Clinical Examination - International Council of Ophthalmology
advertisement

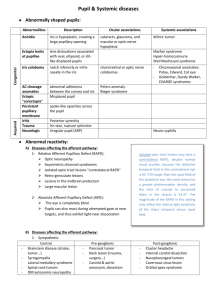
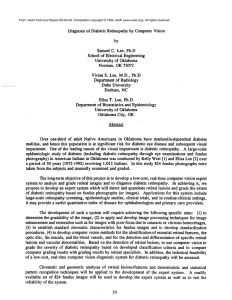
NEURO-OPHTHALMOLOGY Clinical Examination • • • • Visual Acuity Colour Vision Visual Fields Pupils Normal Eye and Optic Disc Cupped disc The swollen optic disc •Papilloedema •Papillitis •Malignant hypertension •Ischaemic optic neuropathy •Diabetic optic neuropathy •CRVO •Intraocular inflammation 25 y.o. female Reduced VA Pain with eye movement Colour desaturation RAPD 65 y.o. male Reduced VA Painless loss of vision Essential hypertension Smoker The pale optic disc •Congenital •Secondary to •raised ICP •vascular retinal disease •optic neuritis •optic nerve compression •trauma •Glaucoma Papilloedema • • • • • Disc swelling secondary to raised ICP Haemorrhages Headache – Worse in the morning – Valsalva manouver Nausea and projectile vomiting Horizontal diplopia (VI palsy) Causes Disc pallor – Space occupying lesion – Intracranial hypertension • Idiopathic • Drugs • Endocrine Vessel attenuation – Severe hypertension Blurred optic disc margin CWS Small optic cup Pupils • First Order – Retina to Pretectal Nucleus in B/S (at level of Superior colliculus) • Second Order – Pretectal nucleus to E/W nucleus (bilateral innervation!) • Third Order – E/W nucleus to Ciliary Ganglion • Fourth Order – Ciliary Ganglion to Sphincter pupillae (via short ciliary nerves) Pupil • Constricted (mioisis) – Sympathetic (pupillodilator) denervation – Drugs • Pilocarpine • Morphine • Dilated (mydriasis) – Parasympathetic (pupilloconstrictor) denervation – Lesion of the third CN – Drugs • Atropine • Cocaine Horner’s • Oculosympathetic paresis – – – – Ptosis Miosis Ipsilateral anhidrosis Does not dilate with cocaine 4% Sympathetic Pathway • First Order – Posterior Hypothalamus to Ciliospinal centre of Budge (C8-T2) (Uncrossed in Brainstem) • Second Order – Ciliospinal centre of Budge to Superior Cervical Ganaglion • Third Order – Superior Cervical Ganglion to dilator pupillae muscle. (Close to ICA and joins V1 intracranially) Internal Carotid Dissection Herpes Zoster Otitis Media Tolosa-Hunt Sy. CVA Tumour Pancoast bronchogenic carcinoma Causes of Horner’s pupil • Central – B/S lesions (tumours, vascular and MS) Syringomyelia, Lat. Med. Syn., S.C. ca. • Preganglionic – Pancoast tumour, Carotid & Aortic aneurysms, Neck lesions/trauma. • Postganglionic – Cluster headaches, Nasopharyngeal tumours, Otitis media, Cavernous sinus mass and ICA disease. • Miscellaneous – Congenital (brachial plexus injury) Idiopathic. Afferent & efferent defects • Argyll-Robertson pupil – Small, irreg – Does not react to light – Reacts to accommodation – Causes • syphilis • diabetes • Miotonic pupil (Adie’s syndrome) – Dilated – Poor response to light and convergence. • Constricts with weak Pilocarpine • Holmes-Adie syndrome – Reduced tendon reflexes (Knee, ankle) - Orthostatic hypotension Ocular motility abnormalities • Third nerve palsy – – – – Double vision Eye turned down & out Ptosis Dilated pupil & headache • Compressive lesion • Sixth nerve palsy – Double vision – Eye turned in Cranial Nerve Palsies Looking straight ahead Posterior communicating artery aneurysm Chiasma Posterior cerebral artery III CN Internuclear Ophthalmoplegia • Defective adduction of the ipsilateral eye • Nystagmus of the contralateral (abducting) eye • NORMAL CONVERGENCE • Causes – Young patients • Bilateral • Demyelination – Older patients • Unilateral • Vascular, tumours Myasthenia Gravis • • • • • Fatigability Double vision Lid twitch Ptosis Normal reflexes & sensation INVESTIGATIONS MG ACh Anti AChR Ab’s AChR • Anti ACh receptor Ab’s • Electromyography • Tensilon test – Edrophonium blocks acetyl-cholinesterase – Beware of cholinergic cardiac effects. Use with Atropine 0.6mg • Thoracic CT and MRI to rule out thymoma Localising the lesion • Monocular visual field defects indicate lesions anterior to the optic chiasm • Bitemporal defects are the hallmark of chiasmal lesions • Binocular homonymous hemianopia result from lesions in the contralateral postchiasmal region • Binocular quadrantanopias reflect optic tract lesions