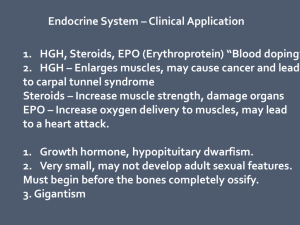
Blood Glucose Levels
advertisement

Be The Pancreas Caring for the Patient with Diabetes Millions of People USA’s Growing Population with Diabetes Data from the National Diabetes Statistics Report, 2014 (released June 10, 2014) - See more at: http://www.diabetes.org/diabetes-basics/statistics/#sthash.dC2iwT48.dpuf Why Nursing is Vital & Well-Positioned to Help Provide Good Diabetes Care • Nursing sees the whole picture & plays many roles in patient care e.g, travel off unit, physical therapy, X-ray Amount of food eaten (carbs) or NPO status Patient’s day to day concerns Order changes (by various providers) Observer of changes in symptoms Nursing does most (if not all) of the patient education Diabetes in the Acute Care Setting Basics – Review of Pathophysiology Prevention/Treatment 1. 2. I. II. 3. 4. 5. 6. Lifestyle Modifications Insulin & Oral Agents Hypo/Hyperglycemia Review The Complications Inpatient Diabetes Care/Patient Education Case Studies The Basics Review of the Pathophysiology of Diabetes Basics Energy Balance – Insulin Production It All Starts with the Eyes & Nose Anyone Hungry??? Basics Energy Balance – Insulin Production Bloom S et al. Hormonal regulation of food intake. Physiol Rev 2005;85(4):1131-58. Basics Blood Glucose Regulation Basics Insulin Production Basics Insulin Uptake into the Cells Harvard Health Publications Basics-The Body’s Response to Efficient Circulating Insulin Hyperglycemia Liver Muscle Glucose storage Glucose uptake for energy Adipose tissue Glucose uptake Stored as fat Euglycemia Basics-The Body’s Response to Little or No Circulating Insulin Hyperglycemia Liver Defective Glucose storage Muscle Defective Glucose uptake for energy Defective Glucose uptake ↑ ↑ ↑ Hyperglycemia Basics Definition of Diabetes Mellitus Diabetes mellitus is a group of metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both. The chronic hyperglycemia of diabetes is associated with long-term damage, dysfunction, and failure of various organs, especially the eyes, kidneys, nerves, heart, and blood vessels. Basics – The Numbers & Targets Normal fasting glucose FPG <100 mg/dl (5.6 mmol/l) Impaired fasting glucose (IFG) or “Pre-Diabetes” FPG 100–125 mg/dl (5.6–6.9 mmol/l) or A1c 5.7-6.4% Diabetes (with A1c or OGTT) FPG ≥126 mg/dl (7.0 mmol/l) or A1c >6.5% Targets*: Critical Care 140-180 mg/dL Non-critical care pre-meal <140 mg/dL Non-critical care random <180 mg/dL Outpatient: A1c <7%; 80-130 mg/dL for most patients; individualize to patient health state *ADA Standards of Medical Care in Diabetes – 2015 Basics – Glycated Hemoglobin or HbA1c An HbA1c or “A1c” test is the measure of the average blood glucose over the past 2-3 months. When BG are high, glucose molecules attach to the hemoglobin in RBCs. The longer hyperglycemia occurs, the more glucose binds to the RBC & the higher the A1c. “Average Glucose” Explaining & Communicating an A1c* A1C (%) Average Blood Glucose Without Diabetes <5.7 70-99 At Risk for Developing Diabetes (sometimes referred to as “pre-diabetes”) 5.7-6.4 100-125 For Those Diagnosed with Diabetes Good Control American Diabetes Association Target <7% Sub-Optimal Control Action Needed to Improve Control >8%* *An A1C goal of 8% may be set for a pt with poor prognosis or frequent occurrences of hypoglycemia Very Poor Control Immediate Action Needed to Improve Control >9% 6 126 7 154 8 183 9 212 10 240 11 269 12 298 13 326 Basics – Diabetes Types Key characteristics of type 1, LADA (latent autoimmune DM in adults), & T2DM. Type 1 DM LADA (Type 1.5) Type 2 DM Typical age of onset Youth or Adult Adult Progression to insulin dependence Rapid Latent (days/weeks) (mos/years) Slow (years) Presence of autoantibodies* Insulin dependence Yes Yes No At diagnosis Within 6 years Over time, if at all Insulin resistance No Some Yes Adult *Proteins that indicate the body has launched an autoimmune attack on the insulin-producing beta cells in the pancreas. Basics – Type 1 Diabetes (T1DM) Characterized by labile glycemic control; sensitivity to both insulin & glucose Associated with microvascular and macrovascular complications Generally arises from an autoimmune process that destroys the pancreatic β-cells Reduced or absent glucagon release Basics – T1DM Treatment Before/After Discovery of Insulin Elizabeth Hughes, 1918 (left), age 11, during starvation therapy. Elizabeth Hughes, 1921 (right) age 14 after start of insulin therapy. She lived until 1981; outlived her T1DM life expectancy by 60 years. Basics – What is Insulin Sensitivity? Insulin sensitivity is a term used to describe people who require relatively normal or low levels of insulin to process glucose. A person who is insulin-sensitive needs only a relatively small amount of insulin to keep blood glucose levels in the normal range and to keep the body’s cells supplied with the glucose they need. T1DM & s/p total pancreatectomy patients are usually insulin sensitive Basics – Type 2 Diabetes (T2DM) Characterized by chronic hyperglycemia; insulin resistance Associated with microvascular and macrovascular complications Generally arises from a combination of defective insulin uptake and -cell dysfunction Basics – What is Insulin Resistance? Opposite of insulin sensitive, an insulin resistant patient needs much more insulin to achieve the same BG lowering effects. Major defect in individuals with T2DM Reduced biological response to insulin (will require larger doses of insulin than T1DM) Strong predictor of T2DM Closely associated with obesity, especially visceral adiposity IR Basics – Insulin Resistance Reduced Response to Circulating Insulin Insulin resistance Liver Glucose output IR Adipose tissue Muscle Glucose uptake Glucose uptake Hyperglycemia Basics – What is -cell dysfunction? Major defect in individuals with type 2 diabetes (inherited) Reduced ability of -cells to secrete insulin in response to hyperglycemia over time Prevention/Treatment Lifestyle Modifications Prevention/Treatment Changing Behaviors Healthy Eating Activity Healthy Coping/Stress Management R E L A P S E The Transtheoretical Model (Prochaska & DiClemente, 1983) Prevention/Treatment – Healthy Eating Moderate intake of carbohydrates (26-45% of daily calories come from carbohydrates) Men 3-4 servings or 45-60 grams per meal Women 2-3 servings or 30-45 grams per meal *Very low carb diets not endorsed (20-50g/day) Increase consumption of vegetables and fruits and low dairy products (DASH diet) Reduce saturated fat, cholesterol and trans fat intake (but not fat free) Reduce sodium intake Moderate intake of alcohol ADA, 2015 Prevention/Treatment – Activity Children with diabetes or prediabetes – 60 minutes of physical activity daily Adults with diabetes or prediabetes – 150 min/week of moderate-intensity aerobic physical ativity (50-70 of maximum heart rate) spread over at least 3 days/week with no more than 2 consecutive days without exercise Adults with T2DM – twice weekly resistance training Prevention/Treatment – Activity Evidence supports that ALL individuals, diabetes or not, should reduce sedentary time, break up extended time (>90 min.) spent sitting ADA, 2015 Prevention/Treatment – Healthy Coping Short term stress response Impact of counter-regulatory hormones: epinephrine & noepinephrine Glycogen broken down into glucose, raising blood glucose Increased blood pressure Increased breathing rate Increased metabolic rate Chang in blood flow patterns, leading to increased alertness, decreased digestion & renal activity Long-term stress response Effects of glucocorticoids/ cortisol: Proteins and fats broken down into glucose, leading to increase blood glucose Effects of mineralocorticoids: Retention of sodium ions & water by the kidney Increased blood volume & pressure Prevention/Treatment – Healthy Coping Recognize stress, know your triggers and understand it can be managed. Learning/Practicing healthy techniques that help you cope. (quiet time, exercise, music, reading, talking with supportive friend) Prevention/Treatment – Healthy Coping Setting realistic expectations & promoting healthy coping behaviors Setting realistic goals (think what we sometimes as our patients to do) Reasonable schedules Regular exercise Appropriate assertiveness Eating Healthy Getting enough sleep Avoiding unhealthy behaviors Breathe…. Frydenberg, E.Thriving, Surviving, or Going Under: Coping with Everyday Lives, Information Age, 2004 How to combat insulin resistance? Loss of body fat Exercise Good blood glucose control Stress management Adequate sleep Food choices-moderation, reduced carbohydrate intake IR Treatment with Diabetes Medications Treating with Insulin Insulin Onset of Action Peak Duration of Action Comments Rapid Acting Analogs: lispro, Humalog® aspart, Novolog® glulisine, Apidra® 5-15 min. 30-90 min. 3 to 5 hours For nutritional & correction coverage Short Acting: Regular, Humulin R® Regular, Novoloin R® 30 min. 2 to 4 hours 5 to 8 hours For nutritional & correction coverage Long-Acting Analogs: glargine, Lantus® detemir, Levemir® 1-2 hours Peakless 20-26 hours Given daily or split twice daily for basal needs Intermediate Acting: NPH, Humulin N® NPH, Novolin N® 1-3 hours 8 hours 12-16 hours Given twice daily for basal needs Mixed Insulin: Humulin/Novolin 70/30® Humalog 50/50® Humalog 75/25® Novolog 70/30® 30 to 60 min. Varies 5 to 15 min. 10-16 hours Given twice daily for basal/nutritional needs. Must eat with mixed insulin intake. Treating with Insulin Insulin Onset of Action Peak Duration of Action Comments Inhaled Insulin: Afrezza® (insulin human) Inhalation Powder 5-15 min. 30-90 min. 3 to 5 hours For nutritional & correction coverage Humulin R U-500® 30 min. 2 to 4 hours Up to 24 hours 5x more concentrated than U-100 regular insulin. Used in patients requiring >200 units/ day. Dosed twice daily. peakless Up to 40 hours U300-Just received FDA approval. Next generation Lantus. Less hypoglycemia than glargine. Degludec – awaiting CV studies, 2015-106 marketing to start Ultra Long Acting Insulin: 1-2 hours Sanofi Aventis’ U300® degludec, Tresiba® Insulin response to blood glucose levels (no Diabetes) Insulin Effect 180mg/dL Blood Glucose Levels 99mg/dL 70mg/dL Breakfast Lunch Dinner Body releases insulin in response to actual glucose levels Body releases a small amount of insulin 24/7 to keep blood glucose stabilized. Basal-Nutritional Therapy -mimicking the body’s natural insulin response- Insulin Effect 180mg/dL Blood Glucose Levels 99mg/dL 70mg/dL Breakfast Lunch Dinner Rapid Acting Insulin Long Acting Insulin (i.e. lispro-Humalog) (i.e. glargine-Lantus) 3 Reasons to Administer Insulin for BG Control Always Ask Yourself “Why Am I Giving this Dose of Insulin”? Basal-long acting to suppress gluconeogenesis between meals or at night Nutritional/Bolus-rapid/fast acting to cover intake of carbs (e.g. meals, Tube Feeds) & prevent post-prandial/meal hyperglycemia Correction (sliding scale)-rapid/fast acting insulin to cover existing hyperglycemia Insulin on Board “Insulin on Board” simply refers to the amount of insulin still circulating in the bloodstream that may still be working. Be mindful of what patient has already received & how long it is acting Prevent Over-Reaction-watch BG trends! I I Insulin Stacking Remember “Insulin on Board” Stacking insulin refers to when a patient receives more insulin before the previous amount of insulin given has finished working. This creates even more onboard insulin. When insulin stacking can lead to serious episodes of hypoglycemia. Insulin Pump Therapy Insertion Set – holds delivery canula in place in the subcutaneous tissue Insulin Pump – preprogrammed technology that holds all basal, nutritional and correction coverage settings. Basal insulin delivered around the clock. Nutritional and correction boluses manually entered dependent on carbohydrate intake and blood glucose levels. Continuous Glucose Monitoring aka “Sensor” Sensor – held in place in the subcutaneous tissue Receiver – blood glucose levels wirelessly transmitted to receiver to give user blood glucose trends. CGM & insulin pump technology combined. Oral Antidiabetic Agents Oral Agents – Target Organs Oral Agents Drug Class Name How it Works Biguanides metformin – Glucophage®, glucophage XR®, Fortamet®, glumetza®, Metromin ER® Decreases liver glucose production and increases insulin sensitivity. Sulfonylureas* glimepiride/Amaryl® Longer-acting agents that glipizide/Glucotrol® & Glucotrol XL® increase insulin release glyburide/DiaBeta®/Micronase® from the pancreas. Thiazolidinediones (TZD) pioglitazone/Actos® Increases insulin sensitivity and decreases liver glucose production. Meglitinides* nateglinide/Starlix® repaglinide/Prandin® Short-acting agents that increase insulin release from the pancreas. *Watch for hypoglycemia especially if patient not eating/NPO Sutter Health. Diabetes Handbook, 2014 Oral Agents Drug Class Name How it Works Alpha-Glucosidase acarbose/Precose® Inhibitors miglitol/Glyset® Blocks carbohydrate digestion and absoprtion to help keep blood glucose levels normal after meals. DPP-4 Inhibitors sitagliptin/Januvia® saxagliptin/Onglyza® linagliptin/Tradjenta® alogliptin/Nesina® Stimulates the pancreas to respond better to glucose and decreases liver glucose production. SGLT-2 Inhibitors canagliflozin/Invokana® dapagliflozin/Farxiga® empagliflozin/Jardience® Decreases re-absorption of glucose in the kidneys. Sutter Health. Diabetes Handbook, 2014 Oral Antidiabetic Meds in Hospitalized Patients Most oral agents are optimized in outpatient settings. If a patient is NPO or eating very little in the wake of illness, oral agents may cause hypoglycemia. However, the stress of most illnesses can cause insulin resistance & worsen control with agents alone. Contrast dye: 48 hour post test hold of metformin Renal Failure: Contraindicated for metformin & SFU (e.g. glyburide) Where do we go from outpatient oral agents to inpatient insulin... Start with a Correction Scale! Other Injectables Drug Class Name How it Works GLP-1 Receptor Agonists exenatide/Byetta®/Bydureon® liraglutide/Victoza® Helps the pancreas make more insulin when blood glucose is high. Reduces glucose production in the liver and slows absorption of food. Amylin Analog pramlintide/Symlin® Reduces the amount of glucose made by the liver. Lowers blood glucose levels after meals and decreases appetite. Sutter Health. Diabetes Handbook, 2014 Diabetes Treatment Pitfalls in the Hospital Home medication plan dc’d & pt put on insulin scale only Pt not on CHO controlled diet RNs/NAs not accurately watching pt nutrition intake for pts on insulin or oral meds therapy MDs not changing insulin plans when hyper/hypoglycemic Large doses of long acting insulin given then pt made NPO (“overbasalization”) or TF stopped with large dose on board Pt hypoglycemia over treated resulting in rebound hyperglycemia Hypoglycemia & Hyperglycemia S/Sx Hypo- Hyperglycemia Hypoglycemia Shakiness, trembling Sweating (diaphoresis) Blurred vision Dizziness (feeling lightheaded) Cognitive impairment Feeling nervous or anxious Weakness Numbness, tingling of mouth and lips Tired Headache Sudden hunger Nauseous Rapid heart beat (tachycardia) Hyperglycemia Increased thirst (polydipsia) Increase in urination (polyuria) Urine may contain ketones Labored breathing Fatigue Increase in appetite (polyphagia), or decrease in appetite Headache, stomachache General aches and pain Changes in behavior or temperament Hypoglycemia Treatment “15/15 Rule” for mild hypoglycemia 15 grams of simple carbohydrate (CHO) ½ cup juice (PO) glucose tablets/gel (PO) ½ vial IV dextrose (NPO) glucagon (NPO) For BG <50mg/dL, give 30 grams simple CHO If next scheduled meal >1hour, give a snack Avoid Rebound HyperglycemiaDo not panic and over-treat mild hypoglycemia! Home Hypoglycemia Treatment “15/15 Rule” for mild hypoglycemia 15 grams of simple carbohydrate ½ cup juice or sweetened soda glucose tablets glucose gel 1 tablespoon sugar, honey or jam/jelly 8 ounces of nonfat or 1% milk 6 large jelly beans, 5 Life Savers, 15 Skittles or 4 Starburst glucagon – family member instruction for emergencies The Complications Diabetes Complications Short Term hypoglycemia DKA/HHS (Hyperglycemic Hyperosmolar State, aka HONK slow wound healing dehydration patients feel awful Chronic Complications Microvascular Disease Macrovascular Disease Complications of Hyperglycemia Leading cause of blindness Leading cause of renal failure 2/3 of DM have nerve damage >60% of amputations occur in diabetes patients Significant risk factor in birth defects and miscarriage Risk for heart disease and stroke 2-4x higher Microvascular Complications Nephropathy Retinopathy Autonomic & Peripheral Neuropathies 15 Retinopathy Nephropathy Neuropathies Microalbuminuria Relative Risk 13 11 9 7 5 3 1 6 7 8 9 10 HbA1c (%) Courtesy of Sanofi-Aventis 11 12 Macrovascular Complications Cardiovascular disease Cerebral vascular disease Peripheral vascular disease Inpatient Diabetes Care Patient Education The Patient on Glucocorticoids Therapy Impact On Glycemic Management: Increased insulin resistance Long-Acting insulin not a physiologic match for glucocorticoids Hyperglycemia worse in the postprandial phase (or post-CHO intake) Very important to start nutritional insulin when pt eating or on TF! Older Adults with Diabetes Reduced life expectancy High CVD burden Reduced GFR At Risk for Adverse Effects due to polypharmacy More likely to be compromised with hypoglycemia Individualize targets: Less ambitious blood glucose targets A1c 7.5-8% Focus on drug safety ADA/EASD Position Statement: Inzucchi, SE, et al. Diabetes Care. 2012; 35: 1364-1379 Inpatient Diabetes Care Keeping the Patients Safe Clarify, Clarify, Clarify-when in doubt, call for help! Notify Prescriber when hypoglycemia or hyperglycemia occurs Remember RN scope of practice with decision to give or hold insulin Don’t forget to involve the patient in diabetes treatment plan! Nursing Roles in Good Diabetes Care • Appropriate timing of point of care test (POCT), • • • • • • insulin administration & meal delivery Recognition of hyper/hypoglycemia & appropriate management/documentation Know when to hold insulin What to do when tube feeding is interrupted & pt has long acting insulin on board Appropriate patient hand off Patient self-management education Are they safe for discharge? Safe for Discharge • Does patient have a glucose monitor for home • • • • use? If not, know where to obtain one (e.g. hospital supplies, diabetes educator, pharmacy) Does patient know how to inject insulin and how to prevent and to treat hypoglycemia? Is patient clear about the diabetes plan after D/C? (e.g. medication plan) Does patient need more diabetes education? Does patient have appropriate outpatient F/U appointment with primary care or specialist? Diabetes Survival Skills Hospital setting is not ideal for learning but it may be the only chance we get! Survival skills Diabetes disease process Healthy eating basics Hypo/hyperglycemia prevention and treatment Medication use, frequency Drawing and injecting insulin Blood glucose monitoring Target blood glucose when to call MD Provide resources including OP education Tips for Diabetes Education for the Busy RN Provide instruction about insulin or oral diabetes agents and side effects when administrating doses Encourage patient to self – administer insulin Discuss impact of carbohydrates on blood glucose when meal tray present Use active listening skills and ask open questions to involve patient in self-care Write insulin doses on whiteboard or paper at bedside so patient understands insulin plan “Chunk & Check” Include education in end of shift hand off Case Studies: Practice Actual Events Case Study-Practice Basal-Nutritional-Correction Dosing Check BG qac, qhs & 0200 Basal: 20 units Lantus QHS Nutritional: 6 units of lispro (Humalog) QAC Correction Scale lispro QAC 70-100 101-150 151-200 201-250 251-300 301-350 >351 Correction 70-200 201-300 301-400 >400 -2 units (negative correction) No insulin +2 units +4 units +6 units +8 units +10 units call MD Scale lispro QHS No Insulin 2 units 4 units Call MD Case Study-Practice Basal-Nutritional-Correction Dosing 1. It is 0745, pt BG 209 mg/dL, pt will eat at 0800, How much insulin do you give at what time? 2. It is 1200, pt BG 185 mg/dL, pt is NPO for a 2pm test, How much insulin do you give at what time? 3. It is 1715, pt BG 85 mg/dL, pt will eat at 1730. How much insulin do you give at what time? 4. It is 2130, pt BG 143 mg/dL. Pt is ready for bed. How much insulin you give at what time? Case Study-Actual Events Insulin Stacking 38 yo M admitted from OSH for ascites Hx ESLD 2° to Hep C, ESRD, TIDM, blind, substance abuse & psych issues 0400 BG: 422 mg/dL –10 units lispro SC 0600 BG: 404 mg/dL –14 units lispro SC 0700 BG: 91 mg/dL 0800 BG: 18 mg/dL –D50 1 ½ ampules & ate 100% breakfast 0900 BG: 260 mg/dL, daily glargine (Lantus) 5 units given 1000 BG: 170 mg/dL Case Study-Actual Events Insulin Stacking What caused the BG to drop so quickly? What clues could the MD have looked for before prescribing STAT insulin doses? What clues could the RN have reviewed for before giving STAT insulin doses? Was an 1 ½ amp of D50 too much correction? Was it safe to give daily glargine (Lantus) dose? Case Study-Actual Events Hypoglycemia with Nutritional Insulin 67 yo M s/p heart transplant Hx Cardiomyopathy, T2DM, HTN, Hyperlipidemia 1155 BG: 145 mg/dL – pt nutritional dose is 17 units lispro with Lunch; trays were on unit, RN gave 17 units lispro SC 1205: PT took patient for a walk 1245– pt c/o dizziness to PT, PT reported Sx to RN, BG: 60 mg/dL Case Study-Actual Events Hypoglycemia with Nutritional Insulin What likely caused BG to drop so quickly? What could have been done by the RN to prevent the hypoglycemic event? Case Study-Actual Events Hypoglycemia with TF Hold 74 yo M s/p abd surgery 2° to SBO Hx T2DM on Metformin at home, HTN, Hyperlipidemia, GERD Pt on TF, with 60 units glargine (Lantus) qdaily at 0800 1145 BG: 145 mg/dL, 60 units glargine given SC 2130 TF stopped as pt had loose stool 0030 BG 85 mg/dL 0245 Pt had LE Sz, BG checked at 38 mg/dL Case Study-Actual Events Hypoglycemia with TF Hold What likely caused hypoglycemia? What could have been done by the MD/RN to prevent the hypoglycemic event? Case Study-Actual Events Hypoglycemia with TF Hold, part 2 0245 Pt had LE Sz, BG checked at 38 mg/dL, RN gave D50 IVP 0310 BG: 77 mg/dL, D50 IVP repeated 0400 BG: 125 mg/dL 0730 AM shift RN noticed pt diaphoretic, BG 52 mg/dL Case Study-Actual Events Hypoglycemia with TF Hold, part 2 What likely caused second episode of hypoglycemia? What should be the next steps to prevent another hypoglycemic event? Case Study-Actual Events Hospital Induced Diabetic Ketoacidosis Pt 47 yo M, s/p R-shoulder replacement, Hx T1DM on insulin pump at home (pump off for surgery) PACU BG 489 20 units Regular given Pt admitted to medical floor 1700 BG 267, pt given 6 units lispro 2130 BG 336, pt given 3 units lispro (Next day) 0800 no BG, “RN missed BG check”, no labs ordered 1130 BG “critical high”, Chem 7 sent BG 670, anion gap 27.4…DKA Case Study-Actual Events Hospital Induced Diabetic Ketoacidosis What happened? Who else played a role in the hyperglycemic event? Lessons learned? Questions? Thank you for great care in patients with diabetes!