BIOS 2310 lecture 4 Joints students
advertisement

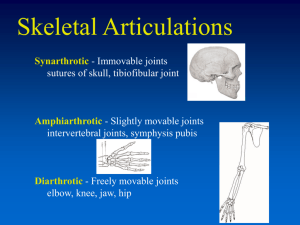
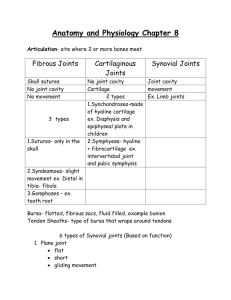
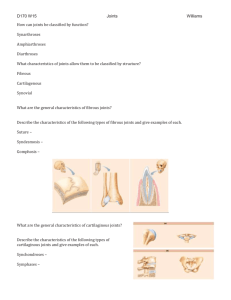
Articulations!! (the Joints) Section 1: Joint Design and Movement • Articulations (_____________________) – Where two bones interconnect – Bones are relatively inflexible so necessary to allow movement – Reflect compromise between need for strength versus need for ______________________ – Anatomical structure of each joint determines type and amount of movement possible • Categories from range of motion and subgroups from anatomical structure Joint types • No Movement – Have we seen this before? • Limited Movement – Can you think of any? • Free Movement – Examples? Joint Design and Movement • Three functional categories 1. 2. 3. – _______________________ (no movement) Amphiarthrosis (little movement) ____________________________ (free movement) Synarthrotic and amphiarthrotic joints • • – Relatively simple structure Direct connections between bones Diarthrotic joints • • Complex in structure Permit greatest range of motion Synovial joints • Components of synovial joints – ___________________ cartilages • Resemble hyaline cartilages – Matrix contains more water comparatively • Have no perichondrium • Slick and smooth, so reduce friction • Are separated by thin film of synovial fluid Articular Cartilage Components of synovial joints (continued) – ______________ fluid • Similar in texture to egg whites • Produced at the synovial membrane • Circulates from areolar tissue to joint cavity • Percolates through articular cartilages • Total quantity is less than 3 mL Synovial fluid Components of synovial joints (continued) – _________________ capsule • Dense and fibrous • May be reinforced with accessory structures (tendons and ligaments) • Continuous with periosteum of each bone Joint capsule Functions of synovial fluid – Lubrication • With articular cartilage compression, synovial fluid is squeezed out and reduces friction between moving surfaces – _______________________________ distribution • Provide nutrients and oxygen, as well as waste disposal for the chondrocytes of articular cartilages • Compression and reexpansion of articular cartilages pump synovial fluid in and out of cartilage matrix – ________________________ absorption • Distributes compression forces across articular surfaces and outward to joint capsule Joint Accessory – ____________________ (a pouch) • Small pocket filled with synovial fluid • Often form in areas where tendon or ligament rubs against other tissues • Reduce friction and act as shock absorbers Bursa Accessory structures in knee (continued) – Fat pads • Adipose tissue covered by synovial membrane • Protect articular cartilages • Act as packing material for joint – _____________________ (a crescent) • Pad of fibrous cartilage between bones of synovial joint • May subdivide joint cavity and affect fluid flow or allow variations in shapes of articular surfaces Meniscus Fat pad • Accessory structures in knee – Tendons of quadriceps • Pass across joint – Limit movement – Provide mechanical support • Accessory ligaments • __________________, strengthen, and reinforce joint • Intrinsic ligaments – Localized thickening of joint capsule – Example: cruciate liagments of knee • ___________________ ligaments – Separate from joint capsule – May pass inside (intracapsular) or outside (extracapsular) the joint capsule – Intracapsular example: cruciate ligaments – Extracapsular example: patellar ligament Synovial joints • _________________ vs. strength in joints – Greater range of motion = ______________ joint • Examples: – Synarthrosis (strongest type of joint, no movement) – Diarthrosis (far weaker but broad range of motion) – _____________________________ (luxation) • • • • Movement beyond normal range of motion Articulating surfaces forced out of position Can damage joint structures No pain from inside joint but from nerves or surrounding structures Types of motion and structural types of synovial joints – _____________________ • – Movement along two axes in one plane Angular motion • – Movement along two axes in one plane with additional change in angle ______________________ – – – Special complex angular movement Proximal end of bone remains fixed while distal end can move in a circle (“trace circumference”) Rotation • Bone ends remain fixed and shaft rotates The anatomical types of synovial joints, with joint models and examples Types of Synovial Joints Models of Joint Motion Gliding joint Examples • Acromioclavicular and claviculosternal joints • Intercarpal and intertarsal joints • Vertebrocostal joints • Sacro-iliac joints Manubrium Hinge joint Humerus • Elbow joints • Knee joints • Ankle joints • Interphalangeal joints Ulna Pivot joint Atlas • Atlas/axis • Proximal radio-ulnar joints Axis Ellipsoid joint Scaphoid bone Radius • Radiocarpal joints • Metacarpophalangeal joints 2–5 • Metatarsophalangeal joints Ulna Saddle joint • First carpometacarpal joints Metacarpal bone of thumb Trapezium Ball-and-socket joint Scapula • Shoulder joints • Hip joints Humerus Figure 8.2 6 • Flexion and extension – – • Usually applied to movements of long bones of limbs but also axial skeleton _____________________ _ Anterior/posterior movement that reduces angle between articulating elements – – – Lateral flexion » Vertebral column bending to the side Dorsiflexion » Flexion at ankle joint and elevation of sole ___________________ flexion (planta, sole) » Extension at ankle joint and elevation of heel – Extension • Anterior/posterior movement that increases angle between articulating elements – __________________ » Extension past anatomical position • Abduction and Adduction – Always refers to movements of appendicular skeleton, not axial Movements are usually toward or away from body midline – • – For fingers or toes, movements are spreading digits apart or bringing them together ____________________ (ab, from) • – Movement away from body longitudinal axis in frontal plane ____________________ (ad, to) • Movement toward body longitudinal axis in frontal plane • Circumduction – Moving arm or thigh as if to draw a big _________________ at distal end of limb • Wrist • Arm • Rotation – When applied to the trunk, described as left and right _____________________ When applied to limbs – • Medial rotation (internal or inward rotation) – • Anterior surface of limb toward trunk long axis Lateral rotation (external or outward rotation) – Anterior surface of limb away from trunk long axis • Rotation (continued) – Other special terms for rotation of forearm • ____________________ – – – • Proximal end of radius rotates near ulna Distal end rolls across anterior ulnar surface Turns the wrist and hand from palm facing front to palm facing back ____________________ – – Opposing movement Palm is turned anteriorly • Special movements – _______________________ • – Movement of thumb toward palm surface or other fingers Protraction • – Movement forward in anterior plane ___________________ • – Reverse of protraction Inversion (in, into + vertere, to turn) • – Twisting foot motion to turn sole inward ________________________ (e, out) • Opposing movement to inversion Special movements Opposition Eversion Retraction Protraction Inversion Depression Elevation Figure 8.4 2 Articulations • ____________________skeleton articulations – Typically are strong but very little movement • ___________________________ skeleton articulations – Typically have extensive range of motion – Often weaker than axial articulations Joints of the Axial Skeleton Sutures of the skull Temporomandibular joint (temporal bone and mandible) Atlanto-occipital joint (occipital bone and atlas) and the atlanto-axial joint (C1–C2) Joints of the thoracic cage Intervertebral joints The lumbosacral joint, which attaches the last lumbar vertebra to the sacrum The sacrococcygeal and intercoccygeal joints, which structurally resemble simplified intervertebral joints Figure 8 Section 2 1 Joints of the Appendicular Skeleton The sternoclavicular joint, the only articulation between the axial skeleton and the pectoral girdle and upper limb Shoulder joint The sacro-iliac joint, which firmly attaches the sacrum of the axial skeleton to the pelvic girdle of the appendicular skeleton Elbow joint Superior and inferior radio-ulnar joints Pubic symphysis Wrist joint Joints of the hand and fingers Hip joint Knee joint Ankle joint Joints of the foot and toes Figure 8 Section 2 2 • Vertebral articulations – Between superior and inferior articular processes of adjacent vertebrae • Gliding ______________________________ joints – Permit flexion and rotation – Adjacent vertebral bodies form symphyseal joints with _______________________________ discs – Numerous ligaments attach bodies and processes of vertebrae to stabilize column • Intervertebral discs – Composition • __________________________ fibrosis – Tough outer layer of fibrous cartilage – Collagen fibers attach to adjacent vertebrae • ___________________ pulposus – Soft, elastic, gelatinous core – Provides resiliency and shock absorption – Account for ¼ length of vertebral column • Water loss from discs causes shortening of vertebral column with age and increases risk of disc injury The ligaments attached to the bodies and processes of all vertebrae Primary Vertebral Ligaments Ligamentum flavum Intervertebral disc Anulus fibrosus Posterior longitudinal ligament Nucleus pulposus Spinal cord Interspinous ligament Spinal nerve Supraspinous ligament Posterior longitudinal ligament Anterior longitudinal ligament Lateral view Sectional view Figure 8.5 2 • Primary vertebral ligaments – Ligamentum ______________________ • Connects adjacent vertebral laminae – Posterior longitudinal ligament • Connects posterior surfaces of adjacent vertebral bodies – Interspinous ligament • Connects spinous processes of adjacent vertebrae – Supraspinous ligament • Connects spinous processes from sacrum to C7 – Ligamentum nuchae from C7 to base of skull – _______________________________ longitudinal ligament • Connects anterior surfaces of adjacent vertebral bodies • Disorders of vertebral column – _______________________ disc • Posterior longitudinal ligaments weaken causing more pressure on discs • Nucleus pulposus compresses, distorts anulus fibrosus • Disc bulges into vertebral canal (doesn’t actually slip) – ________________________ disc • Nucleus pulposus breaks through anulus fibrosus • Spinal nerves are often affected • Disorders of vertebral column (continued) – ______________________ (penia, lacking) • Inadequate ossification leading to loss of bone mass • Often occurs with age beginning between ages 30 and 40 • More severe in women than men • Osteoporosis (porosus, porous) – Bone loss sufficient to affect normal function The effects of osteoporosis on spongy bone Clinical scan of a compression fracture in a lumbar vertebra Figure 8.5 5 The effects of osteoporosis on spongy bone Normal spongy bone SEM x 25 Spongy bone with osteoporosis SEM x 21 Figure 8.5 5 Ball and Socket • Shoulder joint (glenohumeral joint) – __________________ range of motion of any joint Most frequently dislocated joint – • • – Demonstrates stability sacrificed for mobility Most stability provided by surrounding skeletal muscles, associated tendons, and various ligaments Ball-and-socket diarthrosis • Formed by head of humerus and glenoid cavity of scapula • Hip joint – Sturdy ball-and-socket joint • – – Although not directly aligned with weight distribution along femur shaft, which can produce fractures of femoral neck or intertrochanteric region Permits _______________, extension, adduction, abduction, circumduction, and rotation Formed by head of femur and acetabulum of hip bone The ligaments of the hip joint Reinforcing Ligaments Pubofemoral ligament Iliofemoral ligament Ischiofemoral ligament Greater trochanter Ischial tuberosity Posterior view Intertrochanteric line Lesser trochanter The ligaments of the hip joint in posterior view Anterior view The ligaments of the hip joint in anterior view Figure 8.6 5 Hinge • Elbow joint – Complex __________________ joint involving humerus, radius, and ulna Extremely strong and stable due to: – 1. 2. 3. – • – Bony surfaces of humerus and ulna interlock Single, thick articular capsule surrounds both humero-ulnar and proximal radio-ulnar joints Articular capsule reinforced by strong ligaments Severe stresses can still produce dislocations or other injuries Example: ___________________ elbow Muscles flexing elbow attach on anterior while those extending attach on the posterior The elbow joint Humerus Posterior view Olecranon fossa Humeroulnar joint Ulna Olecranon Figure 8.7 1 Elbow and knee joints • Elbow joint (continued) – Specific joints of the elbow • _____________________joint – • Humero-ulnar joint – – – – • Capitulum of humerus articulating with head of radius Largest and strongest articulation Trochlea of humerus articulates with trochlear notch of ulna Shape of ulnar notch determines plane of movement Shapes of olecranon fossa and olecranon limit degree of extension Proximal radio-ulnar joint is ___________part of elbow joint Elbow and knee joints • Elbow joint (continued) – Reinforcing ligaments • Radial _________________ ligament – • Ulnar collateral ligament – • Stabilizes lateral surface of joint Stabilizes medial surface of joint ____________________ ligament – Binds head of radius to ulna Elbow and knee joints • Knee joint – Contains _____________separate articulations 1. 2. 3. – Medial condyle of tibia to medial condyle of femur Lateral condyle of tibia to lateral condyle of femur Patella and patellar surface of femur Permits flexion, extension, and very limited _______________ Elbow and knee joints • Knee joint (continued) – External support • Quadriceps tendon to patella – • Fibular collateral ligament – • Medial support _________________________ligaments – • Lateral support Tibial collateral ligament – • Continues as patellar ligament to anterior tibia Posterior support extending between femur and heads of tibia and fibula Tendons of several muscles that attach to femur and tibia Elbow and knee joints • Knee joint (continued) – Internal support • ___________________ ligaments limit anterior/posterior movement of femur and maintain alignment of condyles – – Anterior cruciate ligament (ACL) » At full extension, knee becomes “locked” (slight lateral rotation tightens ACL, and lateral meniscus forced between tibia and femur) » Opposite motion to “unlock” Posterior cruciate ligament (PCL) Elbow and knee joints • Knee joint (continued) – Internal support (continued) • Medial and lateral _______________ – – Fibrous cartilage pads between tibial and femoral condyles Act as cushions and provide lateral stability to joint Disruption to normal joint function • Arthritis – Damage to articular cartilages but specific cause varies • • – Exposed surfaces change from slick, smooth-gliding to rough feltwork of collagen fibers increasing friction Rheumatism (pain and stiffness affecting the skeletal and/or muscular systems) is often a symptom Osteoarthritis • • Also known as degenerative arthritis or degenerative joint disease Generally affects individuals age 60 and older – • 25% of women, 15% of men Can result from cumulative wear and tear of joints or genetic factors affecting collagen formation Comparisons of normal articular cartilage with articular cartilage damaged by osteoarthritis Arthritic Joint Normal Joint Fibrous remains of the articular cartilage Articular cartilage Degenerating articular cartilage LM x 180 Arthroscopic view of normal cartilage LM x 180 Arthroscopic view of damaged cartilage Figure 8.8 1 – 2 Disruption to normal joint function • Visualizing problematic joints – Arthroscopic surgery • • Optical fibers (arthroscope) inserted into joint through small incision without major surgery to visualize joint interior If necessary, other instruments can be inserted through other incisions to permit surgery within view of arthroscope – _____________________ resonance imaging • Cost-effective and noninvasive viewing technique that allows examination of soft tissues around joint as well An arthroscopic view of the interior of the left knee, showing injuries to the anterior and posterior cruciate ligaments. PCL Femoral condyle ACL Meniscus Figure 8.8 3 Figure 8.8 4 Disruption to normal joint function • _____________________ joints – May be last resort if other solutions (exercise, physical therapy, drugs) for joint problems fail – Not as strong as natural joints, so most suitable for elderly – Typically have service life of about 10 years Figure 8.8 5 Next Monday • Exam: Framework • Start new section: Organization!