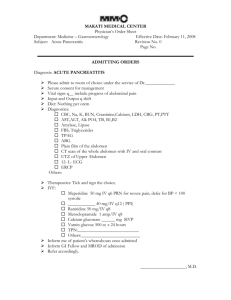
Acute Pancreatitis
advertisement
Acute Pancreatitis Celine Estrada Patient Case Patient’s Chief Complaint: “It feels like I have a knife in my stomach” History of Present Illness (HPI): ▵ Patient is a 63-year old African American male, who presents to the emergency room at the hospital with intense left upper quadrant pain radiating to his back and under his left shoulder blade. He states that he has had intermittent, upper abdominal pain for approximately three weeks but that the pain has been increasing in severity during the last four days. History Patient Medical History (PMH): ▵ Coronary Artery Disease (CAD); S/P angioplasty 1 year ago; denies any chest pain since. ▵ Hypertension (HTN); does not remember exactly how long; he states “for years” ▵ S/P cholescystectomy ▵ S/P appendicitis ▵ (+) for hepatitis C x 5 years ▵ Generalized anxiety disorder; 18 months Familial History (FH): ▵ Father was an alcoholic and died at the age of 49 from myocardial infarction (MI) ▵ Mother alive at 83 with CAD ▵ Brother, age 60, alive and healthy ▵ No family history of gastrointestinal disease reported SH & Meds Social History (SH): ▵ Married with 8 children ▵ Retired high school math teacher and wrestling coach ▵ Alcohol abuse with 10-12 cans of beer per day for 15 years ▵ Denies use of tobacco or illicit drugs Medications (Meds): ▵ Nifedipine 90mg po QD ▵ Lisinopril 20mg po QD ▵ Paroxetine 20mg po QD ▵ Tylenol #3, 2 tablets po QD PRN for back pain that started recently Q1. For which condition is this patient likely taking nifedipine? Q2. For which condition is this patient likely taking lisinopril? Q3. For which condition is this patient likely taking paroxetine? Allergies + ROS Allergies: ▵ PCN Rash ▵ Aspirin Hives and wheezing ▵ Cats Wheezing Review of Systems (ROS): ▵ States that he’s been feeling “very warm” and has experienced several episodes of nausea and vomiting during the past 72 hours ▵ Also describes an 8- to -10 lb weight loss over the past 1 ½ months secondary to intense post-prandial pain and loss of appetite ▵ Reduction of frequency in bowel movements ▵ No complains of diarrhea or blood in stool ▵ No knowledge of any previous history of poor blood sugar control Physical Examination Gen: ▵ The patient is a black male who looks his stated age. He seems restless and in acute distress. He is sweating profusely and seems ill. He is bent forward on the examiner’s table. Vitals: BP 85/60 HR 120 T RR 35 101.4ºF WT 154lb HT 5’7 ½” Physical Examination (cont.) Head, Eyes, Ears, Nose, Throat (HEENT): ▵ PERRLA ▵ EOMI ▵ (-) jaundice in sclera ▵ TMs intact ▵ Oropharynx pink and clear ▵ Oral mucosa dry Skin: ▵ Dry with poor skin turgor ▵ Some tenting of skin noted ▵ No lesions noted ▵ (-) Grey Turner sign ▵ (-) Cullen sign Q4. What is meant by “tenting of the skin” and what does this clinical sign suggest?: Q5. Are the negative Grey Turner and Cullen signs evidence of a good or poor prognosis?: Grey-Turner’s Sign Physical Examination (cont.) Neck: ▵ Supple ▵ (-) Carotid bruits, lymphadenopathy, thyromegaly, and JVD Heart: ▵ Sinus tachycardia ▵ Normal S1 and S2 and (-) for additional cardiac sounds ▵ No m/r/g Lungs: ▵ Clear to auscultation bilaterally Physical Examination (cont.) Abdomen (Abd): ▵ Moderately distended with diminished bowl sounds ▵ (+) Guarding ▵ Pain is elicited with light palpitation of left upper and mid-epigastric regions ▵ (-) Rebound tenderness, masses, HSM, and bruits Extremities (Ext): ▵ No CCE ▵ Cool and pale ▵ Slightly diminished pulses in all extremities ▵ Normal ROM throughout ▵ Diaphoretic Physical Examination (cont.) Rectum (Rect): ▵ Normal sphincter tone ▵ No bright red blood visible ▵ Stool is guaiac-negative ▵ (-) Hemorrhoids ▵ Prostate WNL with no nodules Neuro: ▵ A & O x 3 (person, place, time) ▵ Able to follow commands ▵ CNs II-XII intact ▵ Motor, sensory, cerebellar, and gait WNL ▵ Strength is 5/5 in all extremities ▵ DTRs 2+ throughout Laboratory Blood Test Results Na 134 meq/L Neutrophils 73% T bilirubin 0.9mg/dL K 3.5 meq/L Bands 3% Alb Cl 99 meq/L Eosinophils 1% Amylase 1874 IU/L HCO3 25 meq/L Basophils 1% Lipase 2119 IU/L BUN 34 mg/L 20% Ca 8.3mg/dL 2% Mg 1.7mg/dL Lymphocytes 3.3 g/dL Cr 1.5 mg/dL Monocytes Glu, fasting 415mg/dL AST 291 IU/L PO4 2.4mg/dL Hb 18.3 g/dL ALT 161 IU/L Trig 971 mg/dL Hct 53% Alk phos 266 IU/L Repeat Trig 969 mg/dL LDH 411 IU/L SaO2 WBC 16,400/mm3 96% Urinalysis Appearance yellow, clear SG 1.023 pH 6.5 Glucose + Bilirubin - Bacteria - Ketones - Nitrite - Urobilinogen - Hemoglobin - Crystals - WBC 2/HPF Protein - Casts - RBC 1/HPF Physical Examination (cont.) Chest X-Ray: ▵ Anteroposterior view shows heart to be normal in size ▵ Lungs are clear without infiltrates, masses, effusions, or atelectasis Abdominal Ultrasound: ▵ Non-specific gas pattern ▵ No regions of dilated bowl Abdominal CECT: ▵ Grade C Q6. Identify three major risk factors for acute pancreatitis in this patient Q7. Identify two abnormal laboratory tests that suggest that acute renal failure has developed in this patient Q8. Why are hemoglobin and hematocrit abnormal? Q9. How many Ranson criteria does this patient have and what is the probability that the patient will die from this attack of acute pancreatitis? Q10. Does the patient have a significant electrolyte imbalance? Q11. Why was no blood drawn for an ABG (arterial blood gas) determination?