Comfort & Pain Management Nursing Study Guide
advertisement

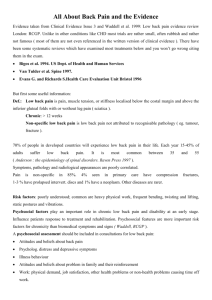
Promoting Comfort/Pain Management Study Guide Comfort The provision of comfort is a concept central to the art of nursing. Pain management is more than administering analgesics. First: understand how pain affects a patient’s ability to function Then: Use therapies that meet the unique needs of the patient. Pain and Misconceptions “Pain is whatever the experiencing person says it is, existing whenever he says it does.” Health care providers often have prejudices about patients in pain Nurses are often afraid of contributing to addiction and do not accept the patient’s report of pain JCAHO Pain Management Standards JCAHO requires that health care workers assess all patients for pain on a regular basis: the “fifth vital sign.” Remember to document that you assessed for pain. If you provide an intervention, be sure to document a follow-up assessment in about ___________. Physiology of Pain See video on website “Gate Control Theory” of Pain Pain impulses can be regulated or blocked by gating mechanisms along the CNS The brain determines if the gate will be “open” or “closed” Pain intensity can be controlled by psychological, physiological and pharmacological interventions to “close the gate.” Ex: heat, cold, massage, TENS release endorphins which close the gate Physiological Reactions to Pain Acute pain stimulates CNS resulting in responses Patients with chronic pain do not have same reactions Unrelieved pain can _________________________ resulting in enhanced intensity, duration and distribution of pain which contributes to chronic pain syndromes Behavioral responses Acute pain: clenching the teeth, grimacing, holding or guarding the painful part, bent posture Chronic pain affects the patient’s activity, thinking and emotions Lack of pain ___________________ does not mean the patient is not having pain; you need to help the patient communicate the pain response effectively Acute vs. Chronic Pain Acute pain has identifiable cause; begins rapidly, varies in intensity and lasts briefly. It warns people of injury or disease. Seriously threatens a patient’s recovery by hampering ability to be active and participate in self-care Chronic pain is prolonged Chronic non-cancer pain such as low back pain frequently has no cause and does not respond to treatment. Health care workers are usually less willing to treat aggressively Often have periods of remissions and exacerbations Major cause of physical and psychological disability Remember to support primary family caregiver Factors Influencing Pain Age Observe for behavioral changes in children that indicate pain Pain is NOT a normal part of _____________ Gender? Culture Affects how people perceive the cause of pain and how they react to and express pain (stoic vs. emotive) Recognize how your own culture influences your attitude about pain and be sensitive to others Meaning of Pain Experience Attention/Distraction Anxiety High anxiety increase pain perception _________________ causes anxiety Depression High rates of depression with chronic pain; routinely assess for suicidal tendencies Fatigue Intensifies pain and decreases coping abilities Previous experience Successfully vs. unsuccessfully resolved affects pain relief Coping Style Internal loci of control vs. External loci Family and Social Support Educate the caregivers as well Assessing Pain For Acute Pain P: precipitating or aggravating factors Q: Quality of pain: “Tell me what your pain feels like.” somatic, visceral, neuropathic R: Relief measures and Region S: Severity: 0-10 or FACES T: Timing (onset, duration, pattern) U: Effect of pain on patient For chronic pain focus on emotional impact and level of function Be aware of patients who cannot communicate pain effectively: Children or developmentally delayed Aphasic patients Psychotic patients Patients with dementia Non-English speaking patients Assessing Pain: Objective Acute pain: VS: increased HR, RR, BP Pallor, Diaphoretic, dilated pupils, grimacing, restless/anxious, holding of painful part Chronic pain: VS normal but often emotionally depressed or withdrawn Assess Patient Expectations Always ask patients what they expect regarding their comfort needs What interventions they prefer How they expect you to administer them Full pain relief or reduced discomfort Planning Develop individualized plan of care Set Priorities Collaboration Family Therapists/Specialists Clergy Implementation Your ability to show caring (compassion) will maximize pain control. Task-oriented and affective touching will benefit patients Health Promotion Maintain wellness: warm baths, personal hygiene measures, schedule of adequate rest If limited mobility r/t pain: help them retain function. Refer to Occupational therapist (with order) as needed Non-pharmacological Pain Relief Measures Prevent painful stimuli (positioning, smoothing wrinkled linen, change wet linen, monitor for bladder distension; protect skin from irritants) Anticipatory guidance: Give detailed descriptions of procedures before to decrease anxiety Distraction: singing, praying, listening to music, describing photos, telling jokes and playing games Cutaneous stimulation Massage, Cold/Heat, TENS (requires order) Relaxation techniques Simple relaxation, guided imagery Pharmacological Therapy Analgesics _____________________________ Acetaminophen, Tramadol (Ultram), and NSAIDs are effective for mild to moderate pain Ketorolac (Toradol) is injectable NSAID used for severe pain NSAIDS inhibit prostaglandins and inflammation Pharmacological Therapy ___________________________ are for severe pain Include codeine, morphine, hydromorphone (Dilaudid), Fentanyl, oxycodone, propoxyphene. Demerol is no longer a drug of choice because of potential for seizures Work on CNS and can depress respirations (so assess respirations before administering) Other common side effects: nausea, vomiting, constipation and altered mental processes If used around the clock (ATC) for a week or more, expect physical dependence (withdrawal symptoms occur if abruptly stopped). This is not the same as addiction which is psychological dependence. Patient controlled analgesia (PCA) Safe, effective drug delivery system via an IV line that allows patients to administer pain medications when they need them based on parameters set by the health care provider (for example, 1 mg of Morphine available every 6 minutes with a hourly limit of 10 mg) Can also be given at a low dose basal rate Patient education is CRITICAL for effective use Patients with Cancer Pain: can be debilitating and difficult to treat See WHO ladder: begin with NSAIDS the progress to opioids and adjuvants if persists Goal: anticipate and prevent/minimize pain ATC or transdermal may be useful but also treat for constipation Hospice Helps terminally ill patients live at home with the help of a health care team Pain control is a priority Teach and reassure about end-of-life maximum pain relief by titrating (increasing) dosages to meet needs and alleviate suffering Promoting Comfort: GI symptoms Promoting Comfort in the Terminally Ill Patient Interventions for nausea and constipation also apply to non-terminally ill patients receiving opioids for pain relief Also see textbook for interventions to promote GI function and promote comfort in post-operative client Common antiemetic meds: Compazine, Reglan, Zofran Promoting Comfort: pruritis Pruritis (_______________) is a common side effect of Morphine. May require patient to be switched to alternative opioid or may be resolved with medication such as Benadryl. Evaluation of Pain Management Compare baseline pain assessments with ongoing assessments Also evaluate if response to pain has changed – is patient able to perform activities that pain prevented? Consider abuse/misuse for long-term use– it is rare, but if suspected, refer to a pain specialist Ask patient if we have met their expectations