours Side Effects Bleeding, GI haemorrhage, stroke Other relevant information Tolerance develops after first administration; develop immunity to bacterial antigens Cholesterol Drugs • Hypercholesteramia is a key risk factor in the development of atherosclerosis • LDL cholesterol is the primary target to prevent atherosclerotic plaques + CHD • Different classes of drugs include: – – – – Statins Bile acid sequestrants Nicotinic acid Fibrates • Triglycerides are also associated with an increased risk of CHD, therefore are an important target. However this mechanism is not fully understood Statins • First-line drugs in treatment of dyslipidaemias • MOA: inhibition of HMG-CoA reductase (ratelimiting enzyme in cholesterol synthesis) • In response to this… – Hepatocytes up-regulate/increase number of LDL receptors, increasing binding and removal of LDL cholesterol from the plasma – Increase in HDL cholesterol (mechanism not fully understood) Drug Simvastatin Class Statin Pharmacodynamics (MOA) HMG-CoA reductase inhibitor – inhibits cholesterol synthesis. Effects include: • Raised HDL • Lowered LDL • Formation of plaque stabilisers Clinical Uses Hypercholesteramia, dyslipidaemia Pharmacokinetics Oral administration Hepatic metabolism Half life 1-2 hours Side Effects Caused by non-selective effects on body (target organ is liver) Other relevant information COCHRANE review has shown reservation in use of statins in primary prevention 3. Diuretics Diuretics • Drugs that act on the renal tubule to promote an increased loss of water in the urine = diuresis • Gross structure of renal tubule can be divided into 4 sections: – Proximal convoluted tubule – Loop of Henle (descending and ascending limb) – Distal convoluted tubule – Collecting duct • There are 5 main classes of diuretics, each with a different MOA: – Osmotic diuretics – act on entire kidney tubule – Carbonic anhydrase inhibitors – act principally on PCT – Loop diuretics – act on ascending limb of LOH – Thiazides – act on early DCT – Potassium sparing diuretics – act on late DCT and collecting duct Drug Mannitol Class Osmotic diuretic Pharmacodynamics (MOA) Pharmacologically inert substance which is freely filtered into kidney lumen, but poorly reabsorbed. Therefore increases osmolarity of kidney filtrate, and decreases water absorption where the nephron is freely permeable to water (PCT, descending LOH, CT) Clinical Uses Prevention of acute renal failure Decreasing intra-cranial pressure, intraocular pressure Pharmacokinetics IV administration Side Effects Increased ECF volume > hyponatremia. This may cause nausea, vomiting, headache + pulmonary oedema Carbonic Anhydrase Inhibitors Drug Acetazolamide Class Carbonic anhydrase inhibitor Pharmacodynamics (MOA) Inhibits action of CA, therefore increasing bicarbonate and sodium loss in the PCT. This reduces water reabsorption in the PCT as well as the CT Clinical Uses Renal stones Metabolic alkalosis Decreasing intra-ocular pressure (glaucoma) Altitude sickness Side Effects Hypokalemia, reduced H+ excretion > alkaline urine + metabolic acidosis Other relevant information Relatively weak; only act on PCT and further reabsorption of sodium occurs in later nephron Loop Diuretics Drug Frusemide Class Loop diuretic Pharmacodynamics (MOA) Acts to block the Na+-2Cl--K+ co-transporter on the apical membrane of the ascending limb, thus reducing the osmolarity of the medullary interstitium > less water reabsorption in descending limb + 15-30% more filtrate loss Clinical Uses Oedema (HF, pulmonary, renal, hepatic or cerebral) Moderate hypertension Hypercalcaemia, hyperkalemia Pharmacokinetics Oral or IV administration Half life 3-6 hours Excreted unmetabolised by kidney Side Effects Hypokalaemia, metabolic alkalosis, hypocalcaemia, and possibly hypotension, nausea and vomiting, and may induce an allergic reaction. Thiazides Drug Bendrofluazide Class Thiazides Pharmacodynamics (MOA) Blocks Na/Cl co-transporter in early DCT, thus increasing osmolarity of tubule lumen and Na+ delivery to late DCT and CT. This results in decreased water reabsorption, increased K+ loss, increased Mg2+ and Ca2+ reabsorption Clinical Uses Hypertension Cardiac failure, resistant oedema, nephrogenic diabetes insipidus (pradoxical effect here = anti-diuretic effect) Pharmacokinetics Oral administration Half life 24 hours Side Effects Hypokalemia metabolic alkalosis Diabetes mellitus Other relevant information Mild diuretic – first line treatment of hypertension in the elderly Potassium Sparing Diuretics Drug Spironolactone Class Potassium sparing diuretic Pharmacodynamics (MOA) Aldosterone receptor antagonist, therefore acts to inhibit Na+ reabsorption in late DCT, as well as concommitant K+ excretion (basal Na/K exchanger) Results in increased tubular osmolarity + water loss, with increased H+ retention (uric acid loss) Clinical Uses Used in primary and secondary hyperaldosteronism Pharmacokinetics Oral administration Duration of action days Side Effects Hyperkalemia, metabolic acidosis Gynaecomastia, menstrual disorders/testicular atrophy Drug Amiloride Class Potassium sparing diuretic Pharmacodynamics (MOA) Inhibitor of aldosterone-sensitive Na+ channel, , therefore acts to inhibit Na+ reabsorption in late DCT, as well as concommitant K+ excretion (basal Na/K exchanger) Results in increased tubular osmolarity + water loss, with increased H+ retention (uric acid loss) Clinical Uses Used in conjunction with other diuretics Side Effects Hyperkalemia and metabolic acidosis 4. NSAIDs NSAIDs • Inhibit COX enzyme; involved in rate limiting step of prostanoid synthesis, thus prevents production of prostaglandin H2 from arachidonic acid • Two isoforms of COX enzyme: – COX 1 – found in nearly all cells, actions tend to be homeostatic – COX 2 – found predominantly in pro-inflammatory cells • Actions of NSAIDs can be predicted by actions of prostanoids, eg prostaglandin E2: – PGE2 sensitizes nociceptors, thus lowering pain threshold and causing pain. NSAIDs raise the threshold therefore reduce perception of pain = ANALGESIC – PGE2 stimulates hypothalamic neurones to increase body temperature. Therefore blocking its production prevents this temp rise = ANTI-PYRETIC – PGE2 enhances Th1 differentiation (>IFN-gamma) + Th17 expansion (>IL-17) – both of these have pro-inflammatory effects therefore blocking = ANTIINFLAMMATORY – PGE2 downregulates gastric acid secretion + stimulates mucus/bicarbonate secretion. NSAIDs block this so remove cytoprotection + increase risk of GASTRIC ULCERATION Drug Ibuprofen Class Non-selective NSAID Pharmacodynamics (MOA) Reversibly inhibits COX 1 and COX 2 with equal affinity, thus preventing prostaglandin H2 synthesis Clinical Uses Anti-inflammatory Anti-pyretic Analgesic Pharmacokinetics Orally active Side Effects Gastric ulcers, decreased glomerular filtration rate, renal ischaemia, salt and water retention Drug Aspirin Class NSAID Pharmacodynamics (MOA) Irreversible COX 1 and COX 2 inhibitor, although selective for COX 1. High affinity for COX 1 reduces thromboxane A2 synthesis in platelets, thus preventing platelet aggregation. COX 2 action prevents PGI2 synthesis, which has inhibitory actions against platelet aggregation, but this effect is much less. Also same actions as other NSAIDs Clinical Uses Anti-platelet Anti-inflammatory, anti-pyretic, analgesic Pharmacokinetics Orally active Irreversible inhibitor therefore prolonged action; requires de novo COX synthesis Side Effects Gastric irritation + ulceration, bronchospasm (in sensitive asthmatics), prolonged bleeding and nephrotoxicity Drug Celecoxib Class COX-2 selective NSAID Pharmacodynamics (MOA) Selectively inhibits COX-2 Clinical Uses In patients with high risk of GI side effects Pharmacokinetics Orally active Side Effects Increase in CVS related side-effects Other relevant information less effect on COX-1 mediate processes > fewer risks of gastric ulceration Drug Paracetamol Class NOT an NSAID Pharmacodynamics (MOA) Not completely understood Clinical Uses Analgesic + anti-pyretic Pharmacokinetics Paracetamol is a phase I metabolite of a pro-drug (thus has free OH). Phase I metabolism of paracetamol > production of NAPQI (toxic), which then undergoes glutathione conjugation (involves glutathione transferase Other phase II metabolism pathways that can occur include methylation, sulphation or glucuronidation Side Effects NAPQI toxicity treated with cysteine – forces NAPQI to undergo Phase II metabolism Contraindications Hepatic impairment 5.Drugs and the GI Tract Anti-Emetics • These should only be administered when the cause of the nausea/vomiting is know, otherwise could mask the diagnosis of a potentially serious condition Vomiting Pathways Drug Promethazine Class Anti-emetic (H1 antagonist) Pharmacodynamics (MOA) Histaminergic antagonist: Competitive antagonist at H1, AchM and D2 receptors, therefore acting centrally (NST, vestibular nuclei, higher centres, CTZ) to block the activation of the vomiting centre Clinical Uses Motion sickness, Meniere’s (disorder of Labyrinth), hyperemesis gravidarium, pre-/post-operatively Also relief of allergic symptoms, anaphylaxis, insomnia Pharmacokinetics Oral administration Onset of action 1-2 hours, peaks at 4 hours Duration of action 24 hours Side Effects Dizziness, tinnitus, fatigue, sedation, convulsions, antimuscarinic side effects (dry mouth etc) Other relevant information Potency of antagonistic action H1 > AchM > D2 Drug Metoclopramide Class Anti-emetic (D2 antagonist) Pharmacodynamics (MOA) Dopaminergic antagonist: competitive antagonist of D2, H1 and AchM receptors acting in the chemoreceptor trigger zone, as well as in the GIT to increase smooth muscle motility + accelerate intestinal transit Clinical Uses Renal failure, radiation sickness, GI disorders, cancer chemotherapy Pharmacokinetics Oral or IV administration Extensive first pass metabolism Crosses BBB and placenta Side Effects Drowsiness, dizziness, anxiety, extrapyramidal reactions (Parkisonian-like syndrome), hyperprolactinaemia, galactorrhea, disorders of menstration Other relevant information Causes faster transit time through GIT, therefore may affect boavailability of co-administered drugs, and comprimise nutrient supply Drug Hyoscine Class Anti-emetic (AchM antagonist) Pharmacodynamics (MOA) Muscarinic cholinoceptor antagonist; acts centrally to block the activation of the vomiting centre (AChM > D2 = H1) Clinical Uses PREVENTION of motion sickness Pre-operative Pharmacokinetics Oral, IV or transdermal administration Peak of action 1-2 hours Side Effects Drowsiness, dry mouth, mydriasis, cyclopegia (loss of vision accomodation), constipation Other relevant information Little effect once nausea/vomiting has been established Drug Ondasetron Class Anti-emetic (5HT3 antagonist) Pharmacodynamics (MOA) 5HT3 receptor antagonist; acts to block transmission via the visceral afferents to the chemoreceptor trigger zone and thus prevents activation of the vomiting centre Clinical Uses Preventing anti-cancer drug-induced vomiting Radiotherapy-induced sickness Post-operative nausea and vomiting Pharmacokinetics Oral administration Excreted in urine Side Effects Headache, flushing, constipation Anti-Ulcer Drugs • Peptic ulcer disease results from the imbalance of the protective and potentially damaging factors of the mucosal barrier. • Almost 100% of patients with peptic ulcer disease are infected with H. Pylori • Triple Therapy is currently the best practice in treating peptic ulcer disease: – Antibiotic – eg Metronidazole, Amoxicillin or Clarithromycin – Inhibitor of Gastric Secretion – PPI (eg omeprazole), or H2 receptor antagonist (eg cimetidine, ranitidine) – Cytoprotective drug – eg Sucralfate, bismuth chelate, misoprostal Drug Metronidazole Class Antibiotic Pharmacodynamics (MOA) Active against anaerobic bacteria and protozoa Drug Amoxicillin Class Antibiotic Pharmacodynamics (MOA) Broad spectrum antibiotic Drug Clarithromycin Class Antibiotic Pharmacodynamics (MOA) Macrolide structured antibiotic which inhibits the translocation of bacterial tRNA Drug Omeprazole Class Proton Pump Inhibitor Pharmacodynamics (MOA) Inhibitors of gastric secretion. Irreversibly inhibit the H/K ATPase responsible for H+ secretion into the canaliculi. Clinical Uses Component of triply therapy Peptic ulcers resistant to H2 antagonists Reflux oesophagitis Pharmacokinetics Orally active Administered as enteric-coated slow-release formulation Duration 2-3 days Side Effects Uncommon; headaches, mental confusion, impotence, gynaecomastia, pain in muscles and joints Other relevant information Inactive at neutral pH. In acid environment of the stomach, are protonated and rearranged into their active form. Inhibit secretion by >90% Drug Cimetidine Class Histamine Type 2 Receptor Antagonist Pharmacodynamics (MOA) Competitive antagonists at H2 receptors on parietal cells; prevent histamine binding > less acid secretion, but also reduce effect of Ach/Gastrin binding Clinical Uses Duodenal ulcer treatment Pharmacokinetics Orally active Duration of action 2-3 days Side Effects Uncommon; diarrhoea, dizziness, muscle pains, transient rashes, hypergastrinaemia Contraindications Withdrawal often results in relapses Other relevant information Reduces secretion by 60% Drug Ranitidine Class Histamine Type 2 Receptor Antagonist Pharmacodynamics (MOA) Competitive antagonists at H2 receptors on parietal cells; prevent histamine binding > less acid secretion, but also reduce effect of Ach/Gastrin binding Clinical Uses Duodenal ulcer treatment Pharmacokinetics Orally active Duration of action 2-3 days Side Effects Uncommon; diarrhoea, dizziness, muscle pains, transient rashes, hypergastrinaemia Contraindications Withdrawal often results in relapses Other relevant information Reduces secretion by 60% Drug Sucralfate Class Cytoprotective Drug Pharmacodynamics (MOA) Polymer containing aluminium hydroxide and sucrose octasulphate; acquires strong negative charge in acidic environment, binds to positively charge compounds (eg glycoproteins) to form gel-like complexes which coat the ulcer, limiting H= diffusion and pepsin degradation Clinical Uses Peptic ulcers Component of triple therapy Pharmacokinetics Orally active Duration of action 3 hours Side Effects Constipation, dry mouth, nausea, vomiting, headaches Other relevant information Reduces absorption of other drugs, eg digoxin. Important to consider therapeutic window + bioavailability Drug Bismuth chelate Class Cytoprotective drug Pharmacodynamics (MOA) Toxic effects on H. pylori, prevents its adherence to mucosa + inhibits its proteolytic enzymes. Enhances local prostaglandin synthesis to stimulate bicarbonate secretion Clinical Uses Resistant cases of triple therapy Pharmacokinetics Orally active Side Effects Nausea and vomiting, blackening of tongue and faeces Drug Misoprotol Class Cytoprotective drug Pharmacodynamics (MOA) Stable prostaglandin analogue; mimics action of locally produced prostaglandins to maintain the gastroduodenal mucosal barrier: Inhibits acid secretion via G-protein coupled receptor mediated inhibition of adenylate cyclase Stimulates increased secretion of protective mucus Increased mucosal blood flow Clinical Uses Prevention of NSAID induced gastric ulcers Side Effects Diarrhoea, abdominal cramps, uterine contractions Contraindications Pregnancy – induces premature labour (use in abortion) Drugs and Inflammatory Bowel Disease Characteristic Ulcerative Colitis Crohn’s Disease Autoimmune disease Th2 mediated Th1 mediated T cell expansion/apoptosis Normal Florid expansion + defective apoptosis Gut layers affected Mucosa + submucosa All layers Regions of the gut affected Colon Any region Inflammation Continuous Patchy Fistulae/fissures/abscesses Not present Present Surgery Curative Not always curative Treatment falls into 2 parts: the treatment of active disease and the maintenance of remission. These then are put into 3 categories: • Supportive therapies – acute treatment + nutrition-based therapies to maintain remission • Treatment to reduce inflammation + relief of symptoms – glucocorticoids, aminosalicylates, immunosuppressives • Curative therapies – anti-TNFalpha antibodies Drug Mesalazine Class Aminosalicylate Pharmacodynamics (MOA) Anti-inflammatory action: reduces free radicals, upregulates endogenous anti-oxidants, reduces leukocyte infiltration Clinical Uses Treatment of ulcerative colitis + maintenance of remission Pharmacokinetics Oral administration (pH dependent capsules) Absorbed in small bowel and colon Side Effects Nausea, diarrhoea, abdominal pain/cramps, urticaria Other relevant information No immuno-supressive action Innefective in Crohn’s Drug Sulfasalazine Class Aminosalicylate Pharmacodynamics (MOA) Anti-inflammatory action: reduces free radicals, upregulates endogenous anti-oxidants, reduces leukocyte infiltration Clinical Uses Treatment of ulcerative colitis + maintenance of remission Pharmacokinetics Oral administration (pH dependent capsules) Absorbed in colon Metabolised by colonic flora Side Effects Anorexia, nausea, agranulocytosis, hypospermia Other relevant information No immuno-supressive action Innefective in Crohn’s Drug Prednisolone Class Glucocorticoid Pharmacodynamics (MOA) Cortisol-derived agonist of glucocorticoid receptors. Then act as: • Anti-inflammatories – positive transcription factors for anti-inflammatory genes + negative transcription factors for pro-inflammatory factors • Immunosuppressives: reduce antigen presentation, cell proliferation and clonal expansion Clinical Uses Inducing remission in Crohn’s disease Pharmacokinetics Administered topically (oral if severe) Side Effects Related to effects of cortisol: osteoporosis, suppression of HPA axis, T2DM, hypertension, infection susceptibility, skin thinning, bruising, proximal myopathy, buffalo hump Other relevant information Strategies for minimising unwanted effects include use of tapered doses, use of drugs with high therapeutic index, topical administration Drug Fluticasone Class Glucocorticoid Pharmacodynamics (MOA) Cortisol-derived agonist of glucocorticoid receptors. Then act as: • Anti-inflammatories – positive transcription factors for anti-inflammatory genes + negative transcription factors for pro-inflammatory factors • Immunosuppressives: reduce antigen presentation, cell proliferation and clonal expansion Clinical Uses Inducing remission in Crohn’s disease Pharmacokinetics Administered topically (oral if severe) Side Effects Related to effects of cortisol: osteoporosis, suppression of HPA axis, T2DM, hypertension, infection susceptibility, skin thinning, bruising, proximal myopathy, buffalo hump Other relevant information Strategies for minimising unwanted effects include use of tapered doses, use of drugs with high therapeutic index, topical administrationn Drug Budesonide Class Glucocorticoid Pharmacodynamics (MOA) Cortisol-derived agonist of glucocorticoid receptors. Then act as: • Anti-inflammatories – positive transcription factors for anti-inflammatory genes + negative transcription factors for pro-inflammatory factors • Immunosuppressives: reduce antigen presentation, cell proliferation and clonal expansion Clinical Uses Inducing remission in Crohn’s disease Pharmacokinetics Administered topically (oral if severe) Side Effects Related to effects of cortisol: osteoporosis, suppression of HPA axis, T2DM, hypertension, infection susceptibility, skin thinning, bruising, proximal myopathy, buffalo hump Other relevant information Strategies for minimising unwanted effects include use of tapered doses, use of drugs with high therapeutic index, topical administratiopn Drug Azathioprine Class Immunosuppressive Pharmacodynamics (MOA) Pro-drug activated by gut flora to 6-mercaptopurine – this interferes with purine biosynthesis and hence dna synthesis/replication. Effects include: • Impaired acquired immune response, lymphocyte proliferation, mononuclear cell infiltration, antibody synthesis • Enhanced T cell apoptosis Clinical Uses Maintaining remission of UC Inducing + maintaining remission of CD Enabling reduction of glucocorticoid dose Pharmacokinetics Metabolised by xanthine oxidase Side Effects Bone marrow suppression Contraindications Co-administration with drugs that inhibit xanthine oxidase, eg allopurinol, as lead to build up of 6-mercaptopurine > blood disorders 6. Antimicrobials Antimicrobials • These should be toxic for the pathogenic cell but innocuous for the host. This selective toxicity depends on the existence of exploitable biochemical differences between the pathogen and host cell, which in turn depends on how far apart the cells are in terms of evolutionary development • These include: – – – – Anti-bacterial agents Anti-mycobacterial agents Anti-fungals Anti-virals Antibacterials • These exploit the differences between prokaryotic bacterial cells, and eukaryotic host cells. • Targets for antibacterial agents include: – Folate – Peptidoglycan – Ribosomes Drug Co-trimoxazole Class Combined folate synthesis inhibitor (sulphonamide) + folate antagonist (trimethoprim) = sequential blockade Pharmacodynamics (MOA) Sulphonamide – structural analogue of P-aminobenzoic acid (required for folate synthesis); competes for dihydropteroate enzyme therefore interfering with DNA/RNA synthesis – BACTERIOSTATIC Trimethoprim – folate antagonist that inhibits dihydrofolate enzyme action; interferes with use of folate for DNA/RNA synthesis Sulphonamides potentiate the action of trimethoprim Clinical Uses Pneumonia (AIDs patients) – infection with pneumocystis carinii Pharmacokinetics Oral administration Half excreted within 34 hours Side Effects Nausea/vomiting Skin rashes Hypersensitivity reactions Drug Penicillin Class Beta-lactam Antibiotic Pharmacodynamics (MOA) Beta lactam ring interferes with peptidoglycan synthesis,by inhibiting the transpeptidation enzyme that cross-links the peptide chains with the backbone of the peptidoglycan • preventing formation of bacterial cell wall > bacterial burst = BACTERIOCIDAL Pharmacokinetics Oral administration – depends on acidity of stomach (empty stomach) Widely bio-distributed; crosses placenta but lipid insoluble therefore doesn’t cross BBB Mainly renal excretion Side Effects Relatively free from toxic effects, but hypersensitivity reactions are common: • Skin rashes, fever • Anaphylaxis GI tract disturbances also common Other relevant information Resistance mechanisms: • Production of B-lactamases • Reduction in permeability of outer bacterium membrane • Occurrence of modified penicillin-binding sites Drug Cefotaxime Class Beta-lactam antibiotic (part of cephalosporin family) Pharmacodynamics (MOA) Interfere with peptidoglycan synthesis = BACTERIOCIDAL Clinical Uses Crosses BBB therefore first line treatment for bacterial meningitis Pharmacokinetics IV/IM administration Renal excretion Side Effects Hypersensitivity Nephrotoxicity Diarrhoea Contraindications 10% of people with penicillin hypersensitivity will be cefotaxime sensitive Other relevant information Resistance (wide-spread) • Gene encoding beta lactamase – more active in hydrolysing cephalosporins than penicillins • Decreased penetration of drug due to mutations in outer membrane proteins or binding site proteins Drug Tetracycline Class Antibiotic (inhibitor of ribosome function) Pharmacodynamics (MOA) Binds to + actively transported into bacteria to interrupt protein synthesis via competitive binding for A binding site on 502 subunit = BACTERIOSTATIC Clinical Uses Wide spread of bacterial infections (both gram +ve and –ve) Pharmacokinetics Absorption is irregular + incomplete – chelation of iron + calcium Wide bio-distribution Excretion by bile and glomerular filtration Side Effects GIT disturbances Chelated calcium deposits in growing bone > deformity Contraindications Children, pregnant women, nursing mothers Other relevant information Resistance mechanisms: • Development of energy dependent efflux mechanisms • Mutations of ribosome structure to prevent binding Drug Chloramphenicol Class Antibiotic (inhibitor of ribosome function) Pharmacodynamics (MOA) Binds to 50s subunit of ribosome, inhibiting transpeptidation and therefore protein synthesis = BACTERIOSTATIC Clinical Uses Wide spread (gram +ve and –ve infections) Pharmacokinetics Oral or parenteral administration Complete absorption Half life 2 hours Distribution includes CSF Excretiion: 10% unchanges in urine, 90% metabolised in liver and then excreted via kidneys + bile Side Effects Pancytopenia (decrease in all blood cells due to bone marrow suppression) Grey baby syndrome – vomiting, diarrhoea. Flaccidity, low temp, ash grey colour in newborns GI disturbances Other relevant information Resistance mechanism: R plasmid mediated transfer of chloramphenicol acetyl-transferase. Solution: replacing terminal OH on side-chain by fluorine reduces susceptibility to acetylation Drug Gentamicin Class Antibiotic (aminoglycoside) Pharmacodynamics (MOA) Binds to 30s subunit of bacteria > anticodon-codon misread > translation of defective protein = BACTERIOCIDAL Second mechanism unknown Clinical Uses Aerobic gram –ve infection Infection causes by streptococcus, listeria, pseudomonas aeruginosa (in conjunction with penicillin) Pharmacokinetics Highly polar – not absorbed in GIT therefore IV/IM adminstration Not widely distributed Half life 2-3 hours Elimination entirely by kidney Side Effects Ootoxicity (damage to sensory cells in cochlea and vestibular organ) Nephrotoxicity Contraindications Renal impairement Chloramphenicol (blocks oxygen-dependent active transport of gentamicin into bacterial cell) Other relevant information Resistance mechanisms: Inactivation by microbial enzymes Failure of penetration – overcome with penicillin Mutations – alter 30s binding site Anti-mycobacterial agents • Used to treat infections caused by mycobacterium tuberculosis and leprae – Main problem with infection is that micro-organisms can survive inside macrophages unless they are activated by T-cell lymphokines > latent infection • 6 month drug combination therapy is used to manage high incidence of drug resistance (6 month treatment minimum – poor compliance) – 1st phase = 2 months (isoniazid, rifampicin + pyrazinamide) – 2nd phase = 4 months (isoniazid + rifampicin) Drug Isoniazid Class Anti-mycobacterial Pharmacodynamics (MOA) Bacteriostatic on resting mycobacteria Bacteriocidal on dividing mycobacteria (extracellular and intracellular) MOA not fully understood – inhibition of cell wall synthesis? Clinical Uses TB + leprosy Pharmacokinetics Oral administration Readily absorbed from GIT Widely distributed (CSF) Metabolism = acetylation. Other relevant information Therapeutic response dependent on whether patient is fast or slow acetylator (slow = better because slower metabolism) Drug Rifampicin Class Anti-mycobacterial agent Pharmacodynamics (MOA) Inhibits prokaryotic DNA-dependent RNA-polymerase = BACTERIOCIDAL Effective for both extracellular and intracellular organisms Clinical Uses TB + leprosy Pharmacokinetics Oral administration Widely distributed Excreted in bile + urine – undergoes enteroheptic recycling Progressive metabolism: deacetylation – metabolite less well absorbed Side Effects Infrequent – skin rashes, fever, GIT disturbances Drug Pyrazinamide Class Anti-mycobacterial Pharmacodynamics (MOA) tuberculoSTATIC at acidic pH, like that of the macrophage environment. Therefore effective against the intracellular organism in macrophage Clinical Uses TB Pharmacokinetics Oral administration Good absorption Widely distributed (inc meninges) Excretion via glomerular filtration Side Effects Arthralgia, GIT disturbance, malaise + fever Anti-fungals • Fungal infections are termed mycoses; these may be systemic (rare) or superficial (more common) • Superficial mycoses may be dermatomycoses (commonly tinea infections) or candidiasis (yeast infections of mucous membranes) Drug Nystatin Class Anti-fungal Pharmacodynamics (MOA) Polyene macrolide that binds to ergosterol (within cell membrane), forming a transmembrane ion channel that disrupts permeability and transport function Clinical Uses Fungal infections of skin + GI tract Pharmacokinetics No absorption through mucous membranes Side Effects Rare; nausea and vomiting Very rare; rash Drug Miconazole Class Anti-fungal Pharmacodynamics (MOA) Azole group of synthetic anti-mycotic agent that blocks the synthesis of ergosterol, altering the fluidity of fungal membrane and interfering with the action of membraneassociated enzymes – results in inhibition of replication Clinical Uses Wide spectrum of systemic and superficial infection Pharmacokinetics IV administration for systemic Oral administration for superficial Short plasma half life Side Effects Infrequent; GIT disturbance Rare; blood dyscrasias Anti-Virals • Viruses: small intracellular parasites consisting of nucleic acids (RNA or DNA) enclosed by a protein coat/capsid • Obligate intracellular parasites therefore use host cell machinery for replication; poses challenge for selective drugs – Virus-specific enzymes potential targets • Difficulty is that clinically detectable infection is usually far advanced so treatment difficult Drug Acyclovir Class Anti-viral Pharmacodynamics (MOA) Guanosine derivative that is converted to monophosphate form by thimidine kinase (viral thymidine kinase much more effective at doing this). Host cell kinases then convert monophosphate form to triphosphate form, and this then inhibits DNA viral-polymerase, terminating chain reaction and thus inhibiting nucleic acid synthesis Clinical Uses HSV infection Pharmacokinetics Oral (20% absorbed) or IV Widely distributed; crosses BBB Rapidly broken down within host cells by cellular phosphatases (need frequent application) Excreted by kidneys Side Effects Rare with oral administration, more common in intravenous administration: Local inflammation, renal dysfunction, nausea, headache Other relevant information Resistance occurs due to changes in viral genes coding for thymidine kinase or DNA polymerase Drug Zidovudine (AZT) Class Anti-RETROviral Pharmacodynamics (MOA) Analogue of thymidine (activated by cellular enzymes to triphosphate form) acts as competitive inhibitor of reverse transcriptase; incorporation into growing viral DNA strand results in chain termination preventing DNA synthesis Clinical Uses AIDS – reduces opportunistic infections, thrombocytopenia, dementia + viral load HIV+ve – prolongs life expectancy HIV+ve mothers – reduces chance of transmission to fetus Pharmacokinetics Oral administration Undergoes extensive first pass metabolism Widely distributed – enters cells by passive diffusion Metabolised by liver to inactive glucuronide 20% active form excreted in urine Side Effects Common = anaemia, neutropenia Rare = GIT disturbance, skin rash, insomnia, fever, headache Other relevant information Therapeutic response wanes with long term use – development of resistance: • Mutations in viral reverse transcriptase accumulate progressively • Decreased activation to triphosphate form 7. Cytotoxics Cytotoxics • Definition: “drugs that modify the growth of cells and tissues” • Challenges with cytotoxics: It is difficult to find exploitable differences, they need to produce a near total cell kill, have no effect on resting cells (which means relapse likely) • Cytotoxics tend to be antiproliferative, with no effect on tendency to metastasize or invade – effect on rapidly dividing normal tissues therefore result in multiple adverse effects Drug Cyclophosphamide Class Alkylating agent (interferes with DNA transcription/replication) Pharmacodynamics (MOA) Ethylene immonium derivative – substrate for cytochrome P450, when oxidised becomes extremely reactive and carbonium ion binds irreversibly with cell macromolecules including RNA, proteins and DNA, causing intra/inter chain cross-linking • This interferes with transcription and replication • Most common targets N7 guanine, N1/N3 adenosine Clinical Uses Cancer treatment Immunosuppession following allogenic tissue transplantation (at low dose) Pharmacokinetics Rapidly metabolised, but metabolites also have cytotoxic action Side Effects Myelotoxicity - damage bone marrow lead to reduced lekukocyte production. Impaired wound healing. Depression of growth. Sterility (because gonadal tissues are highly active). Teratogenicity - cross placenta. Loss of hair. Nausea and vomitting. GI tract epithelia, hair and nails Drug Methotrexate Class Antimetabolite (interferes with DNA base synthesis) Pharmacodynamics (MOA) Interferes with thymidylate synthesis (folate synthesis), thus preventing purine (adenine + guanine) synthesis > interfering with DNA synthesis Clinical Uses Cancer treatment Immunosuppression following allogenic tissue transplant (at low doses) Side Effects Myelotoxicity - damage bone marrow lead to reduced lekukocyte production. Impaired wound healing. Depression of growth. Sterility (because gonadal tissues are highly active). Teratogenicity - cross placenta. Loss of hair. Nausea and vomitting. GI tract epithelia, hair and nails Drug Doxorubicin Class Cytotoxic antibody (inhibits DNA/RNA chain synthesis) Pharmacodynamics (MOA) Antibody complexes with DNA, preventing the topoisomerase from “zipping up” DNA therefore inhibiting DNA and RNA synthesis Clinical Uses Cancer treatment Side Effects Myelotoxicity - damage bone marrow lead to reduced lekukocyte production. Impaired wound healing. Depression of growth. Sterility (because gonadal tissues are highly active). Teratogenicity - cross placenta. Loss of hair. Nausea and vomitting. GI tract epithelia, hair and nails Drug Bleomycins Class Cytotoxic antibody Pharmacodynamics (MOA) Metal-chelating glycopeptide antibody that degrades DNA Clinical Uses Cancer treatment Pharmacokinetics Administered intravenously Side Effects Myelotoxicity - damage bone marrow lead to reduced lekukocyte production. Impaired wound healing. Depression of growth. Sterility (because gonadal tissues are highly active). Teratogenicity - cross placenta. Loss of hair. Nausea and vomitting. GI tract epithelia, hair and nails Other relevant information Active against non-dividing cells, therefore very toxic and high chance of pulmonary toxicity Drug Etoposide Class Plant alkaloid Pharmacodynamics (MOA) Inhibition of topoisomerase II inhibits DNA synthesis > cell cycle block at G2 phase Clinical Uses Cancer treatment Side Effects Myelotoxicity - damage bone marrow lead to reduced lekukocyte production. Impaired wound healing. Depression of growth. Sterility (because gonadal tissues are highly active). Teratogenicity - cross placenta. Loss of hair. Nausea and vomitting. GI tract epithelia, hair and nails Drug Vincristine Class Plant alkaloid (spindle cell poison) Pharmacodynamics (MOA) Binds to tubulin, inhibiting its polymerisation to form microtubules necessary for spindle formation. This therefore prevents cell division and thus successful replication Clinical Uses Cancer treatment Side Effects Myelotoxicity - damage bone marrow lead to reduced lekukocyte production. Impaired wound healing. Depression of growth. Sterility (because gonadal tissues are highly active). Teratogenicity - cross placenta. Loss of hair. Nausea and vomitting. GI tract epithelia, hair and nails Drug Cisplatin Class Miscellaneous cytotoxic Pharmacodynamics (MOA) Interacts directly with DNA causing guanine intrastrand cross-linking > interference with transcription and replication Clinical Uses Cancer treatment Side Effects Myelotoxicity - damage bone marrow lead to reduced lekukocyte production. Impaired wound healing. Depression of growth. Sterility (because gonadal tissues are highly active). Teratogenicity - cross placenta. Loss of hair. Nausea and vomitting. GI tract epithelia, hair and nails Drug Procarbazine Class Miscellaneous cytotoxic Pharmacodynamics (MOA) Alkylates DNA, interfering with DNA/RNA synthesis and mitosis at interphase Clinical Uses Cancer treatment Side Effects Myelotoxicity - damage bone marrow lead to reduced lekukocyte production. Impaired wound healing. Depression of growth. Sterility (because gonadal tissues are highly active). Teratogenicity - cross placenta. Loss of hair. Nausea and vomitting. GI tract epithelia, hair and nails Other relevant information Activated by cytochrome P450 and MAO 8. Drugs of Abuse Drugs of Abuse • MOA: artificially hijack the natural reward pathway; DA release from ventral tegmental area into the nucleus accumbens > euphoria • Classification of drugs: – Narcotics (painkillers) are opiate like drugs, eg heroin and morphine • Opitaes bind to u opiate receptors on the GABAergic neuron cell body to suppress them, therefore suppressing GABA release > more dopamine release – Depressants are ‘downers’, which slow down the CNS. These include alcohol, benzodiazepines (valium), and barbiturates – Stimulants are ‘uppers’, and are probably the largest class of addictive drugs, which tend to speed everything up in the CNS, eg cocaine + nicotine – Miscellaneous drugs have several effects and properties (e.g. stimulant as well as hallucinogenic), and these drugs include cannabis and ecstasy (MDMA). Drug Cannabis Class Miscellaneous drug of abuse Origin Genus of flowering plant. > 60 Cannabinoids (active component) found in all parts of the plant, eg tetrahydrocannabinol (THC – most potent). • Marijuana = crushes dried leaves • Resin/Hashish = cannabinoid secreted from glandular trichomes • Hash oil = solvent extracted hashish (concentrated) Pharmacodynamics (MOA) Analogue of endogenous cannabinoid (eg anadamide – generated from arachidonic acid), which binds to endogenous CB1 receptors in brain and CB2 receptors on WBC. Binding > downregulation of adenylyl cyclase > inhibition of GABA secretion > increased DA secretion Clinical Uses In disease: upregulating CB receptors used to mitigate disease eg MS, as well as having an effect on fertility, obesity In pharmacology: targeting the cannabinoid system can be used to increase appetite in AIDs patients, decrease appetite in obese patients and treat neuropathic pain in MS Pharmacokinetics Administration: • Smoking > 50% absorption but rapid onset of action • Eating > 10% absorption (first pass metabolism), delayed onset of action but prolonged effect Duration of action is dependent on adipose tissue. Cannabis is very lipid soluble, therefore sits in fat cells for long periods of time before returning to the circulation (unusual) Hepatic metabolism 25% excreted unmetabolised, 65% undergoes enterohepatic recycling. Metabolism forms 11hydroxyTHC = active metabolite > increased intoxication Side Effects Psychosis + schizophrenia (anterior cingulate cortex), munchies (hypothalamus), amnesia (limbic regions), effect on psychomotor performance (cerebral cortex), immunosuppressant (B2 receptors on WBC), reddening conjunctivae (vasodilation) Drug Cocaine Class Stimulant drug of abuse Origin Erythroxylum coca plant. Can extract up to 0.9% of drug from plant; different forms: • Paste • Cocaine HCl (paste dissolved in acid) • Crack cocaine (Cocaine HCl precipitated in alkaline solution) • Freebase cocaine (crack dissolved in ammonia) Pharmacodynamics (MOA) Binds to da transporter present on terminals of DA neurons and prevents reuptake, therefore prolonging DA effect > euphoria Pharmacokinetics Administration • Paste + cocaine HCl – IV, oral , intranasal • Crack + freebase – inhalation Onset of action: within seconds following smoking/injection Metabolised by liver + plasma cholinesterases Half life < 20 mins Side Effects Local anaesthesia – blocks Na+ channels, inhibits monoamine transporters (a2 adrenoceptors) Irratibility, anxiety, hostility – CNS stimulation Other relevant information Risk of sudden death: increased endothelin 1 (vasoconstriction), decreased NO production (increased platelet activation), increased SNS activation Drug Nicotine Class Plant-derived alkaloid Pharmacodynamics (MOA) Acts on nicotinic acetylcholine receptors (especially alpha 4 and beta 2 subunits) on the cell bodies of dopaminergic neurones > DA release into nucleus accumbens > euphoria Clinical Uses Suggestive protection against Parkinson’s and Alzheimer’s Pharmacokinetics Administration • Intranasal spray – 20-50% absorbed • Gum – 50-70% absorbed (slow onset) • Cigarettes – 20% absorbed (rapid onset) • Transdermal patch – 70% absorbed Spray, gum + patch aim to remove spike which encourages addiction Pka of 7.9. smoke is relatively acidic therefore is ionised; spray, gum and patch aim to buffer to maximise absorption Half life – hours Hepatic metabolism by cytochrome P2A6 and cotidine Renal excretion Side Effects CVS effects (due to Ach agonistic action) • Increased HR, SV, coronary vasoconstriction, skeletal vasodilation, increased platelet activity (increased ThA2 + decreased NO) Metabolic effects: increase BMR, appetite suppressant Drug Alcohol See lecture 15 (too much detail for slide) Disulfram Alcohol dehydrogenase inhibitor = Ethanol aversion drug; leads to build up of toxic metabolite acetylaldehyde which leads to horrible feeling when drinking 9. Opiates + Opioids Pain Pathway • Ascending pathways - perception of pain • Descending inhibitory pathways – pain tolerance – – – – PAG = peri-aqeductal grey area (midbrain) NRM = nucleus raphe magnus (medulla) NRPG = nucleus reticularis paragigantocellularis LC = locus coeruleus (brainstem) Drug Morphine Class Opiate Structure Natural opiate; alkaloid derivative of papaver somniferum poppy (tertiary amine with hydoxyl groups at positions 3 and 6) Pharmacodynam ics (MOA) Act via endogenous opioid receptors (endogenous opioid peptides inc endorphins, enkephalins and neoendorphins). Binding to u, d or k G-protein linked receptors > decreased adenylate cyclase > decreased cAMP > increased capacity for K+ efflux + decreased Ca2+ influx > decreased action potential generation = DEPRESSANT • Analgesia: huge concentration of receptors in SC – depress afferent pathways > reduced perception + activate descending inhibitory pathway > increased tolerance • Euphoria: Suppress GABA release from mesolimbic dopamine neurones into nucleus accumbens > increased DA • Antitussive: inhibit seratonin receptor activation in cough centre + suppress release of Ach and neurokinins in airways Clinical Uses Analgesic Antitussive (usually codeine) Pharmacokinetic s Oral administration (40-50% bioavailability) or IV administration Metabolised in liver > morphine-6-glucuronide. Then either excreted by kidney or active metabolite secreted in bile to undergo enterohepatic recycling Complex pharmacokinetics as largely ionized at physiological pH Side Effects SHORT TERM: • Respiratory depression: desensitizes chemoreceptors > loss of response to arterial CO2 + medullary action to control resp (main COD in overdose) • Nausea/vomiting: depresses natural inhibition of chemoreceptor trigger zone > activation of vomiting centre • Miosis: stimulation of occulomotor nerve > ciliary ganglion > iris > constriction (unconscious + pinprick pupils = heroin overdose) • Constipation: depress gastric emptying and GI motility > increased water absorption • Allergy: G-protein mediated activation of mast cells > histamine release > pruritus (itching), urticaria, hypotension LONG TERM: • Tolerance: increased arrestin production > receptor internalisation > decreased response • dependence: withdrawal > upregulation of adenylate cyclase system > craving, tremor, diarhoea Other relevant information Treatment for overdose is opioid receptor antagonist NALOXONE (iv administration) Drug Codeine Class Opiate Structure Natural opiate (methyl-morphine) – tertiary amine with methyl group at position 3 Pharmacodynami cs (MOA) Act via endogenous opioid receptors (endogenous opioid peptides inc endorphins, enkephalins and neoendorphins). Binding to u, d or k G-protein linked receptors > decreased adenylate cyclase > decreased cAMP > increased capacity for K+ efflux + decreased Ca2+ influx > decreased action potential generation = DEPRESSANT • Analgesia: huge concentration of receptors in SC – depress afferent pathways > reduced perception + activate descending inhibitory pathway > increased tolerance • Euphoria: Suppress GABA release from mesolimbic dopamine neurones into nucleus accumbens > increased DA • Antitussive: inhibit seratonin receptor activation in cough centre + suppress release of Ach and neurokinins in airways Clinical Uses Analgesic Antitussive Pharmacokinetics Oral administration (5-10% bioavailability) Side Effects SHORT TERM: • Respiratory depression: desensitizes chemoreceptors > loss of response to arterial CO2 + medullary action to control resp (main COD in overdose) • Nausea/vomiting: depresses natural inhibition of chemoreceptor trigger zone > activation of vomiting centre • Miosis: stimulation of occulomotor nerve > ciliary ganglion > iris > constriction (unconscious + pinprick pupils = heroin overdose) • Constipation: depress gastric emptying and GI motility > increased water absorption • Allergy: G-protein mediated activation of mast cells > histamine release > pruritus (itching), urticaria, hypotension LONG TERM: • Tolerance: increased arrestin production > receptor internalisation > decreased response • dependence: withdrawal > upregulation of adenylate cyclase system > craving, tremor, diarhoea Other relevant information Treatment for overdose is opioid receptor antagonist NALOXONE (iv administration) Drug Heroin Class Opiate Structure Di-acetyl-morphine – acetylated > acetyl groups at position 3 and 6 > increased potency Pharmacodynamics (MOA) Act via endogenous opioid receptors (endogenous opioid peptides inc endorphins, enkephalins and neoendorphins). Binding to u, d or k G-protein linked receptors > decreased adenylate cyclase > decreased cAMP > increased capacity for K+ efflux + decreased Ca2+ influx > decreased action potential generation = DEPRESSANT • Analgesia: huge concentration of receptors in SC – depress afferent pathways > reduced perception + activate descending inhibitory pathway > increased tolerance • Euphoria: Suppress GABA release from mesolimbic dopamine neurones into nucleus accumbens > increased DA • Antitussive: inhibit seratonin receptor activation in cough centre + suppress release of Ach and neurokinins in airways Clinical Uses Analgesic Antitussive (usually codeine) Pharmacokinetics Intravenous administration Hepatic metabolism (like morphine) + plasma esterases > shorter half life > more addictive Side Effects SHORT TERM: • Respiratory depression: desensitizes chemoreceptors > loss of response to arterial CO2 + medullary action to control resp (main COD in overdose) • Nausea/vomiting: depresses natural inhibition of chemoreceptor trigger zone > activation of vomiting centre • Miosis: stimulation of occulomotor nerve > ciliary ganglion > iris > constriction (unconscious + pinprick pupils = heroin overdose) • Constipation: depress gastric emptying and GI motility > increased water absorption • Allergy: G-protein mediated activation of mast cells > histamine release > pruritus (itching), urticaria, hypotension LONG TERM: • Tolerance: increased arrestin production > receptor internalisation > decreased response • dependence: withdrawal > upregulation of adenylate cyclase system > craving, tremor, diarhoea Other relevant information Treatment for overdose is opioid receptor antagonist NALOXONE (iv administration) Drug Methadone Class Opiate Pharmacodynamics (MOA) Act via endogenous opioid receptors (endogenous opioid peptides inc endorphins, enkephalins and neoendorphins). Binding to u, d or k G-protein linked receptors > decreased adenylate cyclase > decreased cAMP > increased capacity for K+ efflux + decreased Ca2+ influx > decreased action potential generation = DEPRESSANT • Analgesia: huge concentration of receptors in SC – depress afferent pathways > reduced perception + activate descending inhibitory pathway > increased tolerance • Euphoria: Suppress GABA release from mesolimbic dopamine neurones into nucleus accumbens > increased DA • Antitussive: inhibit seratonin receptor activation in cough centre + suppress release of Ach and neurokinins in airways Clinical Uses Morphine/heroin replacement to wean off addicts Analgesic Antitussive (usually codeine) Pharmacokinetics Lipid-soluble + efficient distribution Long half-life, therefore low dose for long time Side Effects SHORT TERM: • Respiratory depression: desensitizes chemoreceptors > loss of response to arterial CO2 + medullary action to control resp (main COD in overdose) • Nausea/vomiting: depresses natural inhibition of chemoreceptor trigger zone > activation of vomiting centre • Miosis: stimulation of occulomotor nerve > ciliary ganglion > iris > constriction (unconscious + pinprick pupils = heroin overdose) • Constipation: depress gastric emptying and GI motility > increased water absorption • Allergy: G-protein mediated activation of mast cells > histamine release > pruritus (itching), urticaria, hypotension LONG TERM: • Tolerance: increased arrestin production > receptor internalisation > decreased response • dependence: withdrawal > upregulation of adenylate cyclase system > craving, tremor, diarhoea Other relevant information Treatment for overdose is opioid receptor antagonist NALOXONE (iv administration) 10. Drugs and the CNS Anxiolytics, Sedatives + Hypnotics • These drugs all affect GABA transmission (principal inhibitory NT of the CNS), and tend to act on the GABAA receptor complex • GABA-A complex consists of Cl-, GABA, BDZ + BARB receptor proteins • GABA binds to receptor, activating GABA modulin (link between GABA + BDZ protein) > opening of Cl- channel • Anxiolytics remove anxiety WITHOUT impairing mental or physical activity • Sedatives reduce mental and physical activity WITHOUT producing loss of consciousness • Hypnotics induce sleep Drug Amobarbitol Class Barbituate Structure Classic 6-membered ring with number of additional groups Pharmacodynamics (MOA) BARBs bind to their own receptor; enhance GABA action + binding (not reciprocated by GABA) + direct effect on Cl- channel > increased DURATION of Cl- ion channel opening BARBs also appear to act as non-selective glutamate antagonists > decreased excitatory transmission (use for induction of anaesthesia) Clinical Uses Sedative, hypnotic Side Effects Depress respiration, “hangovers” (alter natural sleep + REM), tolerance (severe; pharmacokinetic + tissue tolerance), dependence/withdrawal (insomnia, anxiety, tremors) Contraindications Interact with co-administered drugs, as are enzyme inducers Potentiate other CNS depressants eg alcohol Benzodiazepine ure 3 ring structure; lots of variations > large changes in pharmacokinetic activity acodynamics BDZ bind to their own receptor; enhance GABA action + GABA binding (reciprocrat GABA) > increased FREQUENCY of Cl- ion channel opening Uses Anxiolytic acokinetics Oral administration Peak plasma within hour Bind pp and highly lipid soluble – well distributed Hepatic metabolism (glucuronidation) Renal excretion Duration of action = long acting (t ½ = 32 hours); metabolism via active metabolite fects Sedation, confusion, ataxia Tolerance (< than BARBs; only tissue) Dependence + withdrawal Increase in free plasma concentrations of other drugs eg aspirin indications Potentiates other CNS depressants eg alcohol dynamics ses Benzodiazepine 3 ring structure; lots of variations > large changes in pharmacokinetic activity BDZ bind to their own receptor; enhance GABA action + GABA binding (reciprocrated b increased FREQUENCY of Cl- ion channel opening Sedative Hypnotic Anxiolytic (in hepatic impairment as alternative to diazepam) kinetics Oral administration (IV for status epilepticus) Peak plasma within hour Bind pp and highly lipid soluble – well distributed Hepatic metabolism (glucuronidation) Renal excretion Duration of action = short acting (t ½ = 8 hrs) ts Sedation, confusion, ataxia Tolerance (< than BARBs; only tissue) Dependence + withdrawal Increase in free plasma concentrations of other drugs eg aspirin ications Potentiates other CNS depressants eg alcohol e 3 ring structure; lots of variations > large changes in pharmacokinetic activity codynamics BDZ bind to their own receptor; enhance GABA action + GABA binding (reciprocrated increased FREQUENCY of Cl- ion channel opening Uses Sedative Hypnotic cokinetics Oral administration (IV for status epilepticus) Peak plasma within hour Bind pp and highly lipid soluble – well distributed Hepatic metabolism (glucuronidation) Renal excretion Duration of action = short acting (t ½ = 8 hrs) ects Sedation, confusion, ataxia Tolerance (< than BARBs; only tissue) Dependence + withdrawal Increase in free plasma concentrations of other drugs eg aspirin ndications Potentiates other CNS depressants eg alcohol levant Advantages over BARBs: Drug Chloral Hydrate Pharmacodynamics (MOA) not known Clinical Uses Sedative/hypnotic in children/elderly (wide margin of safety) Pharmacokinetics Metabolised in liver to trichloroethanol = active component Drug Busipirone Class 5HT-1A agonist Pharmacodynamics (MOA) Interacts with seratonin transmission (not fully understood) Clinical Uses Anxiolytic Pharmacokinetics Slow onset of action Side Effects Few Anti-convulsants • Epilepsy: the tendency to recurrent, unprovoked seizures – Cause: symptomatic (structural/metabolic brain injury – either acquired or inherited) or idiopathic (either mendelian or polygenic) – Classification: focal or generalised (tonic-clonic or absence) • AED act by 3 mechanisms: – Enhancing GABA mediated transmission – Inhibiting fast excitatory NT transmission – glutamate – Inhibiting neuronal AP generation – blocking NA voltage channels Phenytoin Anti-convulsant dynamics Blockade of voltage-dated Na+ channels > reduced AP generation es Partial epilepsy Status epilepticus (prolonged seizure) kinetics Hepatic metabolism: oxidation, hydroxylation then conjugation (large variation) Renal excretion Saturable kinetics; dosing very important Elimination t ½ 20 hours – monitoring requires at least 5 half lives Highly pp bound s Allergy: rash, vasculitis, fever, hepatitis Toxic: ataxia, sedation Chronic: folate deficiency, Vit K deficiency, peripheral neuropathy, myopathy vant n P450 enzyme inducer, therefore large number of drug interactions • Amiodarone + isoniazid – inhibit metabolism • Aspirin – disaplaces from PP • Valproate – displaces + inhibits • Cyp450 > reduced warfarin, estrogen containing OCP Drug Carbazepine Class Anti-convulsant Pharmacodynamics (MOA) Blockade of Na+ voltage-gated channels Clinical Uses Partial seizures Secondary generalized seizures Pharmacokinetics Half-life 5-26 hours Hepatic metabolism: oxidation then conjugation. Active metabolite = carbazepine epoxide Side Effects Hypersensitivity: rash, hepatitis, nephritis Dose-related: ataxia, dizziness, sedation Chronic: Vit K deficiency, depression Other relevant information Potent hepatic enzyme inducer Complex drug interaction profile Drug monitoring useful Drug Sodium valproate lass Anti-convulsant harmacodynamics MOA) Mechanism not known, but enhances GABA via number of mechanisms linical Uses Partial seizures Generalised seizures harmacokinetics Half life 4-12 hours Metabolism by hepatic oxidation and conjugation – no active metabolites Renal excretion ide Effects Severe adverse drug reactions: Severe hepatic toxicity, pancreatitis, encephalopathy, tremor, blood dyscrasias ontraindications Co-administration with penytoin, phenobarbitol + carbazemazepine Other relevant nformation Potent inhibitor of hepatic enzymes > important drug reactions Drug Vigabatrin Class Anti-convulsant Pharmacodynamics (MOA) Irreversible inhibition of GABA transferase (involved in metabolism of GABA to SCA) Clinical Uses Partial epilepsy Pharmacokinetics Half life 7 hours Side Effects Visual field constriction Other relevant information May worsen some generalized seizures Drug Lamotrigine Class Anticonvulsant Pharmacodynamics (MOA) Unknown Clinical Uses Partial epilepsy Generalised epilepsy Pharmacokinetics Half life 8 hours Side Effects Well tolerated Anti-Parkinsonians + Neuroleptics • Parkinson’s affects the Nigrostriatal dopaminergic pathway (projected from substantia nigra to striatum) – involved in control of movement – Neuropathology: nigrostriatal pathway degeneration, accumulation of Lewy-Bodies (containing toxic proteins), cell loss > 85% dopaminergic neuron loss + 70% striatal DA depletion • Schizophrenia affects the Mesolimbic dopaminergic pathway (projected from ventral tegmental area to nucleus accumbens etc) – involved in emotion – Neuropathology: excessive dopamine transmission through mesolimbic region (DA action on D2 receptors) > positive symptoms (delusions, hallucinations, etc), and dopamine deficit in pre-frontal regions (D1 mediated) > negative symptoms (withdrawal, flattening of emotional responses) Drug L-DOPA Class Anti-parkinsonian Pharmacodynamics (MOA) Dopamine replacement therapy. DOPA doesn’t cross BBB, but L-DOPA can cross BBB and be centrally converted to DOPA. This occurs if peripheral conversion of L-DOPA to DOPA does not occur (involving DOPA-decarboxylase) Clinical Uses Hypokinesea, rigidity + tremor associated with Parkinson’s Pharmacokinetics Start with low dose; response decreases with disease progression Side Effects Acute: • Nausea (prevents by Domperidone) • Hypotension • Psychological (schizophrenia-like effects) Chronic: • Diskinesias • Rapid fluctuations in clinical state Drug Domperidone Class Anti-parkinsonian drug Pharmacodynamics (MOA) DOPA-decarboxylase antagonist– inhibits peripheral conversion of L-DOPA > DOPA, therefore increasing quantity of L-DOPA crossing BBB Clinical Uses Administered with L-DOPA; allowing lower dose of L-DOPA to be used, and boosting its effect Side Effects Chronic: • Diskinesias • Rapid fluctuations in clinical state Drug Carbidopa Class Anti-parkinsonian drug Pharmacodynamics (MOA) Inhibits DOPA-decarboxylase action in periphery, so more LDOPA reaches the CNS Clinical Uses Treatment of bradykinesias, tremors and rigidity associated with Parkinsons Pharmacokinetics Administered in conjunction with L-DOPA Side Effects Chronic: • Diskinesias • Rapid fluctuations in clinical state Drug Bromocriptine Class Anti-parksinonian drug Pharmacodynamics (MOA) DA (esp D2) receptor agonist Clinical Uses Used in conjunction with L-DOPA (to treat bradykinesias etc) when L-DOPA becoming less effective Pharmacokinetics Oral administration Crosses BBB Longer duration of action than L-DOPA, therefore less diskinesias Side Effects Common – confusion, dizziness, nausea/vomiting, hallucinations Rare – constipation, headache, dyskinesias Contraindications Ergot ring structure can cause problems with heart valves Drug Deprenyl Class Anti-parkinsonian drug Pharmacodynamics (MOA) Selective MAO-B inhibitor; prevents central breakdown of DA, therefore prolonging action Clinical Uses Preservation of naturally synthesised DA in early Parkinson’s Administration in conjunction with L-DOPA to reduce dose Pharmacokinetics Side Effects Rare – hypotension, nausea/vomiting, confusion, agitation Drug Entacapone Class Anti-parkinsonian drug Pharmacodynamics (MOA) COMT inhibitor; prevents peripheral conversion of L-DOPA to 3-0methylDOPA, thus increasing the bioavailability of L-DOPA Clinical Uses To reduce L-DOPA dosage To boost response to L-DOPA in patients starting to show tolerance Side Effects Marked side effect profile – CVS effects Drug Chlorpromazine Class Neuroleptic Pharmacodynamics (MOA) Dopamine receptor antagonists (particular D2 + D4) > reduce dopamine transmission through mesolimbic region > reduction in positive symptoms Clinical Uses Treatment of schizophrenia Pharmacokinetics Initially compensatory mechanisms to increase DA synthesis, but these decline with therefore slow onset of action Side Effects Effects due to non-selectivity of antagonists: Blocking receptors in chemotactic trigger zone > anti-emetic Blocking of DA in tuberoinfundular pathway (endocrine) > excess prolactin > lactation Blockade of AChM receptors > blurring of vision, increased intraocular pressure, dry mouth, constipation (typical anti-muscarinic effects) Blockade of DA receptors in nigrostriatal pathway > Parkinsonian- Drug Haloperidol Class Neuroleptic Pharmacodynamics (MOA) Dopamine receptor antagonists (particular D2 + D4) > reduce dopamine transmission through mesolimbic region > reduction in positive symptoms Clinical Uses Treatment of schizophrenia Pharmacokinetics Initially compensatory mechanisms to increase DA synthesis, but these decline with therefore slow onset of action Side Effects Effects due to non-selectivity of antagonists: Blocking receptors in chemotactic trigger zone > anti-emetic Blocking of DA in tuberoinfundular pathway (endocrine) > excess prolactin > lactation Blockade of AChM receptors > blurring of vision, increased intraocular pressure, dry mouth, constipation (typical anti-muscarinic effects) Blockade of DA receptors in nigrostriatal pathway > Parkinsonian- Drug Sulpride Class Neuroleptic Pharmacodynamics (MOA) Dopamine receptor antagonists (particular D2 + D4) > reduce dopamine transmission through mesolimbic region > reduction in positive symptoms Clinical Uses Treatment of schizophrenia Pharmacokinetics Initially compensatory mechanisms to increase DA synthesis, but these decline with therefore slow onset of action Side Effects Effects due to non-selectivity of antagonists: Blocking receptors in chemotactic trigger zone > anti-emetic Blocking of DA in tuberoinfundular pathway (endocrine) > excess prolactin > lactation Blockade of AChM receptors > blurring of vision, increased intraocular pressure, dry mouth, constipation (typical anti-muscarinic effects) Blockade of DA receptors in nigrostriatal pathway > Parkinsonian- Drug Clozapine Class Neuroleptic Pharmacodynamics (MOA) Dopamine receptor antagonists (particular D2 + D4) > reduce dopamine transmission through mesolimbic region > reduction in positive symptoms Clinical Uses Treatment of schizophrenia Pharmacokinetics Initially compensatory mechanisms to increase DA synthesis, but these decline with therefore slow onset of action Side Effects Effects due to non-selectivity of antagonists: Blocking receptors in chemotactic trigger zone > anti-emetic Blocking of DA in tuberoinfundular pathway (endocrine) > excess prolactin > lactation Blockade of AChM receptors > blurring of vision, increased intraocular pressure, dry mouth, constipation (typical anti-muscarinic effects) Blockade of DA receptors in nigrostriatal pathway > Parkinsonian- 11. Anaesthetics General Anaesthetics • Common property: inducing loss of consciousness at low concentrations • Desirable effects: – loss of consciousness (propofol) – depression of thalamocortical neurons + RAS – analgesia (opiates) – suppression of reflex responses (enflurane) – depression of reflex pathways in spinal cord – muscle relaxation (NM blockers) – amnesia (benzodiazepines) – decreased synaptic transmission in hippocampus + amygdala • May be gaseous or intravenous • The more lipid-soluble, the more rapid the onset of action. For inhaled GAs, a lower blood-gas partition coefficient means more lipid-soluble and remains gaseous for longer. Drug Propofoll Class General anaesthetic Pharmacodynamics (MOA) Binds to GABA-a receptor to facilitate opening + GABA-mediated inhibition • B3 subunit = anaesthetic effect • A5 subunit = amnesia effect Clinical Uses Inducing loss of consciousness Pharmacokinetics Intravenous administration Fast recovery Drug Etomidate Class General anaesthetic Pharmacodynamics (MOA) Binds to GABA-a receptor to facilitate opening + GABAmediated inhibition • B3 subunit = anaesthetic effect • A5 subunit = amnesia effect Pharmacokinetics Intravenous administration Fast recovery Drug Nitrous oxide Class General anaesthetic Pharmacodynamics (MOA) Blocks excitatory NMDA-type glutamate receptors Neuronal nicotinic Ach receptor antagonists TREK (background leak) K+ channel agonists > increase hyperpolarisation Pharmacokinetics Gas administration Fast recovery Drug Halothane Class General anaesthetic Pharmacodynamics (MOA) Potentiate GABA-A receptor function (no subunit specificity) Blocks excitatory NMDA-type glutamate receptors Neuronal nicotinic Ach receptor antagonists TREK (background leak) K+ channel agonists > increase hyperpolarisation Pharmacokinetics Gas administration Medium recovery )higher blood-gas partition coefficient) Side effects Rare liver toxicity Drug Enflurane Class General anaesthetic Pharmacodynamics (MOA) Potentiate GABA-A receptor function (no sub-unit specificity) Blocks excitatory NMDA-type glutamate receptors Neuronal nicotinic Ach receptor antagonists TREK (background leak) K+ channel agonists > increase hyperpolarisation Clinical Uses Suppression of reflex responses and maintenance of anaesthesia Pharmacokinetics Gas administration Medium recovery (higher blood-gas partition coefficient) Local Anaesthetics • Definition: drugs which reversible block neuronal conduction when applied locally • Structural group areas: aromatic benzene-like ring, basic amine side chain (usually tertiary amine) + bridging group (ester linkage eg cocaine, amide linkage eg lidocaine) • Different routes of administration: – – – – – – Surface Infiltration (subcutaneous) Intravenous regional Nerve block Spinal Epidural Drug Cocaine Class Local anaesthetic (ester) Pharmacodynamics (MOA) Unionised basic structure diffuses inside sensory axon and then is ionized (to reach equilibrium). Ionized cation binds to voltage-sensitive Na+ channels, preventing rapid depolarisation by blocking the flow of ions = HYDROPHILIC PATHWAY Pharmacokinetics Surface administration Good mucuous membrane absorption Pka 8-9 90% plasma protein bound Metabolized in liver + plasma (non-specific esterases) T ½ 1 hour Side Effects CNS stimulation: restlessness, confusion, tremor (paradoxical) CVS: myocardial depression, vasodilation, hypotension Drug Lidocaine Class Local anaesthetic (amide) Pharmacodynamics (MOA) Unionised basic structure diffuses inside sensory axon and then is ionized (to reach equilibrium). Ionized cation binds to voltage-sensitive Na+ channels, preventing rapid depolarisation by blocking the flow of ions = HYDROPHILIC PATHWAY Pharmacokinetics Various routes of administration Hydrolysed in liver, then undergoes n-dealkylation 70% plasma protein bound T ½ 2 hours Side Effects CNS: euphoria and excitation CVS: increased cardiac output, vasoconstriction, hypertension