Diagnosis and Management of Acute Abdominal Pain - mcstmf
advertisement

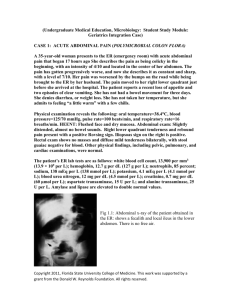
Introduction Complaints related to abdominal pain comprise between 7- 9 % of all visits to the ED. Of those, the most common discharge diagnosis is Abdominal Pain NOS. Although most abdominal pain is non-emergent and self-limited in nature, attention must be paid to not miss medical and/or surgical emergencies. Important Factors Patients rarely present with the classical signs/symptoms of acute abdominal pain. Three important factors to consider are age, gender, and co-morbidities. Definition The term acute abdomen refers to a sudden, severe abdominal pain that is less than 24 hours in duration. It is in many cases a medical emergency, requiring urgent and specific diagnosis. Several causes need surgical treatment. Don’t forget about the chronic pain that has acutely worsened. Basic Principles Proper evaluation and management requires one to recognize: 1. Does this patient need surgery? 2. Is it emergent, urgent, or can wait? • In other words, is the patient unstable or stable? Remember medical causes of abd pain > 100 causes exist 1. 2. 3. 4. 5. 6. 7. 8. NSAP (34%) Acute appendicitis (28%) Acute chlecystitis (10%) SBO (4%) Perforated PU (3%) Pancreatitis (3%) Diverticular disease (2%) Others (13%) In children Acute appendicitis UTI Mesenteric adenitis GE Constipation 50-65% inaccurate initial diagnosis 50% of surgical admissions are emergencies, and of those 50% present with acute abdomen. Types of Pain Visceral Pain: caused by stretching of fibers innervating the walls of hollow organs or capsules of solid organs, described as cramp or dull pain Parietal Pain: caused by irritation of fibers that innervate the parietal peritoneum, pain is more sharp and localized Referred Pain: pain at a location distant to the diseased organ based on embryological origin Visceral pain I. Parietal pain Is localised to the dermatome above the site of the stimulus. Character: I. sharp and localized pain. II. somatic nerve distribution (T7-L2, umbilicus at T12). The exception to this is the diaphragmatic portion, which is supplied centrally by the phrenic nerve (C3-C5), and peripherally by the lower six intercostal and subcostal nerves. III.sensitive to mechanical stimuli (stretching, pinprick , pinch), heat, electrical shock, chemical stimulus, infection-inflammation. I. Referred pain It’s pain perceived distant from its source and results from convergence of nerve fibers at the spinal cord. produces symptoms, not signs e.g. tenderness Causes of Acute Abdomen I. Surgical II. Gynecological III. Medical Think Broad categories for DDx surgical Causes o Inflammation o Obstruction o Ischemia o Perforation (any of above can end here) Offended organ becomes distended Lymphatic/venous obstruction due to ↑ pressure Arterial pressure exceeded → ischemia Prolonged ischemia → perforation Inflammation versus Obstruction Organ Lesion Stomach Gastric Ulcer Duodenal Ulcer Biliary Tract Acute cholecystitis Acute cholangitis Pancreas Acute, recurrent, or chronic pancreatitis Small Intestine Large Intestine Crohn’s disease Meckel’s diverticulum Appendicitis Diverticulitis Location Lesion Small Bowel Obstruction Adhesions Hernia Cancer Crohn’s disease Gallstone ileus Intussusception Volvulus Large Bowel Obstruction Malignancy Volvulus: cecal or sigmoid Diverticulitis Biliary colic Ureteric colic Acute retention Ischemia versus Perforation Acute mesenteric ischemia Usually acute occlusion of the SMA from thrombus or embolism Perforated PU Chronic mesenteric ischemia Typically smoker, vasculopathy with severe atherosclerotic vessel disease Perforated appendix Ischemic colitis Torsion of a viscus Perforated diverticular disease Acute chlolecystitis with Perforation Ruptured AAA Perforated bladder GYN Causes Organ Lesion Ovary Torsion of ovary Ruptured graafian follicle Tubo-ovarian abscess (TOA) Fallopian tube Ectopic pregnancy Acute salpingitis Pyosalpinx Uterus Uterine rupture Endometritis Non-Surgical (Medical) Causes System Cardiac Disease Myocardial infarx Acute pericarditis Pulmonary Pneumonia System Disease Endocrine Diab ketoacidosis Addisonian crisis Metabolic Acute porphyria Mediterranean fever Hyperlipidemia Pulmonary infarx PE GI Acute pancreatitis Gastroenteritis Acute hepatitis Musculoskeletal Rectus muscle hematoma GU Pyelonephritis CNS PNS Tabes dorsalis (syph) Nerve root compression Vascular Aortic dissection Hematological Sickle cell crisis Generalized AP Perforation Mesenteric ischemia AAA Acute pancreatitis Central AP Early appendicitis SBO Acute pancreatitis Ruptured AAA Mesenteric thrombosis Acute gastritis Epigastric pain DU / GU Recurrent, relationship to meals, relationship to posture Oesophagitis Acute pancreatitis History of alcohol consumption, history of similar event, elevated labs AAA RUQ pain Acute cholecystitis Recurrent attacks, tender over gall bladder area DU Acute pancreatitis Retrocecal appendicitis Shift of pain, tenderness R L Pneumonia Fever, tachypnea, bronchial breathing Subphrenic abscess LUQ pain Pneumonia Acute pancreatitis Splenic rupture Splenic abscess Acute perinephritis Subphrenic abscess RIF pain Acute appendicitis Shift of pain, anorexia, localized tenderness Mesenteric adenitis (young) Fever, inconstant signs Perf DU Diverticulitis Salpingitis Ureteric colic Colicky pain, hematuria Meckel’s diverticulum Ectopic pregnancy Crohn’s disease Biliary colic (low-lying GB) LIF pain Diverticulitis Constipation IBS PID Rectal Ca UC Ectopic pregnancy Suprapubic pain Acute urinary retention Palpable bladder, difficulty passing urine UTI Cystitis PID Ectopic pregnancy Diverticulitis Loin pain Muscle strain UTIs Renal stones Pyelonephritis Approach to Acute Abdomen Take a proper Hx and Ex, do not work to the diagnosis given to you by the referring doctor. History is THE MOST IMPORTANT part of the diagnostic process: Location , onset, nature , severity, radiation, aggravating or relieving factors, associated symptoms A good medical history A good social history, including alcohol, drugs, domestic abuse, stressors, etc. Family history is important (IBD, cancers, etc) MEDICATION INVENTORY CLUES in Hx. Was onset of pain gradual or sudden? Sudden perforation, hemorrhage, infarct Gradual inflammation, peritoneal irrigation, hollow organ distension What does nature of pain? Steady pain inflammatory process Colicky pain Biliary colic ,obstruction Stabbing AAA Does pain radiate anywhere? Right shoulder, angle of right scapula Around flank to groin kidney, ureter In Females ? Last menstrual period? Abnormal bleeding? GB Progression of Pain Associated symptoms • • • • Fever Genitourinary Gynaecological Vascular PMSH • • • • • Previous episodes of AP Investigations Operations Chronic disease Medications (NSAIDs) Physical examination Administration of analgesics prior to surgical consultation does not obscure the diagnosis, but improves accuracy. Observation Bending Forward: Chronic Pancreatitis Jaundiced: CBD obstruction Dehydrated: Peritonitis, SBO Inspection Not move with respiration in peritonitis Scaphoid or flat in peptic ulcer Distended in ascites or intestinal obstruction Visible peristalsis in a thin or obstruction Scars : relevant previous illness or adhesions Hernia : intestinal obstraction Palpation Check for Hernia sites Tenderness Rebound tenderness. Guarding. Rigidity. Rebound tenderness, considered the clinical indicator of peritonitis, has a high (25%) false -ve rate Rigidity, referred tenderness & cough pain are sufficient evidence for peritonitis Local Right Iliac Fossa tenderness: Acute appendicitis Acute Salpingitis in females Low grade, poorly localized tenderness: Intestinal Obstruction Tenderness out of proportion to examination: Mesenteric Ischemia Acute Pancreatitis Flank Tenderness: Perinephric Abscess Retrocaecal Appendicitis Important Signs in Patients with Abdominal Pain Sign Finding Association Cullen's sign Bluish periumbilical discoloration Kehr's sign referd left shoulder pain McBurney's sign Tenderness located 2/3 distance from anterior iliac spine to umbilicus on right side Murphy's sign Abrupt interruption of inspiration on palpation of right upper quadrant Iliopsoas sign Hyperextension of right hip causing abdominal pain Appendicitis Obturator's sign Internal rotation of flexed right hip causing abdominal pain Appendicitis Grey-Turner's Discoloration of the flank Chandelier sign Manipulation of cervix causes patient to lift buttocks off table PID Rovsing's sign Right lower quadrant pain with palpation of the left lower quadrant Appendicitis Retroperitoneal haemorrhage Splenic rupture Ectopic pregnancy rupture Appendicitis Acute cholecystitis Retroperitoneal hemorrhage Percussion Resonance : intestinal obstruction Loss of liver dullness: gastrointestinal perforation Dullness : free fluid , full bladder Shifting dullness : free fluid Auscultation NR Bowel sounds 5-30/min > 2min to confirm absent High pitched, hyperactive or tinkling caused by powerful peristaltic action , partial obstruction , abdominal cramping Hypoactive bowel sounds indicates Peritonitis , non-mechanical obstruction , Inflammation , gangrene Bruit in epigastrium indicates AAA Systemic Examination PR Examination: Tenderness Induration Mass Frank blood Systemic Examination PV Examination Bleeding Discharge Cervical motion tenderness Adnexal masses or tenderness Uterine Size or Contour Investigations Beware of misleading by investigations A.Blood tests CBC (Hb & WBC) & U&E Amylase (Pancreatitis) but remember 20% have NR values LFTs CRP & ESR (inflammatory markers) ABG Serum calcium (Abnormal GI motility PU, Pancreatitis) Clotting (acute pancreatitis, sepsis, DIC, liver disease) Blood glucose ECG Attention to the WBC as a screening test only if substantially elevated. 25% of patients with elevated WBC do not have different outcomes from those with a normal WBC. CBC has a limited clinical utility In RLQ pain to rule in or rule out Acute Appendicitis wbc count (n>70%) < 8,000 very unlikely 8,000-10,000 unlikely 10,000-12000 equivocal 12,000-15,000 suggestive 15,000-20,000 highly suggestive >20,000 probably ruptured B. Urinalysis Cheap Simple & available test High yield when results fit with the clinical scenario Pregnancy test C. Radiology Erect CXR Supine AXR USS Biliary trees , Mass , fluid , Retroperitoneal organs Ultrasound in Acute Appendicitis +!? Causes of free sub- IVU (renal/ureteric colic) CT scan Similar benefit as in U/S but more time consumed , more accurate more expensive more risk diaphragmatic gas Perforation of viscus Gas-forming infection Pleuroperitoneal fisula Iatrogenic Interposition of bowel b/t liver & diaphragm Plain X-rays have limited utility in the evaluation of AAP Low diagnostic yield High incidence of misleading incidental findings Lack of impact on management Exception: Bowel obstruction or perforation Labs & Imaging Test CBC w diff Reason Left shift can be very telling ABG N/V, acidosis, dehydration Amylase Pancreatitis, perf DU, bowel ischemia LFT Jaundice, hepatitis UA GU- UTI, stone, hematuria Beta-hCG Ectopic Test KUB Reason Flat & Upright SBO/LBO, free air, stones Ultrasound Chol’y, jaundice GYN pathology CT scan Anatomic dx Case not straight forward Diagnostic accuracy Findings in plain X-ray abdomen in case of Biliary disease : 1. radioopaque shadow for stone 2. pneumobilia 3. calcification of porcelain gallbladder In case of pancreatic disease : 1. calcification in chronic pancreatitis 2. sentinel loop : dilatation of a segment of large or small intestine, indicative of localised ileus from nearby inflammation. In case of appendicitis: 1. Fecalith: a hard stony mass of feces 2. Phlebolith : is a small local, usually rounded, calcification within a vein 3. Abscent of psoas muscle shadow calcification of porcelain gallbladder Pneumoperitoneum Findings in plain X-ray abdomen Intestinal obstruction Erect (air fluid level) Step ladder Central Small multiple Supine (dilatation of bowel) >3cm plicae circulares Erect (air fluid level) Peripheral Large Few Supine (dilatation of bowel) > 5cm in sigmoid > 10 cm in cecum Peripheral haustration SBO LBO ultrasound . Hepatobiliray tree(stones,mass,thickining of the wall) *pancreases *kidney *pelvic organ *intrabdominal fluid collection Gall stone\ appendicolith CT scan . Helpful in case of abdominal pain without clear etiology better in evaluation of abdominal aortic aneurysm. 5.helical CT_scan Provide rapid cost effective diagnostic tool. CT scan What is the diagnosis? Acute appendicitis Acute pancreatitis D. Laparoscopy Early diagnostic laparoscopy may result in: accurate, prompt, efficient management of AAP Reduces the rate of unnecessary laparotomy Increases the diagnostic accuracy May be a key to solving the diagnostic dilemma of NSAP. Immediate Treatment of the Acute Abdomen I. Start large bore IV with either saline or lactated Ringer’s solution II. IV pain medication III. Nasogastric tube if vomiting or concerned about obstruction. IV. Foley catheter to follow hydration status and to obtain urinalysis. V. Antibiotic administration if suspicious of inflammation or perforation. VI. Definitive therapy or procedure will vary with diagnosis. VII. Reassess patient on a regular basis. Decision to operate • Proper management requires a timely decision about the need for surgical operation. Peritonitis Tenderness w/ rebound, involuntary guarding Severe / unrelenting pain “Unstable” (hemodynamically, or septic) Tachycardic, hypotensive, white count Intestinal ischemia, including strangulation Pneumoperitoneum Complete or “high grade” obstruction Take Home Massage Careful history (pain, other GI symptoms) Remember DDx in broad categories Narrow DDx based on hx, exam, labs, imaging Always perform ABC, Resuscitate before Dx If patient’s sick or “toxic”, get to OR (surgical emergency) Ideally, resuscitate patients before going to the OR Don’t forget GYN/medical causes, special situations For acute abdomen, think of these commonly (below) Perf DU Appendicitis +/perforation Diverticulitis +/perforation Bowel obstruction Cholecystitis Ischemic or perf bowel Ruptured aneurysm Acute pancreatitis