Objectives: on facilitator version
advertisement
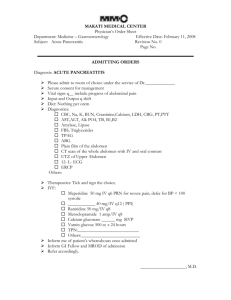
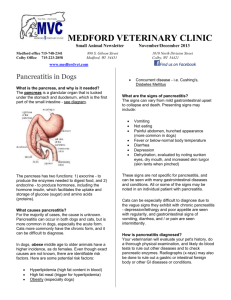
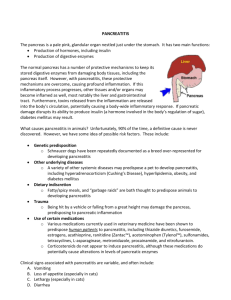
Learner Version Module #20 Objectives: on facilitator version References: on facilitator version CASE A 42 year old Male with no previous history presents to the ED with acute onset of epigastric pain that radiates to the back and is associated with nausea and vomiting. His only medication is ibuprofen for headaches. On physical examination, his temperature is 37.2 °C (99 °F), the blood pressure is 158/90 mm Hg, the pulse rate is 101/min, and the respiration rate is 20/min. There is no scleral icterus or jaundice. The abdomen is distended with mid-epigastric tenderness without rebound or guarding and with hypoactive bowel sounds. Labs: wbc 13, Hgb 12, Hct 36, Plt 231. LFTs: TP 6, Alb 3.8, AST 131, ALT 167, TB 1.1, DB 0.9, Amylase 824, Lipase 1432. Chem 7 is normal. Abdominal x ray shows mild ileus. What information is needed to establish the diagnosis of pancreatitis? What are the criteria? What is the most likely cause of this patient’s pancreatitis? What are physical exam findings important in the diagnosis of pancreatitis? You order an ultrasound. What information are you looking for on the ultrasound? In what instances should you obtain imaging other than ultrasound in patients with pancreatitis? What other orders are you writing at this time? The astute intern visits the patient after the resident has left and obtains additional history. The patient notes a history of drinking 1/5 vodka daily for the past 2 years and was on a recent binge. 1 ½ days later the patient continues to have severe mid-epigastric pain that radiates to the back, nausea, and vomiting. He has not been able eat or drink and has not had a bowel movement since being admitted. The nurse calls to notify you that the patient is diaphoretic, having increasingly worsening epigastric pain, and is toxic appearing. On repeat physical examination, the temperature is 38.2 °C (100.8 °F), the blood pressure is 182/84 mm Hg, the pulse rate is 131/min, and the respiration rate is 20/min. The abdomen remains distended and diffusely tender with hypoactive bowel sounds. Exam is otherwise normal other than that stated previously. Labs and studies? CT scan of the abdomen shows a diffusely edematous pancreas with multiple peripancreatic fluid collections, and evidence of 40% pancreatic necrosis. What is your next step in the management of this patient? gi_q011 The patient is started on Imipenem. GI and surgery consults are all obtained. The MICU is also called. A resident well known for “blocking” says that he will “keep an eye on your patient” overnight, but will not transfer at this time given that the patient remains hemodynamically stable. But what about that lactate? What is your plan now? Your patient is started on a dilaudid PCA and Imipenem. His lactate trends down and his vitals stabilize. He remains NPO and inpatient for 2 more days and then begins to tolerate a regular diet. He is monitored for 2 more days and then discharged. He is sent home with followup in 1 week. What are the long term complications of pancreatitis? If time: discuss feeding in acute pancreatitis. When do we decide to feed these patients? When do we consider enteral feeding? Associated GI MKSAP 16 questions for this module: A) B) C) D) Question 22 – Question 35 – Question 54 – Question 86 – Post Module Evaluation Please place completed evaluation in an interdepartmental mail envelope and address to Dr. Wendy Gerstein, Department of Medicine, VAMC (111). 1) Topic of module:__________________________ 2) On a scale of 1-5, how effective was this module for learning this topic? _________ (1= not effective at all, 5 = extremely effective) 3) Were there any obvious errors, confusing data, or omissions? Please list/comment below: _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ _________________________________ 4) Was the attending involved in the teaching of this module? Yes/no (please circle). 5) Please provide any further comments/feedback about this module, or the inpatient curriculum in general: 6) Please circle one: Attending Resident (R2/R3) Intern Medical student