Blood Pressure
advertisement

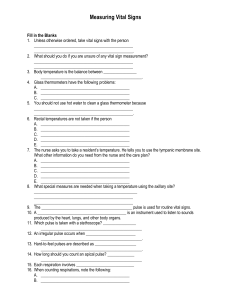
Measurements Pre-CNA SP2-AP2 This presentation will: Briefly review the four vital signs Height and weight Intake and Output Measurements When working with your resident, you will measure: Vital signs (VS) Height/weight (ht/wt) Intake and output (I&O) Why Do You Take Vital Signs? Vital signs show minor changes in the resident’s condition. Vital signs show how the resident responds to treatment. Vital signs change with fear, exercise, anxiety, pain and other activities. Vital Signs Vital signs include: Temperature Pulse Respiration Blood pressure Report vital signs promptly when: they are above or below normal. there is a significant change from the prior reading. Body Temperature The body temperature is the amount of heat produced by the body. The temperature is lower in the morning and higher in afternoon and evening. Body temperature is affected by age, weather, exercise, emotions, stress and illness. Sites for Measuring Temperature Mouth – oral Rectal - anus Ear – tympanic Axilla - underarm Oral Temperature Taken in the mouth. Do not use if a person has an injury to his mouth, difficulty breathing, or confusion. Normal Range 97.6-99.6 F (36.5 C-37.5 C) Rectal Temperature Do not use when the person has: diarrhea, a rectal injury or rectal surgery, heart disease, or confusion. Normal Range 98.6-100.6 F (37.0-38.0 C) Most accurate route Tympanic Temperature This site has fewer microbes than other sites. However, it should not be used if there is ear drainage. Normal range 97.6-99.6 F (36.5-37.5 C) Axillary Temperature The axilla is the “armpit”. It is the least accurate site. Normal Range 96.6-98.6 F (35.5-36.5 C) Pulse Used to monitor the circulatory system (heart and blood vessels) Pulse Rate Measures how fast the heart is beating Normal rate=60-100 beats/minute Tachycardia=“fast heart” >100 beats/minute Bradycardia=“slow heart” <60 beats/minute Other Pulse Characteristics Rhythm Regular: same amount of time between beats Irregular: NOT the same amount of time between beats or skipped (missed)beats Strength Strong/bounding: easy to feel Weak/thready: difficult to feel The Pulse Sites Taking A Pulse These pictures show radial and brachial pulse sites. Radial pulse The most common location to check a pulse On the thumb side of the wrist Gently press with 2 or 3 fingers. Do not use your thumb when checking a pulse Count for 1 minute Blood Pressure Used to monitor the circulatory system. Normal range: 90-120 60-80 Systolic Diastolic Systolic Heart is contracting Higher or top number First sound you hear Normal Range: 90-120mmHg Diastolic Heart is resting Lower or bottom number Last sound you hear Normal Range: 60-80mmHg Hypertension Hyper=“too much” Tension=“pressure” High BP Systolic >140 Diastolic>90 Hypotension Hypo=“too little” Tension=“pressure” Low BP Systolic<90 Diastolic<60 When do you not use a person’s arm to measure blood pressure? If the arm has an IV, cast or dialysis access site. If a woman has had surgery to remove a breast on that side of her body. Any injury of surgery to the arm. What are the parts of the sphygmomanometer? Manometer Bulb valve cuff Respiration Respiration means breathing air into (inhalation) and out of (exhalation) the lungs. 1 respiration= 1 exhalation + 1 inhalation People tend to change breathing patterns when they know someone is counting their respirations. Respirations are counted right after taking the pulse. Keep your fingers on their radial pulse and observe their chest rising and falling. Count for 1 minute. What to observe when taking respirations Rate: Normal respirations are 12-20 times per minute. Depth: deep or shallow Rhythm: regular or irregular Equality: equal or unequal Pt. c/o pain or dyspnea Abnormal noises Height/Weight Baseline height and weight is measured when the resident is admitted to the nursing home. Height Standing: No shoes, have the person stand straight. Lying Have person in good alignment in supine position. Using a tape measure, measure from top of head to soles of feet. Weight • • • • • The scale should be set at zero. The resident should be weighed at the same time of day wearing as few clothes as possible. The morning before breakfast is the best time. Make sure the person empties his/her bladder before weighing. This is one method of monitoring the patient’s fluid status Intake and Output (I&O) Used to monitor fluid balance and kidney function Intake= amount of fluid entering the body PO (oral) Output=amount of fluid leaving the body Urine Diarrhea Emesis Drainage Sweat (perspiration) Breathing (exhalation) As a NA, you will help record: Oral Fluid Intake water, milk, juice, coffee, etc. Foods that melt at room temperature: Ice cream Jello Popsicles You will also record: Measurable fluid output: Urine Diarrhea Emesis Drainage from tubes You cannot measure: Non-measurable output Sweat Breathing Wound drainage without a tube If a person is incontinent How many milliliters (ml) in an ounce? 1 ounce (oz) = 30 ml (cc) graduate