Pulmonary thromboembolism
advertisement

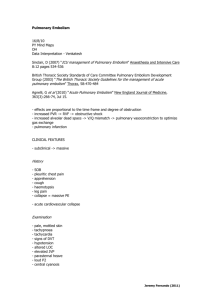
Pulmonary Thromboembolism Prevention, Diagnosis, Management Alex Yartsev (October 2010) Embolism? • Something obstructing the vessel • Piece of fat • Piece of tissue • Bubble of gas …CLOT • Venous thromboembolism: DVT and PE Aetiology: Where are these clots coming from? • • • • • Deep veins of lower limbs Pelvic veins Inferior vena cava Occasionally, deep veins of upper limbs Rarely, tips of central lines Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Aetiology: why are these clots forming? • Virchow’s Triad • Immobility • Hypercoagulability • Vessel wall injury Virchow RLK (1856). "Thrombose und Embolie. Gefässentzündung und septische Infektion". Gesammelte Abhandlungen zur wissenschaftlichen Medicin. Frankfurt am Main: Von Meidinger & Sohn. pp. 219–732. Risk factors: immobility Post operative immobility – – – – – – Hip Fracture, or hip replacement Knee replacement Major Trauma Spinal cord injury Major general surgery eg. laparotomy arthroscopic surgery OR > 10 Immobility due to pathology – Paralytic stroke OR 2-9 Immobility due to circumstance – Bed rest > 3 days – Sitting immobility (air travel, movie marathon) – Obesity OR 1-2 Anderson F, Spencer F; Risk Factors for Venus Thromboembolism; Circulation 2003;107;I-9-I-16 *OR: Odds ratio, a measure of effect size; ratio of odds of one event to the odds of another event Risk factors: Hypercoagulability Hormone replacement therapy Oral contraceptive therapy Chemotherapy Malignancy Pregnancy: postpartum Inherited thrombophilia Pregnancy: antepartum Increasing age (>40) OR 2-9 OR 1-2 Though risk increases for every decade over 40 Anderson F, Spencer F; Risk Factors for Venus Thromboembolism; Circulation 2003;107;I-9-I-16 *OR: Odds ratio, a measure of effect size; ratio of odds of one event to the odds of another event Risk factors: Vessel wall abnormality Central venous lines Previous DVT / VTE Varicose veins OR 2-9 OR 1-2 Anderson F, Spencer F; Risk Factors for Venus Thromboembolism; Circulation 2003;107;I-9-I-16 *OR: Odds ratio, a measure of effect size; ratio of odds of one event to the odds of another event Epidemiology • 1 in 1000 in general population • Variable in critical care. – From 0.4% to 8.3%, depending on who you talk to • Up to 40% of pts with DVT will develop PE • Up to 5% of pts with PE devlop pulmonary hypertension Patel R., et al Burden of Illness in venous ThromboEmbolism in Critical care: a multicenter observational study J Crit Care Volume 20, Issue 4, Pages 341-347 Muscedere J, et. al., Venous thromboembolism in critical illness in a community intensive care uni, J Crit Care Volume 22 Issue 4 Pages 285-289 Rocha AT Tapson VF Venous thromboembolism in intensive care patients. Clin Chest Med. 2003 Mar;24(1):103-22. Prophylaxis - Everyone should get heparin or clexane - Everyone should get TEDs or calf compressors - Everyone should be mobilized early - Aspirin can be used, but is less efficacious Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Geerts et. al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):338S-400S. Symptoms • • • • Dyspnoea Syncope Pleuritic chest pain Hemoptysis – Most patients will have at least one – Chest pain and hemoptysis is a late sign (pulmonary infarction) Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Signs ….Frequently, no signs! • Tachypnea (most common) • Tachycardia • Fever • Signs of right ventricular dysfunction HUGE PE: - Hypotension - Cyanosis - Mottled skin Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Xray Findings • Focal oligaemia: reduced vascular markings • Peripheral wedge-shaped density • Enlarged left descending pulmonary artery Or more likely, and less specific… • Cardiac enlargement • Elevated hemidiaphragm • Atelectasis ECG Findings • Normal in 1/3rd • • • • • Sinus tachy Non specific STD / TWI in anterior leads (right heart strain) Right axis deviation RBBB Classic S1 Q3 T3 : – Deep S wave in lead I – Q wave and inverted T wave in lead III Bloods - Troponin may be raised A-a gap may be increased CO2 may be low Metabolic acidosis may be present Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Specific investigations - D-Dimer: - Fibrin degradation product Comes from any fibrin, anywhere Normal = highly unlikely there is VTE Abnormal = could mean anything Elevated in MI, malignancy, trauma, infection, DIC, heart failure Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Specific investigations - CTPA: - For large PE, very accurate; less so for small PE - Added bonus: compares RV:LV size ratio Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Specific investigations - Ventilation-perfusion (V/Q ) scanning - Low probability does not satisfactorily exclude PE Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Specific investigations - ECHO - RV wall hypomotility, RV + RA dilatation - Sometimes, you can visualize the thrombus Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Investigation Algorithm Stable patient Unstable patient Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Investigation Algorithm Stable patient CTPA or V/Q scan Unstable patient Transthoracic Echo Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Severity Stratification Stable patient CTPA or V/Q scan Little segmental defects Large defects, dilated RV, visible PA clot Unstable patient Transthoracic Echo RV dysfunction Visible RV or PA thrombus Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Management according to severity Stable patient CTPA or V/Q scan Little segmental defects Anticoagulate ..or IVC filter Large defects, dilated RV, visible PA clot Unstable patient Transthoracic Echo RV dysfunction Anticoagulate if there is no RV failure, Thrombolyse if RV is dysfunctional Visible RV or PA thrombus Thrombolysis Embolectomy Anticoagulation Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Management according to severity -Small PE, no RV dysfunction: - anticoagulation only -Submassive PE, RV dysfunction but hemodynamically stable: -Strongly consider thrombolysis -Also anticoagulate - MASSIVE PE: - remove the thrombus somehow, either by embolectomy or by thrombolysis Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed ANTICOAGULATION: with what? - HEPARIN: clexane as effective and safe as unfractionated - UNFRACTIONATED for post-embolectomy or postthrombolysis, as it can be reversed quickly with protamine The key is to achieve therapeutic levels quickly: subtherapeutic levels increase risk of recurrence Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Segal JB et al., Management of venous thromboembolism: a systematic review for a practice guideline Ann Int Med 2007; 146: 211-222 Inferior Vena Cava Filter - If anticoagulation is contraindicated - If there have been RECURRENT PE while the patient is already anticoagulated - Some newer ones are easily retrieved - Improve 90 day mortality Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Kucher N. et al, Massive pulmonary embolism Circulation 2006; 1113: 577-82 Thrombolysis - Hopefully, produces massive immediate improvement in hemodynamic parameters - The bigger the PE, the more useful the thrombolysis - Randomized studies: no difference in mortality - In submassive PE: reduce escalation of treatment - In summary: - Always useful in massive PE - In submassive PE, useful if there is RV dysfunction - Unlike MI, these are useful with 14 days of onset! Complications: 10% will hemorrhage; 0.5% into the brain. Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Konstantinides et.al, Association between thrombolytic treatment and the prognosis of hemodynamically stable patients with major pulmonary embolism Circulation 1997; 96: 882-8 Wan S et. al, Thrombolysis compared with heparin for the initial treatment of pulmonary embolism: a meta-analysis of randomized controlled trials. Circulation 2004 110: 744-9 Embolectomy - Perioperative mortality 25-50% (as low as 7%-18% in some studies) Percutaneous embolectomy: mortality still 20-30% - Few studies comparing embolectomy and thrombolysis - Indications: Friedrich Trendelenburg - Thrombolysis is contraindicated, or has failed - Free-floating cardiac thrombus - Massive PE with shock Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Supportive measures - GIVE THEM OXYGEN. - Be cautious with fluids: too much will worsen RV function - Elevate MAP while working to drop pulmonary and right ventricular pressures Use norad to increase coronary perfusion pressure - ECMO/IABP Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Unusual measures - Selective pulmonary vasodilators: - Inhaled nitric oxide - Inhaled prostacycline - Limited supporting evidence, or animal studies Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Capellier G,Jacques T, Balvay P, et al: Inhaled nitric oxide in patients with pulmonary embolism. Intensive Care Med 1997;23:1089-1092 Webb SAR, Stott S, van Heerden PV: The use of inhaled aerosolized prostacyclin (IAP) in the treatment of pulmonary hypertension secondary to pulmonary embolism. Intensive Care Med 1996 , 22:353-355 No questions, please. References • • • • • • • • • • • • • • Bahloul M, Chaari A, Kallel H, Abid L, Hamida C, Dammak H, Rekik N, Mnif J, Chelly H, Bouaziz M. Pulmonary embolism in intensive care unit: Predictive factors, clinical manifestations and outcome. Ann Thorac Med 2010;5:97-103 Agnelli G,Becattini C, Acute Pulmonary Embolism N Engl J Med 2010;363:266-74. Davies A, Pilcher D; Pulmonary Embolism (ch. 30) cit. Oh’s Intensive Care Manual 6th ed Virchow RLK (1856). "Thrombose und Embolie. Gefässentzündung und septische Infektion". Gesammelte Abhandlungen zur wissenschaftlichen Medicin. Frankfurt am Main: Von Meidinger & Sohn. pp. 219–732. Cohen AT, et al for the ENDORSE Investigators. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study). Lancet 2008; 371: 387—94. Heit et al; Risk Factors for Deep Vein Thrombosis and Pulmonary Embolism Arch Intern Med. 2000;160:809-815. Anderson F, Spencer F; Risk Factors for Venus Thromboembolism; Circulation 2003;107;I-9-I-16 Patel R., et al Venous thromboembolism in critically ill patients: incidence and risk factors Critical Care 2007, 11(Suppl 2):P363 Muscedere J, et. al., Venous thromboembolism in critical illness in a community intensive care uni, J Crit Care Volume 22 Issue 4 Pages 285-289 Segal JB et al., Management of venous thromboembolism: a systematic review for a practice guideline Ann Int Med 2007; 146: 211-222 Kucher N. et al, Massive pulmonary embolism Circulation 2006; 1113: 577-82 Konstantinides et.al, Association between thrombolytic treatment and the prognosis of hemodynamically stable patients with major pulmonary embolism Circulation 1997; 96: 882-8 Wan S et. al, Thrombolysis compared with heparin for the initial treatment of pulmonary embolism: a metaanalysis of randomized controlled trials. Circulation 2004 110: 744-9 Geerts et. al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004 Sep;126(3 Suppl):338S-400S.