Neuro LABS
advertisement

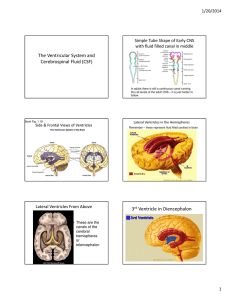
Neurology Labs Brenda Beckett, PA-C Clinical Assessment II Cerebrospinal Fluid (CSF) Clear fluid that occupies subarachnoid space and ventricles Produced in the choroid plexus Obtained by lumbar puncture (L3-L4) Usually: clear, colorless, acellular, sterile Traumatic tap Cerebrospinal Fluid WBC, RBC Protein Glucose Culture Other tests (see table p 307-313 Wallach) Multiple Sclerosis CSF IgG, nonspecific marker (also elevated in: neurosyphilis, GuillanBarre, head trauma, leukemia, etc) Measure CSF and serum IgG and albumin. (to determine increased production in CNS vs crossing bb barrier) Multiple Sclerosis CSF IgG Index. Compares ratio of CSF IgG: albumin to serum IgG:albumin ratio. Multiple Sclerosis Oligoclonal proteins (or bands)- shows discrete bands on electrophoresis. – Perform on CSF and serum – MS will show +CSF, neg serum myelin basic protein (MBP) may be observed during active demyelinization. – Perform on CSF – Used to monitor therapy Myasthenia Gravis Acetylchoine receptor (AChR) antibodies (3 different Ab:binding, blocking, modulating). Positive in >85% of pts with generalized sx, 50% of pts with occular sx. Also check thyroid function. At risk for other autoimmune diseases. Therapeutic Drug Monitoring (TDM) • • • Measures the level of some drugs as a way to determine the most effective dose or to avoid toxicity. Most drugs do not need to be monitored this way. Monitor drugs that have: narrow therapeutic window, toxic side effects. TDM Therapeutic range: Concentration where the drug has been shown to be efficacious without causing toxic effects in most people. Drug Category Drugs in that Category Treatment Use Cardiac drugs Digoxin, quinidine, procainamide, N-acetyl-procainamide (a metabolite of procainamide) CHF, angina, arrhythmias Antibiotics Aminoglycosides (gentamicin, tobramycin, amikacin),Vancomycin, Chloramphenicol Infections with bacteria that are resistant to less toxic antibiotics Drug Category Drugs in that Category Treatment Use Antiepileptics Phenobarbital, Epilepsy, phenytoin, valproic acid, prevention of carbamazepine, seizures ethosuximide, gabapentin, lamotrigine Bronchodilators Theophylline, caffeine Immunosuppressants Cyclosporine, Prevent tacrolimus, sirolimus, rejection of mycophenolate mofetile transplanted organs Asthma, COPD, neonatal apnea Drug Category Drugs in that Category Treatment Use Anti-cancer drugs Methotrexate Cancers, rheumatoid arthritis, non-hodgkin's lymphomas, osteosarcoma, psoriasis Psychiatric drugs Lithium, desipramine, some antidepressants (imipramine, amitriptyline, nortriptyline, doxepin) bipolar disorder, depression TDM Specimen collection time in relation to dose is important. – Sampling time is most frequent error Trough vs peak – Most are drawn as trough, except some antibiotics Steady state – After multiple doses Case Study History and presentation: 33yo female, admitted for sudden, bilat loss of vision. 1yr ago, had difficulty walking, improved w/i 2wks. Occ tingling and “electrical” sensation down her back with flexed neck. Occ difficulty expressing herself verbally. Case Study Physical exam: A&O, mild distress, speech normal No light perception bilat, EOMI. No nystagmus, Pupils sluggishly reactive to light. Paraparesis with spacicity and dissociated sensory loss in LE. Sensory level at T7. Brisk patellar DTRs and bilat +Babinski’s Remainder of PE unremarkable Case Study What is your differential diagnosis? What lab testing do you want to perform? Case Study What additional CSF test(s) would you like to order? Results: Case Study - What is your diagnosis?