EPIGASTRIC PAIN
advertisement
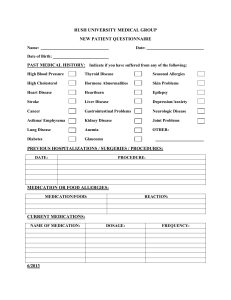
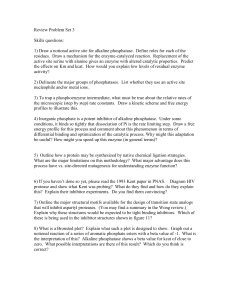
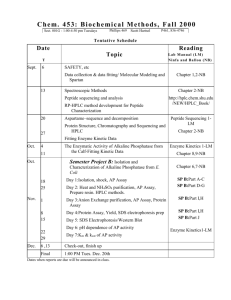
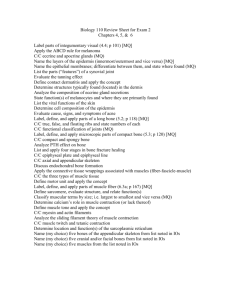
ER CASE REPORT PATRICK J. NAGLE A 79 y/o female Caucasian presented to the ED with a friend complaining of severe, sharp epigastric pain that radiated into her chest, back, and pelvic region. She has been having the pain for about 2 months, but it has progressively been getting worse since that time. Initially the pain was rated at a 2 or 3 out of 10, but within the past week has become a constant sharp pain rated between 8 and 10 out of 10. She now has a lot of difficulty eating because the pain is so severe. Pt thought she was constipated so she took some overthe-counter Colace thinking it would help. This was the only method of relief the pt attempted and it was unsuccessful. The pt denies having any fever, chills, night sweats, abnormal weight loss/gain, malaise, lymphadenopathy, difficulties or painful swallowing, N/V/D, blood in her mucus or stools, change in color or caliber of bowel movements, difficulties or changes in urination, wheezing, cough, SOB, SOB on exertion, chest tightness or pressure, palpitations, PND, orthopnea, fainting, dizziness, swelling of feet, or abnormal bleeding and bruising. Pt is known to have allergies to iodine resulting in kidney failure. PMH revealed documentation of Type II DM, HTN, hypercholesterolemia, CHF, stroke, MI, CAD, CABG x 3 - 2 months ago, AAA repair - 2 years ago, complete left mastectomy 7 years ago, GERD, removal of her gallbladder and appendectomy – over 20 years ago. Both sides of the patient’s family has a history of DM, HTN, dyslipidemia, and breast cancer is known on her side of the family. She has not been exposed/used tobacco, alcohol, or illicit drugs. Pt appears to be in moderate to severe discomfort with severe, sharp pain throughout the epigastric region of her stomach that radiated into the chest, back, and pelvic area. Abdominal aorta auscultated with no sounds indicating a possible leak. Normoactive bowel sounds with clicks and gurgles noted. 2+ peripheral pulses, radial and dorsalis pedis without radial/femoral delay were also noted to examine for a possible leak in the abdominal aorta. Pain in the epigastric and pelvic region was increased upon palpation and no organomegaly was noted. Lungs clear to auscultation and vesicular breath sounds were heard at the bases bilaterally with no crackles, rales, rhonci, rubs, or wheezing. RR at 20. Heart was a regular rhythm at a rate of 106, PMI was localized at the left 5th ICS mid-clavicular line. No S3, S4, murmurs, thrills, or lifts noted. Scarring was noted on the left side of the chest from prior CABG and mastectomy. Rectal exam to determine if there was any blood in the stool, which the stool guaiac was negative. The rest of the exam revealed no signs/symptoms of a disease process. AMI and a leaking AAA were the most emergent diagnoses. Bowel obstruction, pancreatitis, GERD, hiatal hernia, peptic ulcer disease, indigestion, constipation, and pneumonia were also included. Extensive labs were conducted because of the presentation. These included a CBC with diff., CMP, Amylase/Lipase, Troponin, CPK, U/A, Uroscreen, PT, PTT, INR, EKG and cardiac monitoring. Imaging studies that were completed consisted of a CXR, Abdominal Flat & Upright X-ray and MRI of the abdomen. EKG was immediately done - nonspecific T wave abnormality previously seen on the EKG. Troponin - 0.0, within normal limits (0.0 – 0.3). MRI and Abdominal Flat & Upright X-rays reviewed by the ER doctor to examine for any signs of a leaking AAA, bowel obstruction, pancreatitis, PUD, and constipation - No acute processes noted. CXR to r/o pneumonia - Negative. Amylase of 56 (range of 22-125 IU/L), lipase of 26 (range of 22-51 U/L) supported no acute pancreatitis. PT, PTT, and INR were within the accepted range. Lab results from the CBC with diff and CMP were in the accepted range for this institution, except for the alkaline phosphatase . Alkaline phosphatase - 548 (range of 42-121 IU/LA). Review of previous lab studies conducted on the patient since January of 2008 showed a slow and gradual elevation of the alkaline phosphatase. Radiologists interpretation of MRI - lytic lesions, often seen with bone metastasis from breast cancer. Lesions were imaged on the patient’s ribs, T&L spine, and pelvis. KEY HISTORY – PATIENT HAD A COMPLETE LEFT MASTECTOMY WITHOUT LYMPH NODE INVOLVEMENT 7 YEARS AGO. Therapeutic options for a progressed stage of cancer like this are only palliative in nature. Radiation or chemotherapy. Always consider the possibility of a relapse of cancer. Zebras are not common, but you must remain openminded to the possibility that you may see one. For this patient, catching the gradual increase of alkaline phosphatase and conducting the proper imaging studies could have lead to a different outcome and not a terminal illness. ALP. (2007, July 30). Retrieved July 8, 2009, from Lab Tests Online: http://www.labtestsonline.org/understanding/analytes /alp/test.html Degroot III, H. (2009). Bone Metastasis. Retrieved July 13, 2009, from Bonetumor.org: http://www.bonetumor.org/tumors/pages/page67.htm l Metastatic Bone Cancer. (2007, October). Retrieved July 8, 2009, from American Academy of Orthopaedic Surgeons: http://www.orthoinfo.aaos.org/topic.cfm?topic=A00093 What is Bone Cancer? (2009, May 13). Retrieved July 13, 2009, from American Cancer Society: http://www.cancer.org/docroot/CRI/content/CRI_2_4_ 1X_What_Is_bone_cancer_2.asp