Basic Human Needs Bowel Elimination
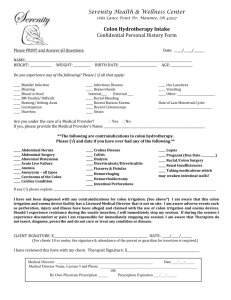
advertisement

Bowel Elimination Bowel Elimination GI Tract is a series of hollow mucous membrane lined muscular organs Purpose is to absorb fluids & nutrients, prepare food for absorption & provide storage for feces GI Tract Anatomy Mouth Esophagus Stomach Small Intestine Large Intestine Rectum Mouth Digestion begins here Mechanical, chemical breakdown of nutrients Teeth-Mastication Salivary secretions-enzymes Food Bolus مضغة Esophagus Hollow, muscular tube for passage of food to stomach Peristaltic waves, contraction and relaxation of smooth muscle moves food down to stomach Sphincter control to prevent reflux Stomach Food is temporarily stored and mechanically and chemically broken down Secretes HCL, mucus, pepsin, & intrinsic factor(Needed for Vitamin B12 absorption) Food is converted into chyme Small Intestine 1 inch in diameter 20 feet long Three divisions: Duodenum, Jejunum, Ileum Enzymes in small intestine (amylase, lipase, & bile) break down fats, proteins & carbs into basic elements Nutrients absorbed in duodenum & jejunum, ileum absorbs vitamins, iron, & bile salts Large Intestine Lower GI tract Larger diameter, 5-6 feet in length 3 divisions: cecum, colon, rectum Responsible for absorption of water Primary organ of bowel elimination Cecum-chyme enters cecum via the ileocecal valve, valve prevents regurg back to small intestine, cecum ends with appendix Colon 3 Divisions: Ascending, Transverse, Descending Colon Functions: Absorption, Protection, Secretion, & Elimination (stool and flatus) Rectum Sigmoid colon Storage of feces Length varies with age When fecal mass or flatus moves into rectum, it distends and defecation begins Process involves involuntary (Internal sphincter) and voluntary control (external sphincter) Valsalva Maneuver - voluntary contraction of abdominal muscles Factors Affecting Bowel Elimination Age Infection Diet Fluid Intake Physical Activity Psychological factors Personal Habits Factors Affecting Bowel Elimination Position during Defecation Pain Surgery and Anesthesia Medications Common Bowel Elimination Problems Constipation Impaction Diarrhea Incontinence Flatulence Hemorrhoids Constipation More of a symptom than a disorder Decrease in frequency of BM Straining & pain on defecation is associated symptoms(Valsalva manuever) Can be significant heath hazard (increase ICP, IOP, reopen surgical wounds, cause trauma, cardiac arrhythmias) Impaction Results from unrelieved constipation Collection of hardened feces wedged عالقinto rectum Can extend up to sigmoid colon Most at risk: confused, unconscious (all are at risk for dehydration) Impaction When a continuous ooze of diarrheal stool develops, impaction should be suspected Associated S/S: Loss of appetite, abdominal distention, cramping, rectal pain Diarrhea Increase in number of stools & the passage of liquid, unformed stool Symptom of disorders affecting digestion, absorption, & secretion of GI tract Intestinal contents pass through small & large intestines too quickly to allow for usual absorption of water & nutrients Diarrhea Irritation can result in increased mucus secretion, feces become too watery, unable to control defecation Excess loss of colonic fluid can result in acid-base imbalances or fluid/electrolyte imbalances Can also result in skin breakdown Conditions that cause Diarrhea Emotional Stress Intestinal Infection (Clostridium difficile) Food Allergies Food Intolerance Tube Feedings (Enteral) Medications Laxatives Colon Disease Surgery Incontinence Inability to control passage of feces and gas from the anus Caused by conditions that create frequent, loose, large volume, watery stools or conditions that impair sphincter control or function Flatulence Gas accumulation in the lumen of intestines Bowel wall stretches and distends Common cause of abdominal fullness, pain, & cramping Gas escapes through mouth (belching), or anus (flatus) Flatus Formation Air swallowing Diffusion of gas from bloodstream into intestines Bacterial action on unabsorbable CHO (Beans) Fermentation of CHO (cabbage, onions Can stimulate peristalsis Adult forms 400-700 ml of flatus daily Flatulence Causes: Decreased peristalsis Constipation Medications Surgery Diet Stress Decreased activity NonInvasive Interventions for Flatulence *Ambulation* Knee chest position Invasive Interventions for Flatulence Glycerin Suppository Harris Flush Rectal Tube Hemorrhoids Dilated, engorged veins in the lining of the rectum External (Clearly visible) or Internal Caused by straining, pregnancy, CHF, chronic liver disease Physical Assessment Inspection- observe contour of abd and note visible peristalsis Auscultation- listen for bowel sounds all quadrants Percussion- resonant or tympany over hollow organs…dullness over intestinal obstruction Palpation- feel for masses, tenderness etc… Bowel Diversions Certain diseases cause conditions that prevent normal passage of feces through rectum Creates need for temporary or permanent artificial opening (stoma) in the abdominal wall Bowel Diversions Surgical openings (ostomy) are most commonly formed in the ileum (ileostomy) or the colon (colostomy) Incontinent ostomy- need to wear appliance pouch Continent ostomy- have control through use of ostomy cap Ostomy Nursing Considerations Patient Education Care of stoma, appliance selection and use Body Image considerations Support groups Enterostomal nursing- specialty within profession Nursing Process Assessment Nursing History Physical Assessment Lab Tests Fecal characteristics Diagnostic evaluation- Endoscopy, Colonoscopy Nursing Diagnosis Bowel Incontinence Constipation Diarrhea Impaired Skin Integrity Body Image Disturbance Altered bowel elimination Pain Implementation Promoting Normal Defecation Positioning of patient-squatting Positioning on bedpan Use of cathartics, laxatives Anti-diarrheal agents Enemas Digital removal of stool Ostomy care Interventions: Promote Bowel Elimination Laxatives and Cathartics Enemas Suppositories Digital Removal Types of Enemas Types of Enemas Cleansing Retention Return Flow Enemas Cleansing enema Tap water Normal saline Hypertonic Solutions (Fleet’s enema) Soapsuds Oil Retention Medicated enemas (Kayexalate, Lactulose) Administering a Cleansing enema P&P pg. 12001201 Tap Water (TWE) Amount: 500-1000cc Action: Distends, increases peristalsis Time: 15 min. Indicated: inflamed bowels/irritated colon Contraindicated: Atonic bowels, fluid restrictions Normal Saline Amount: 500-1000cc Action: Distends, increases peristalsis Time: 15 min. Indicated:Inflamed bowels/irritated colon Contraindicated: Na retention problems, fluid restrictions Soap Amount: 500-1000cc (Castile 5ml/1000cc) Action: Distends, Irritates Time: 15 min. Indicated: Constipation Contraindicated: Prior to rectal exams Hypertonic Amount: 70-130 cc solution Action: Distends/Irritates Time: 5-10 min. Indicated: Constipation, convenience Contraindicated: Dehydration, Na problems Oil Retention Amount: 120-200cc Action: Lubricates Time: 30 min. Indicated: Fecal impaction Contraindication: none Colostomy nursing care 1. Wash hands. 2. Apply clean gloves. 3. Assemble irrigation kit: Attach cone or catheter to irrigation bag tubing. 4. Fill irrigation bag with 1000 cc tepid tap water 5. Open clamp and let water from the irrigation bag fill the tubing. 6. Hang bottom of irrigation bag at height of client’s shoulder, or 18 inches above the stoma if the client is supine. 7. Check direction of intestine by inserting a gloved finger into orifice of stoma. 8. Place irrigation sleeve over stoma and hold in place with beltيطوق بحزام 9. Spray inside of irrigation sleeve and bathroom with odor eliminator (usual dose is two sprays). 10. Cuff end of irrigation sleeve and place into toilet bowl (if client is in bathroom) or bedpan (if client is in bed or chair) (see Figure 6-22-5). 11. Lubricate the cone end of the irrigation tubing and insert into orifice of stoma through the top opening of irrigation sleeve 12. Close top of irrigation sleeve over the tubing. 13. Slowly run water through tubing into colon 14. Remove cone after all water has emptied out of irrigation bag. 15. Close end of irrigation sleeve by attaching it to the top of the sleeve. 16. Encourage client to ambulate to facilitate emptying of remaining stool from colon. 17. Remove irrigation sleeve after 20–30 minutes or when stool is no longer emptying from colon. 18. Cleanse stoma and skin with warm tap water. Pat dry. 19. Place gauze pad over stoma to absorb mucus from stoma. 20. Secure gauze with hypoallergenic tape. 21. Remove gloves and wash hands.