Understanding Chronic Pain And A Pathway Approach
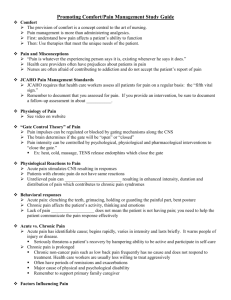
advertisement

Developing Integrated Care Clinical Pathways: The Example of Chronic Pain Kirk Strosahl Ph.D. Central Washington Family Medicine mconsultinggrp@embarqmail.com www.behavioral-health-integration.com Clinical Pathway Targets: What Are the Priorities in Your Clinic? • High prevalence (depression) or high impact (chronic pain) conditions • Variability among providers • Evidence available for preferred treatment • Patient preference • Provider preference • Resources (opinion leaders, grants) • Cost savings or practice leveraging Five Steps To Developing Population-Based Pathways 1. Choose a common condition that is amenable to a systems approach to care. 2. Identify a method for identifying patients in the primary care practice who have the selected condition. 3. Choose measurable outcomes that reflect best evidence-based medical or behavioral health practice for that condition. 4. Form a high performance team to implement a system of care that improves outcomes. 5. Measure outcomes regularly and make changes as needed to improve outcomes Examples of Clinical Pathway Targets • • • • • • • Depression Alcohol-Drug Abuse Diabetes Chronic Pain Syndrome Anxiety Smoking Obesity Qualities of an Integrated Pathway • Stepped care approach to accommodate varying levels of severity and motivation • Shortened sessions • Condensed treatment packages • Multiple delivery formats • Patient education philosophy • Designed for use by all PC team members • Culturally competent What Makes Chronic Pain So Difficult For Physicians? • There is no cure for it (even successful treatment involves residual pain) • The help seeking, help rejecting stance of CP patients (My pain is at a 10, but don’t try to get me to do those morning stretches) pushes a lot of hot buttons • Negative feedback loop (nothing you are doing is helping me) makes it very unrewarding for the provider • Fear of substance abuse, addiction and diversion and possible legal sanctions • Many PCPs use acute care strategies for a problem which is a chronic condition (PRN medications for pain presentations) and thus develop a revolving door What Makes Chronic Pain So Difficult For The Patient? • • • • • • • • Pervasive sense of isolation Loss of contact with a “normal day” Perception that others do not believe the pain is real Perception of being promised one thing (a cure), but delivered another (a curse) by the medical establishment Perception of being viewed as an “addict” by others because of dependency on narcotics Criticism from family members and friends for variable day to day performance Self criticism for not being able to “rise above the pain” Common co-morbid states like depression, anxiety amplify pain experience Which Treatments Are Effective for Chronic Pain and Which Aren’t? • Evidence for long term usefulness of narcotics is very limited (particularly end state functioning) • NSAIDS are more likely to reduce or eliminate pain and should be first line treatments • Cognitive and behavioral interventions have been repeatedly shown to be effective at improving functional status, less so with pain • Regimens of exercise aimed at stretching and limbering have been repeatedly shown to reduce pain and improve functional status A Contextual Behavioral Model of Chronic Pain (McCracken, 2006) • Pain plus the unwillingness to have pain leads to a refusal to accept the reality of pain • Pain is perceived as the main obstacle to vital living; thus, the goal is first to eliminate pain and then vital living can happen • Since pain cannot be controlled or eliminated, the paradoxical result is an increasing focus on pain experience and its elimination • This leads to an ever widening pattern of behavior designed to control pain, at the expense of living a vital life Components of Contextual Cognitive Behavioral Treatment • Pacing—Adapting daily activity pattern to match pain tolerance, so as to optimize “up time” • Attention Diversion—Mental strategies for focusing attention away from pain, or re-associating pain sensations in a way that reduces pain experience • Cognitive Restructuring—Strategies designed to defeat “pain catastrophizing” and pain related avoidance • Acceptance/Mindfulness—Strategies that promote pain acceptance and the ability to stay detached in the presence of pain • Value Based, Motivation Enhancement—Strategies designed to clarify and help patient pursue valued life directions in spite of pain Clinical Philosophies of the Pain and Comfort Program • Pain must be assessed and treated within a biopsychosocial framework • The goal of treatment is not the elimination of pain, but the restoration of functioning • Any treatment that is not improving functional status will not be continued • Long term narcotics treatment always comes with “strings attached” • Evidence based care is the strongest platform from which to engage the patient • All chronic pain patients started as acute pain patients and thus there must be a place for prevention Pain & Comfort Program Goals • • • • Promote functional improvement Increase pain acceptance & engagement in life Decrease reliance on long term narcotics use Identify and manage patients at risk for substance abuse or addictive behaviors • Prevent the onset of chronic pain by working aggressively with acute pain patients • Seamlessly integrate behavioral and medical interventions within a single care plan Primary Care Behavioral Health Model: The Platform For An Integrated Pain Pathway • Behavioral Health Consultation – BHC works within medical exam room area as a core team member – Schedule is open and designed for fast, easy access at the time of medical visits (Lucy is in) – Visits are short (15-25 minutes) and consultatively oriented – The MD remains “in charge” of the patient’s healthcare plan – Intervention model is a temporary co-management approach – Most patient encounters are warm handoffs from a immediately preceding medical visit Components Of The CWFM Pain & Comfort Program • Standardized format for initial MD assessment – Establish the diagnosis (acute vs. chronic pain) – Assess level of pain related disability – Establish the treatment plan (includes medication and behavioral management) – Assess potential for opiod abuse and make a decision about medication (Opioid Risk Tool) – Establish pain contract and set functional goals – Refer to BHC in every case for evaluation of psychosocial factors and preparation for class Components of the CWFM Pain and Comfort Program • Treatment Phase – Generally, long acting narcotics are substituted for short acting narcotics as the base pain treatment – Monthly Pain and Comfort Class is center piece of the treatment and is required for continuation of narcotics – Class uses CCBT model of pain treatment with different modules offered repeatedly over time – Pain disability assessments are taken on every patient at every class meeting – Scores entered into EMR note, along with narrative comments about patient progress Components of the CWFM Pain and Comfort Program • Progress Monitoring – Outcomes are measured monthly in terms of pain disability index and pain acceptance scale – PADT (Pain Assessment Documentation Template) used by MD’s at every pain management visit – Failure to improve in functional status over time triggers a review of the entire treatment plan • MD and BHC consult to identify barriers to improvement and develop new interventions • MD may choose to taper off narcotics because of lack of functional improvement Components of the CWFM Pain and Comfort Program • Risk Monitoring – “Three Strikes Program” establishes three levels of aberrant drug use behavior • Misuse/abuse/addiction – Misuse re-educate patient – Abuse Caution • Express concern and set limits • Consider tapering/stopping addictive medicines • Consider specialty consultation or referral to BHC for 1:1 evaluation – Addiction/Diversion STOP Components of the CWFM Pain and Comfort Program • Prevention – Chronic pain syndrome is an iatrogenic phenomenon – By changing the initial “message” to acute pain patients, MD’s and the BHC can avoid the control and eliminate pain trap • Protocol – When an acute pain patient requests the first refill of a prescribed narcotic, an automatic referral to the BHC is generated – A chronic pain risk assessment is performed – A high risk patient is managed differently than a low risk patient Components of the CWFM Pain and Comfort Program • High Risk Patient Prevention Protocol – A definite, short range date is set for the termination of narcotic medicine – Patient is told that some pain complaints turn out to be chronic and the goal is to learn to live a vital life even if the pain persists – BHC is involved with patient to teach pain management skills, to identify the patient’s values and to address any reversible risk factors (i.e., patient hates job or is seeking workman's’ compensation for an injury) Summary • Chronic pain syndrome is a complicated biopsychosocial disorder that nevertheless is very manageable using an integrated primary care team model • The new contextual behavioral treatments are extremely potent and are easily adapted to a classroom format • Physicians readily respond to a structured, evidence based approach that is easily learned and easy to apply • Clinic wide, the program is actually popular with patients and has improved MD self perceived efficacy in working with chronic pain patients • A fully integrated biopsychosocial program for chronic can be implemented in a relatively short period of time