Connective tissue mast cells
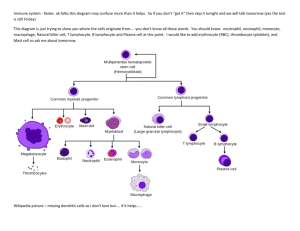
advertisement

Basophils and mast cells and their importance in immune responses Mast cells Mucosal mast cells - in the mucous membranes of respiratory and gastrointestinal tract, produce histamine, serotonin, heparin, tryptase, leukotriene C4 ..., participate in parasitosis and allergy Connective tissue mast cells - the connective tissue, producing tryptase, chymase, prostaglandinD2 ..., are multiplicated in fibrosis, in parasitosis and allergy are not participating Mast cell functions Defense against parasitic infections In pathological circumstances, responsible for the early type of hypersensitivity (immunopathological reaction typeI) Apply during inflammation, in angiogenesis, in tissue remodeling Mast cell activation Mast cells can be stimulated to degranulate by: cross-linking of IgE Fc receptors by anafylatoxins (C3a, C4a, C5a) direct injury, alcohol, some antibiotics Mast cell activation by cross-linking of IgE Fc receptors Establishing of multivalent antigen (multicellular parasite) to IgE on highaffinnity Fc receptor for IgE (FcRI) Aggregation of several molecules FcRI Initiate mast cell degranulation (cytoplasmic granules mergers with the surface membrane and release their contents) Activation of arachidonic acid metabolism (leukotriene C4, prostaglandin D2) Start of production of cytokines (TNF, TGF, IL-4, 5,6 ...) Mast cell activation scheme Secretory products of mast cells Cytoplasmatic granules: hydrolytic enzymes, proteoglycans (heparin, chondroitin sulphate), biogenic amines (histamine, serotonin) Histamine causes vasodilation, increased vascular permeability, erythema, edema, itching, contraction of bronchial smooth muscle, increases intestinal peristalsis, increased mucus secretion of mucosal glands in the respiratory tract and GIT (helps eliminate the parasite) Arachidonic acid metabolites (leukotriene C4, prostaglandin D2) Cytokines (TNF, TGF , IL-4, 5,6 ...) The role of mast cells in development of allergy Basophils Differentiate from myeloid precursor Receptor equipment, containing granules, the mechanisms of stimulation and functions are very similar to mast cells They are responsible for the emergence of anaphylactic shock Basophil activation markers: CD 63, (CD 203) Immune mechanisms of inflammation (Local and systemic reactions) Inflammation * Is a summary of physiological responses to breach the integrity of the organism, leading to protection against infection of damaged sites, localization of damage and healing. Local body's response to inflammation Manifestations - pain (dolor), fever (calor), redness (rubor), swelling (tumor) Inflammation • The first signals to the development of inflammatory responses come from mast cells, phagocytes, and the substances released from damaged cells and extracellular components of matter. Inflammation Local inflammation - increased permeability of blood vessels (vasoactive amines, complement components C3a, C5a, leukotrienes ..., swelling at site of inflammation) → rednes, swelling - increased expression of adhesion molecules on endothelia - activation of coagulation, fibrinolytic, kinin and complement system - influence of local nerve endings via prostaglandins → pain - changes in temperature (IL-1, IL-6, TNF, prostaglandins) Systemic response to inflammation - leukocytosis - fever (proinflammatory cytokines TNF, IL-1, IFN ; stimulate hypothalamic center of thermoregulation) - mobilization of tissue metabolism - induction of expression of Hsp (heat-shock-proteins; function as chaperones) - production of acute phase proteins (CRP, SAP, C3, C4; opsonization and complement activation) by liver after stimulation with cytokines (TNF-α, IL-1, IL-6) - increased hepatic synthesis of certain serum transport proteins (ceruloplasmin, transferrin) - increased synthesis of protease inhibitors ( macroglobulin) Septic shock - the massive penetration of microorganisms into the bloodstream (TNF) Anaphylactic shock - basophil degranulation and complement activation with allergen (histamine) Repair of damaged tissue - elimination of damaged cells with phagocytes - activation of fibroplastic mechanisms - activation of angiogenesis - regeneration and tissue remodeling Physiological mechanisms of regulation of the immune system Regulation by antigen Induce immune responses and extinction Affinity maturation of B lymphocytes Maintaining immunological memory Antigenic competition Threshold density of the complex MHC II-gp Ag on APC Regulation by antibodies Antibodies competes with the BCR for antigen (negative regulator of B lymphocyte stimulating) IgG immune complexes bind to the BCR and FcR on B cells, resulting in blocking activation of B lymphocytes Regulation via idiotypic network Regulation by cytokines and cellular contact Interaction APC - T lymphocyte Interaction TH1 – macrophages Interaction TH2 - B lymphocytes Mutual regulation of activity TH1 versus TH2 Development of leukocyte subpopulations Negative regulation of effector cells: CTLA-4 - T cell inhibitory receptor, binds ligands CD80 and CD86 Inhibitory receptors of NK cells Self-destruction interaction of the apoptotic receptor Fas with ligand FasL on the surface of activated T lymphocytes Interaction of APC with T lymphocyte T cell: TCR - antigen-specific receptor (signal 1) CD4 or CD8 - coreceptor (MHCgp binding) CD 28 - costimulatory receptor (signal 2, binds CD 80, CD 86) CTLA-4 - inhibitory receptor (binds CD 80, CD 86) CD-40L APC: MHC gp I + antigenic peptide MHC gp II + antigenic peptide CD 80, CD 86 - costimulatory ligands CD 40 Suppression mediated by T lymphocytes Mutual negative interaction TH1 and TH2 cytokine-mediated (TH2 lymphocytes produce IL-4 and IL-10 that suppress the immune response based on TH1 cells) Clonal elimination or anergy of T lymphocytes after contact with antigen on the surface of other cells than APC (lacking costimulating signals) Regulatory T cells (Tr1 CD 4+) help to maintain tolerance to autoantigens Factors influencing the outcome of the immune response The same antigen can induce an active immune response or an active state of tolerance, the result of response depends on many factors: State of the immune system Properties of antigen Dose of antigen Route of antigen administration Cytokines (Tissue hormones) Cytokines Regulatory proteins and glycoproteins produced by leukocytes and other cells Essential regulators of the immune system Apply also outside the immune system (angiogenesis, tissue regeneration, carcinogenesis, treatment of many brain functions, embryonic development ...) Cytokines - secreted - membrane (CD 80, CD86, CD40L, FasL ..) Pleiotropic effect Operates in a cascade Cytokine Network Cytokine system is redundant Effects of cytokines - autocrine - paracrine - endocrine Are known as interleukins (exception: TNF, lymphotoxin, TGF, interferons, CSF and growth factors) B cells communicate via cytokines with other inflammatory cells, such as T cells and macrophages Distribution of cytokines according their function Proinflammatory cytokines (IL-1, IL-6,IL- 8,IL- 12,IL- 18, TNF) Antiinflammatory cytokines (IL-1Ra, IL-4, IL-10, TGF) Cytokines with the activity of hematopoietic cells growth factor (IL-2, 3, 4, 5, 6, 7, 9, 11, 14, 15, CSF, SCF, LIF, EPO) Cytokines applying in TH2 humoral immunity (IL-4, 5, 9, 13) Cytokines applying in the cell-mediated immunity TH1 (IL-2, 12, IFN, GM-CSF, lymphotoxin) Cytokines with anti-virus effect (IFN-, IFN- , IFN- ) Overview of the most important cytokines Cytokine Produced Function IL-1 MF, N T cell costimulation, induction of TNF and IL-8, pyrogen IL-2 Th1 Growth factor for T cells IL-4 Th2, basophils Th2 differentiation, B cell stimulation, isotype switching to IgE and IgG4, Th1 inhibition IL-5 Th2, eosinophils B cell stimulation, growth factor for eosinophils IL-6 Th2, MF, N T and B cell stimulation, stimulation of Ig production, induction of acute phase proteins synthesis, pyrogen IL-8 MF, other cells Granulocyte activation and chemotaxis (primarily neutrophils) IL-10 Th2,M, Treg Th1 and MF inhibition, B cell differentiation to plasma cell IL-12 MF, DC, B Th1 differentiation, NK stimulation TNF M, MF, NK Induction of local inflammation, endothelium activation, induction of apoptosis TGF T, MF, platelets The anti-inflammatory effect (control of lymphocyte proliferation, control of Ig production, control MF activity), stimulation of fibroblasts and osteoblasts, gain production of extracellular matrix IFN L, M, MF Inhibition of viral replication IFN Fibroblasts, epithelial cells Inhibition of viral replication IFN Th1, NK MF activation, stimulation of MHC gp. expression, Th2 inhibition MF – macrophages; M – monocytes; N – neutrophils; DC – dendritic cells; NK – natural killers; L – lymphocytes; B – B cell; T – T cell Cytokine receptors Consisting of 2 or 3 subunits One subunit binds cytokine, other are associated with cytoplasmic signaling molecules (protein kinases) Signaling subunit is shared by several different cytokine receptors - called receptor family Signaling through these receptors may lead to proliferation, differentiation, activation of effector mechanisms or blocking the cell cycle and induction of apoptosis HLA system (MHC glycoproteins) MHC glycoproteins class I (Major histocompatibility complex) The function of MHCgpI is presentation of peptide fragments from inside the cell (which are produced by cell, including viral peptides if are present) on the cell surface to T lymphocytes (cytotoxic CD8+) Present on all nuclear cells of the organism 3 isotypes of classical human MHC gp. (HLA - A,-B,-C) 3 isotypes of nonclassical MHC gp. (HLA - E,-F,-G; molecule CD1) Structure of MHC gp I MHC gp class I consists of transmembrane chain and non-covalently associated 2mikroglobulin chain has 3 domains, 2 N-terminal (1, 2 - binding site for peptides) and 1 C-terminal domain (3 anchored in the cytoplasmic membrane, a structure similar to imunoglobulin domain) Binding of peptide is necessary for a stable conformation of MHCgp and thus ensure its long presentation on the cell surface Peptides binding to MHCgpI MHC gp I bind peptides with a length of 8 to 10 aminoacides Certain MHC gp molecule binds peptides sharing common structural features - coupling motif (critical are aminoacides near the end of peptide) The binding of endogenous peptides occurs in the endoplasmic reticulum during biosynthesis of MHC gp Peptides binding to MHCgpI After a string and 2mikroglobulin create in the ER, folding into the correct conformation and the mutual association and the association of an appropriate peptide, the complex is further processed in the Golgi apparatus and then is presented on the cell surface Linked peptides derived from proteins degraded proteasome, which cleaves cytoplasmic proteins for destruction (labeled with ubiquitin), peptide fragments are transported into the ER by specific membrane pump Peptides binding to MHC gp I Non-classical MHC gp I HLA - E,-F,-G; CD1 molecules Structurally similar to classical MHC gp Are less polymorphic There are only on some cells They specialize in binding of specific ligands HLA-E and HLA-G - occurs on the trophoblast cells Complexes of HLA-E and HLA-G with peptides are recognized by inhibiting receptors of NK cells and contribute to the tolerance of the fetus in utero CD1 molecules - bind glycolipids (recognized by NK-T lymphocytes) MHC glycoproteins class II The function of MHC gpII is the presentation of peptide fragments from protein whitch were engulfed by antigen presenting cell on the cell surface to T lymphocytes (auxiliary CD4) Occur on the APC (dendritic cells, monocytes, macrophages, B lymphocytes) 3 isotypes of MHC gpII (DR, DQ, DP) Structure of MHC gp II MHC gp II consist of 2 non-covalently associated transmembrane subunits and The peptide binding site consists of N-terminal domains 1 and 1 Binding of peptide is necessary for a stable MHC gp conformation and thus ensure its long presentation on the cell surface Binding of peptides to MHC gp II MHC gpII bind peptides with a length of 15 to 35 aminoacides (but possibly longer - because the peptide binding site is open at both ends) Certain MHC gp molecule binds peptides sharing common structural features - coupling motif Binding of peptides to MHC gp II After a string and are created in ER, fold into the correct conformation and the mutual associated are connected with another transmembrane chain called invariant chain, which blocks the binding site for the peptide, this complex is further processed in the Golgi apparatus, secretory vesicles isolated from GA merge with endosomes, then split the invariant chain and peptide fragments from cell absorbed proteins bind into binding site of MHC gp and the complex is then presented on cell surface Peptides binding to MHC gp II HLA system – genetic background HLA complex is localized on chromosome 6 Codominant inheritance of HLA ( Individual has 3 cell surface isotypes of HLA molecules (HLA-A,-B,-C) mostly in 2 different alelic forms ) Polymorphism of MHC glycoproteins For MHC gp is typical high polymorphism (except the non-classical MHC gp) Polymorphism has a protective significance at individual and population level Ppolymorphism MHC gp causes complications in transplantation Carry out during the testing before transplantation , in the diagnosis of certain autoimmune diseases and in determination of paternity HLA typing • Serotyping • genotyping