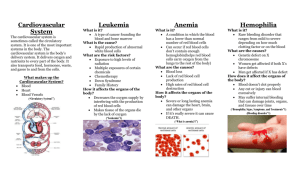
What is Hemophilia?
advertisement

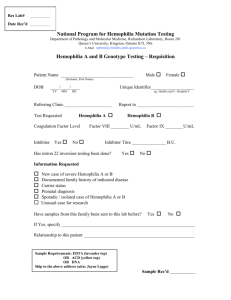
DIAGNOSIS OF HEMOPHILIA Nairobi, Kenya June 24, 2013 JIM MUNN, R.N., M.S. Program Nurse Coordinator University of Michigan HTC Ann Arbor, MI, USA Chair – WFH Nursing Committee Acknowledgement: Slides 20,21, 23-28 reproduced with permission from Partners in Bleeding Disorders Education Program www.partnersprn.org OBJECTIVES • Discuss the history of hemophilia • Illustrate the clotting cascade and how bleeding occurs • Describe the two main types of hemophilia • Classify the severities of hemophilia • List common presenting symptoms in patients with hemophilia • Examine the process of diagnosing hemophilia • Identify common labs used to diagnose hemophilia EARLY OBSERVATIONS Twelfth Century Physician and Talmudist Maimonides states in the Mishneh Torah1 “If a woman had her first son circumcised and he died as a result of the circumcision, which enfeebled his strength, and she similarly had her second [son] circumcised and he died as a result of the circumcision whether [the latter child] was from her first husband or her second husband the third son may not be circumcised at the proper time [on the eighth day of life]…”2 1. Rosner F. “Moses Maimonides.” Ann Intern Med. 1965;372:1135-1204. 2. Mishneh Torah, Hilkhot Milah. 1:18. EARLY OBSERVATIONS 1803: John Conrad Otto • Provided first accurate account of hemophilia in the modern medical literature • His investigation of “bleeders” was published in a New York journal under the title, “An Account of an Hemorrhagic Disposition Existing in Certain Families” • Traced to woman who settled in Plymouth, New Hampshire in 1720 Otto JC. The Medical Repository. 1803;Vol VI (No 1):1-4. EARLY OBSERVATIONS 1820: Nasse of Bonn • German physician 1778-1851 • Formulated observations on inheritance of hemophilia • “Nasse’s Law”: Transmitted by unaffected females to their sons Nasse CF. Arch Med Erfahr. 1(1820):385. EARLY OBSERVATIONS 1828: The word “hemophilia” first appears in a description of inherited bleeding disorders by Physician Frederick Hopff at the University of Zurich 1840: First recorded case of hemophilia treatment by transfusion written by Samuel Lane in The Lancet 1 1893: First documentation of abnormal prolongation of coagulation in capillary tube in hemophilics2 1. Farr AD. J Royal Soc Med. April 1981;74(4):301-305. 2. Wright AE. Br Med J. 1893;2:223-225. THE ROYAL DISEASE: QUEEN VICTORIA FAMILY TREE THE COAGULATION SYSTEM Procoagulants Platelet Endothelial Cell Fibrinolysis Coagulation inhibitors THE CLOTTING CASCADE Intrinsic pathway (I.P.) Extrinsic pathway (E.P.) XII XI IX VII VIII X V Prothrombin (II) Fibrinogen Thrombin Fibrin CLOT FORMATION XIII HOW DOES CLOTTING OCCUR? WHAT IS HEMOPHILIA? • Rare, genetic condition • Gene located on the X chromosome • Results in bleeding manifestations in affected individuals • Present at birth and continues throughout life • Decreased amount or impaired functioning of one of the plasma proteins • Usually factor VIII (eight) or IX (nine) • Factor levels usually do not change over time WHY DO PEOPLE WITH HEMOPHILIA BLEED LONGER? • In hemophilia, one clotting factor is missing, or the level of that factor is low. • It is difficult for the blood to form a clot, so bleeding continues longer than usual (not faster). TYPES OF HEMOPHILIA Types Prevalence % of Cases Hem A/Factor VIII 1:5,000 males 80-85% Hem B/Factor IX 1:25,000 males 15-20% Hem C/Factor XI All types: • Affect all races • Worldwide distribution SEVERITY OF HEMOPHILIA • Low levels of factor VIII (eight) = hemophilia A. • Low levels of factor IX (nine) = hemophilia B. • Hemophilia A and B can be mild, moderate, or severe, depending on the level of clotting factor. Severity of symptoms often corresponds to factor level COMMON PRESENTING SYMPTOMS IN HEMOPHILIA • Bleeding at circumcision • Mouth bleeds in young children • Excessive bruising, hematomas – especially in areas not subjected to bumps and scrapes • Head bleeding related to birth trauma • Joint bleeding • Muscle bleeding • Bleeding after surgery, dental work, or trauma • In severe hemophilia, bleeding can be spontaneous DIAGNOSING HEMOPHILIA: HISTORY AND PHYSICAL • Accurate and detailed history with assessment of bleeding episodes and trauma in individuals with bleeding disorders is essential for determining appropriate care • Use age-appropriate approach • Get a patient and family history • Start general (ROS), get specific • History and assessment may be as, or more, important as labs/imaging • Listen to the patient and family • The process is continuous from first notification of event to follow-up THE 7 HISTORY AND ASSESSMENT QUESTIONS 1. What are the symptoms? 2. How long have the symptoms been present? 3. What treatment was given, and when? 4. Did an injury happen before the symptoms started? 5. Did a similar problem occur in the past? 6. How was that problem treated? 7. Did that treatment resolve the issue? LABORATORY EVALUATION • Laboratory evaluation is guided by thorough history & physical examination • Clinical impression is critical to determine: - Extent of evaluation - Phase of coagulation most likely abnormal - Need for repeated evaluations LABORATORY EVALUATION: GUIDED BY SYMPTOMS • Petechiae • Abnormal bruising • Mucocutaneous bleeding Abnormal platelet number or function • Deep tissue, muscle, joint bleeding • Abnormal bruising • Bleeding with injury, surgery → Abnormal procoagulants • Delayed bleeding → Abnormal fibrinolysis THE CLOTTING CASCADE: PT AND APTT Intrinsic pathway (I.P.) Extrinsic pathway (E.P.) XII XI IX VII VIII X APTT PT V Prothrombin (II) Fibrinogen Thrombin Fibrin CLOT FORMATION XIII LABORATORY EVALUATION: APTT • Activated partial thromboplastin time (aPTT) • Non-specific test of “intrinsic system” • aPTT screens for abnormality in factors VIII, IX, XI, XII Activated Partial Thromboplastin Time. Virginia Commonwealth University, 2005. http://www.pathology.vcu.edu/clinical/coag/aPTT.pdf. Laboratory Evaluation of Hemostasis. Virginia Commonwealth University, no date. http://www.pathology.vcu.edu/clinical/coag/Lab%20Hemostasis.pdf. LABORATORY EVALUATION: PT • Prothrombin time (PT) • Tests efficiency of “extrinsic system” • PT sole abnormality factor VII • Abnormality of PT may be due to deficiency in factors VII, X, V • Somewhat useful for detecting changes in factors II (prothrombin) and I (fibrinogen) Laboratory Evaluation of Hemostasis. Virginia Commonwealth University, no date. http://www.pathology.vcu.edu/clinical/coag/Lab%20Hemostasis.pdf LABORATORY EVALUATION: PROLONGED PT AND APTT Common pathway • Both PT & aPTT prolonged • May be due to deficiency in factors X, V, II, I (fibrinogen) • May also indicate vitamin K deficiency: factors II, VII, IX, X Laboratory Evaluation of Hemostasis. Virginia Commonwealth University, no date. http://www.pathology.vcu.edu/clinical/coag/Lab%20Hemostasis.pdf MIXING STUDY • Prolonged coagulation screening tests such as PT & aPTT should first be followed by a mixing study • Mixing study consists of mixing equal parts the patient’s plasma with a known normal plasma • Coagulation test is then repeated • Correction of the test to the normal range = Factor deficiency • Lack of correction of the test to the normal range = Inhibitor Partial Thromboplastin Time Mixing Study. University of Alabama at Birmingham Coagulation Service, no date. http://peir.path.uab.edu/coag/article_101.shtm Patient with prolonged aPTT + aPTT corrects = Factor deficiency Mixed with normal plasma Patient with prolonged aPTT + aPTT does not correct or re-prolongs with incubation = Inhibitor Mixed with normal plasma SPECIFIC FACTOR ASSAYS • Factor VIII level • Factor IX level • May need repeat testing as factor IX levels are typically low at birth due to immature liver (vitamin K-dependent protein) • Cord blood sampling can be done • Exposure to blood products for treatment can falsely elevate factor levels SUMMARY • Hemophilia has been around as long as people have been around. • Hemophilia is not a “Royal Disease”. • Symptoms typically appear earlier in life in severe disease. • Clotting involves a complex series of reactions between a number of components. • The diagnosis of hemophilia requires a coordinated approach. • Careful history and physical should precede any laboratory investigations. • Labs may need to be repeated. ADDITIONAL WFH RESOURCES • Diagnosis of Hemophilia and Other Bleeding Disorders: A Laboratory Manual • Guidelines for the Management of Hemophilia, 2nd edition, Section 3. Visit the Publications Library at www.wfh.org/publications for free copies