Chapter 26: The Reproductive System
Chapter 26: The Reproductive System
Objectives:
1. Describe the structure and function of the testes, and explain the importance of their location in the scrotum.
2. Discuss the sources and functions of semen.
3. Outline the events of spermatogenesis.
4. Describe the phases of the male sexual response.
5. Discuss hormonal regulation of testicular function and the physiological effects of testosterone on male reproductive anatomy.
6. Describe the location, structure, and function of the ovaries.
7. Describe the process of oogenisis and compare it to spermatogenesis.
8. Describe the phases of the ovarian cycle, and relate them to events of oogenesis
9. Describe the regulation of the ovarian and menstrual cycles.
10. Discuss the physiological effects of estrogens and progesterone.
11. Discuss the determination of genetic sex and prenatal development of male and female structures.
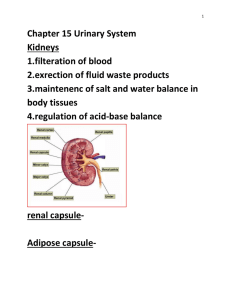
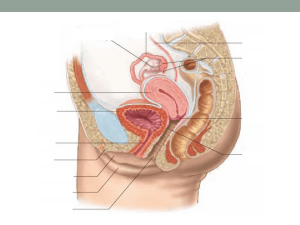
Male reproductive system See figure 26.1, 26.2, 26.4
1. Anatomy
A. Testes : paired gonads found in scrotum for optimum temperature of sperm production. See figure 26.3
B. seminal vesicles : produce 60% of the volume of semen, yellowish, viscous, alkaline with fructose.
C. prostate gland : produces 33% of volume, milky, slightly acidic, contains citrate, enzymes and antigens to activate sperm. Hypertrophy of prostate is common in elderly males.
D. bulbourethral gland : thick, clear mucus that neutralizes acidic urine in the urethra
E. semen : milky white, sticky, with sperm and secretions. Transport medium and nutrients, chemicals to activate and facilitate. 2-5 ml/ejaculation w/ 50-130 million sperm/ml.
2. Physiology
A. erection : parasympathetic response that causes relaxation of vascular smooth muscle (hence, vasodilation). Erectile bodies (cavernosa and spongiosum) fill with blood.
B. ejaculation : propulsion of semen, sympathetic response. Reproductive ducts and accessory glands contract. Bladder sphincter muscle contracts, preventing expulsion of urine or semen reflux.
3. Spermatogenesis : occurs in seminiferous tubules of testes. Begins in puberty, 400 million/day. Meiosis results in 4 haploid spermatids. See figure 26.8, 26.9
During spermiogenesis, a midpiece containing many mitochondria and flagellum develops.
Head of sperm has an acrosome that contains hydrolytic enzymes to penetrate and enter the egg.
Leydig (interstitial) cells between seminiferous tubules produce testosterone.
Hormonal regulation of male reproductive function See figure 26.10
1.
Hypothalamus releases GnRH (gonadotropin releasing hormone) which controls the release of FSH and LH from the anterior pituitary gland.
2.
FSH goes to the semiferous tubules and stimulates spermatogenesis by causing the release of androgen binding protein (ABP) that prompts the binding and concentrating of testosterone to spermatogenic cells (makes cells receptive to testosterone’s stimulating effects). Then meiosis occurs.
3.
LH binds to interstitial cells (Leydig cells) and stimulates them to secrete testosterone.
Testosterone exerts a negative feedback control on the hypothalamus and anterior pituitary .
Mechanisms and effects of testosterone activity
1. Testosterone is synthesized from cholesterol. It activates specific genes to enhance the production of certain proteins in target cells. It is sometimes changed to DHT or estrogen in order to bring about its effects.
2. During puberty, it targets all accessory reproductive organs (ducts, glands,
& penis) to grow and assume adult size and function. Functions will cease to exist in the absence of testosterone
3. Male secondary sex characteristics: Axillary, facial hair, enhanced growth on chest and other areas. Deepening of voice as larynx enlarges. Skin thickens and becomes oilier. Bones grow in size and density. Skeletal muscle increases in size and mass. Boosts BMR. Influences behavior (libido)
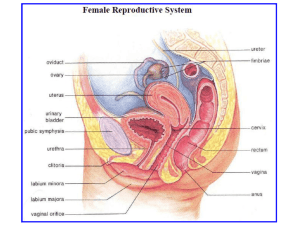
Female reproductive system
1. Oogenesis: See figure 26.19, 26.20
During fetal development the primary oocytes begin the 1st meiotic division
(prophase of meiosis I: tetrads form and can lead to nondisjunction)
By birth 2 million oocytes have formed
By puberty 400,000 oocytes remain and each month a small number are activated by FSH but only one oocyte is selected to complete meiosis I to produce a haploid ovum
Fewer than 500 oocytes are ever released.
2. Ovarian cycle See figure 26.22 a. Follicular phase:
Period of follicle growth from day 1-~14
1. Primordial follicles activated, oocyte enlarges, become primary follicle
2. Theca folliculi forms to produce estrogen and zona pelucida (thick transparent membrane forms)
3. Vesicular follicle bulges from surface by day 14. Primary oocyte completes meiosis I and becomes secondary oocyte. b. Ovulation: occurs near midcycle
Ovary wall ruptures and expels secondary oocyte into peritoneal cavity.
One dominant follicle develops when the LH stimulus is given
Fraternal twins occur when more than one follicle ovulates c. Luteal phase : corpus luteum activity from day 14-28 (always 14 days). Ruptured follicle collapses to form corpus luteum, an endocrine gland that secretes progesterone and estrogen. Begins to degenerate in about 10 days. Corpus albicans remains.
Hormonal regulation of female reproduction: estrogen inhibits hypothalamus until puberty.
Menarche: 1 st menstrual period See figure 26.21, 26.22
1. Day 1: GnRH from hypothalamus stimulates release of FSH and LH from anterior pituitary
2. FSH and LH stimulate follicle growth and thecal cells. As follicle grows, estrogen secretion begins from thecal cells. (Androgens are released to be converted to estrogen)
3.
Negative feedback of estrogen of FSH and LH release occurs, positive feedback on estrogen production. Inhibin also inhibits release of FSH
FSH).
4.
5.
Now high estrogen levels exert positive feedback on anterior pituitary.
Day 13: about 24 hours prior to ovulation an LH surge occurs (and to a lesser extent of
6. LH surge stimulates primary oocyte of dominant follicle to complete meiosis I. Secondary oocyte continues to metaphase II. LH also triggers ovulation (about day 14). Estrogen levels decline.
7.
Corpus luteum forms.
8.
Increasing progesterone and estrogen from corpus luteum now have an inhibitory effect again on FSH and LH.
9. A decrease in LH causes corpus luteum to degenerate. begins.
10. Day 28: decreasing ovarian hormones ends blockade of FSH and LH and new cycle
Uterine (Menstrual) cycle See figure 26.22
1. Day 1-5: Menstrual phase : uterus sheds all but basalis layer (FSH and LH are beginning to rise and ovarian hormone levels are lowest); bleeding for 3-5 days due to break up of spiral arteries. By day 5 the growing ovarian follicles are starting to produce more estrogen.
2. Day 6-14: Proliferative phase : endometrium rebuilds itself by basalis layer generating a new functionalis layer due to presence of estrogen. Glands enlarge and spiral arteries increase in number. Estrogens also induce synthesis of progesterone receptors.
3. Day 15-28: Secretory phase : endometrium prepares for implantation. Increasing progesterone from corpus luteum cause spiral arteries to elaborate and coil. Uterine glands secrete glycoproteins to sustain embryo until implantation. Increasing progesterone causes formation of cervical plug. LH is inhibited, corpus luteum degenerates. Fat deposits help convert adrenal androgens to estrogens.
Extrauterine effects of estrogens and progesterone
1.
promote oogenesis and follicle growth
2.
3.
maturation of reproductive tract
growth spurt but earlier than boys and earlier closure of epiphyseal plates.
4.
growth of breasts, subcutaneous fat, widening of pelvis, axillary and pubic hair, low blood cholesterol (high HDL’s) and calcium uptake.
Pregnancy : from the start of the last menstrual period until birth = 280 days.
The oocyte is viable for 12-24 hours after ovulation. Sperm have fertilizing power for 24-72 hours after ejaculation. Coitus must occur no more than 3 days before ovulation for a girl and no later than 24 hours after ovulation for a boy. Fertilization occurs 1/3 of the way down the uterine tube and forms a zygote.