acute lung injury and ARDS
advertisement

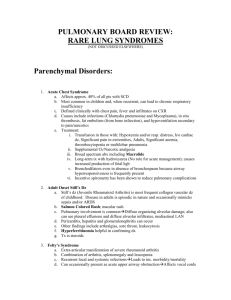
PULMONARY COMPLICATIONS PULMONARY COMPLICATIONS • Occur in up to 15% of general anaesthetic and major surgery and include: – Atelectasis – Pneumonia – Pulmonary Edema, Acute Lung Injury, and Adult Respiratory Distress Syndrome – Pulmonary Embolism and Venous Thromboembolism Atelectasis (alveolar collapse): Caused – airways obstructed, usually by bronchial secretions. – anesthetic, abdominal incision, and postoperative narcotics, Risk ― heavy smokers, obese, and have pulmonary secretions Symptoms – slow recovery from operations, poor colour, mild tachypnea, tachycardia and low-grade fever – the alveoli in the periphery collapse and a pulmonary shunt may occur Prevention is by pre-and post-operative physiotherapy – pain control, take deep breaths In severe cases – positive pressure ventilation may be required Pneumonia requires antibiotics, physiotherapy. Aspiration pneumonitis: • Sterile inflammation of the lungs from inhaling gastric contents Symptoms • vomiting or regurgitation with rapid onset of breathlessness and wheezing. • Non-starved patient undergoing emergency surgery is particularly at risk • May help avoid this by use of oral antacids or metoclopramide • Mortality is nearly 50% Pneumonia requires urgent treatment • bronchial suction, positive pressure ventilation, prophylactic antibiotics and IV steroids Prevention of aspiration • a period of no oral intake • usually 6 hours after a night meal • 4 hours after clear liquids • a longer period for diabetics Pulmonary Edema, Acute Lung Injury, and Adult Respiratory Distress Syndrome Etiology • A wide variety of injuries to the lungs or cardiovascular system, or both. • Three of the most common manifestations – pulmonary edema, acute lung injury, and ARDS Conditions Leading • Increased Hydrostatic Pressure • Altered Permeability State • Mixed or Incompletely Understood Pathogenesis Pulmonary Edema, Acute Lung Injury, and Adult Respiratory Distress Syndrome Conditions Leading Increased Hydrostatic Pressure Acute left ventricular failure Chronic congestive heart failure Obstruction of the left ventricular outflow tract Thoracic lymphatic insufficiency Volume overload Pulmonary Edema, Acute Lung Injury, and Adult Respiratory Distress Syndrome Conditions Leading (continued) Altered Permeability State Acute radiation pneumonitis Aspiration of gastric contents Drug overdose Near-drowning Pancreatitis Pneumonia Pulmonary embolus Shock states Systemic inflammatory response syndrome and multiple organ failure Sepsis Transfusion Trauma and burns Pulmonary Edema, Acute Lung Injury, and Adult Respiratory Distress Syndrome Conditions Leading (continued) Mixed or Incompletely Understood Pathogenesis Hanging injuries High-altitude pulmonary edema Narcotic overdose Neurogenic pulmonary edema Postextubation obstructive pulmonary edema Re-expansion pulmonary edema Tocolytic therapy Uremia Pulmonary Edema, Acute Lung Injury, and Adult Respiratory Distress Syndrome pulmonary edema often have a corresponding cardiac history or a recent history of massive fluid administration (or both). abnormal chest radiograph Management Requires intensive care with mechanical ventilation with positive-end pressure oxygen via facemask in mild cases intubation in more severe cases Pulmonary Edema, Acute Lung Injury, and Adult Respiratory Distress Syndrome acute lung injury and ARDS tachypnea, dyspnea, and increased work of breathing, as manifested by exaggerated use of the muscles of breathing. Cyanosis is associated with advanced hypoxia and is an emergency In patients with impending respiratory failure tachypnea, dyspnea, and air hunger Auscultation of the lung very poor breath sounds associated with crackles . Arterial blood gas presence of a low Pao2 and a high Paco2 Pulmonary Edema, Acute Lung Injury, and Adult Respiratory Distress Syndrome acute lung injury and ARDS Management initiated by immediate intubation plus careful administration of fluids and invasive monitoring with a Swan-Ganz catheter to assess wedge pressure and right-sided heart pressure. Pulmonary Edema, Acute Lung Injury, and Adult Respiratory Distress Syndrome acute lung injury and ARDS Management maintaining the patient on the ventilator with assisted breathing while healing of the injured lung takes place severe acute lung injury or ARDS is initially placed on an Fio2 of 100% and then weaned to 60% as healing takes place. Pulmonary Edema, Acute Lung Injury, and Adult Respiratory Distress Syndrome acute lung injury and ARDS Pulmonary Embolism and Venous Thromboembolism • serious postoperative complication • DVT is very commonly related to grade of surgery. • Many cases are silent – present as swelling of leg, tenderness of calf muscle and increased warmth • Diagnosis – venography or Doppler ultrasound. Pulmonary Embolism and Venous Thromboembolism Risk Factors for Venous Thromboembolism CATEGORY FACTORS General factors Advancing age Hospitalization or nursing home (with or without surgery) Neurologic disease (plegia and paresis) Cardiomyopathy, myocardial infarction, or heart failure secondary to valve disease Acute pulmonary disease (adult respiratory distress syndrome and pneumonia) Chronic obstructive lung disease Varicose veins Pulmonary Embolism and Venous Thromboembolism Risk Factors for Venous Thromboembolism CATEGORY FACTORS Inherited thrombophilia Protein C,S deficiency Antithrombin III deficiency Dysfibrinogenemia Factor V Leiden mutation Prothrombin gene mutation Anticardiolipin antibody Paroxysmal nocturnal hemoglobinemia Pulmonary Embolism and Venous Thromboembolism Risk Factors for Venous Thromboembolism CATEGORY FACTORS Acquired thrombophilia Malignancy Inflammatory bowel disease Heparin-induced thrombocytopenia Trauma Major surgery Nephrotic syndrome Systemic lupus erythematosus Pregnancy/postpartum History of venous thromboembolism Pulmonary Embolism and Venous Thromboembolism Pulmonary embolism Pulmonary Embolism and Venous Thromboembolism Pulmonary embolism • Diagnosis – ventilation/perfusion scanning and/or pulmonary angiography or dynamic CT • Management – intravenous heparin or subcutaneous low molecular weight heparin (LMWH),oral warfarin. – goal of reaching an INR of 2.5. ENDOCRINE COMPLICATIONS ENDOCRINE COMPLICATIONS • • • • Adrenal Insufficiency Hyperthyroid Crisis Hypothyroidism Syndrome of Inappropriate Antidiuretic Hormone Secretion Adrenal Insufficiency Chronic adrenal insufficiency Etiology • Adrenal insufficiency is an uncommon but potentially lethal condition associated with failure of the adrenal glands to produce adequate glucocorticoids 1. Primary adrenal insufficiency – most frequently due to autoimmune adrenalitis (Addison's disease), in which the adrenal cortex is destroyed by cytotoxic lymphocytes. 2. Secondary adrenal insufficiency – most commonly caused by long-term administration of pharmacologic doses of glucocorticoids. – Chronic use of glucocorticoids causes suppression of the hypothalamic-pituitary-adrenal axis (HPA), induces adrenal atrophy, and results in isolated adrenal insufficienc Adrenal Insufficiency Acute adrenal insufficiency Etiology • a result of abrupt cessation of pharmacologic doses of chronic glucocorticoid therapy, • surgical excision or destruction of the adrenal gland (adrenal hemorrhage, necrosis, or thrombosis in patients with sepsis or antiphospholipid syndrome), • surgical excision or destruction (postpartum necrosis) of the pituitary gland. Adrenal Insufficiency Symptoms and signs fatigue, weakness, anorexia, weight loss, orthostatic dizziness, abdominal pain, diarrhea, depression, hyponatremia, hypoglycemia, eosinophilia, decreased libido and potency. Patients with primary hypoadrenalism elevated plasma levels of corticotropin (hyperpigmentation of the skin and mucous membrane). Patients with secondary disease in contrast, initially have neurologic or ophthalmologic symptoms (headaches, visual disturbances) before showing signs of HPA axis disease (hypopituitarism). Adrenal Insufficiency Adrenal Insufficiency Treatment detailed instruction of patients receiving chronic corticosteroid therapy Adequate perioperative corticosteroid administration. In the critically ill a high index of suspicion can prevent a fatal outcome. A stress dose of hydrocortisone (100 mg) may be given with induction of anesthesia. For minor surgical procedures, usual maintenance dose is continued postoperatively. For major surgical procedures, a stress dose (100 mg) is continued every 8 hours until stable or free of complications and then tapered to the usual maintenance dose. Adrenal Insufficiency Hyperthyroid Crisis Etiology • Thyroid crisis is a medical emergency that occurs in thyrotoxic patients with toxic adenoma or toxic multinodular goiter • most often in patients with Grave's disease. • The crisis is frequently precipitated by a stressful event and characterized by exacerbation of hyperthyroidism and decompensation of one or more organ systems. • Mortality is high, ranging from 20% to 50% if the crisis is unrecognized and left untreated. Hyperthyroid Crisis Clinical manifestations of hyperthyroidism – nervousness, fatigue, palpitations, heat intolerance, weight loss, atrial fibrillation (in the elderly), – ophthalmopathy characterized • eyelid retraction or lag, periorbital edema, and proptosis. – The onset of thyroid crisis is sudden and characterized by accentuation of the symptoms and signs of thyrotoxicosis and organ system dysfunction • hyperpyrexia, tachycardia, dehydration , central nervous system dysfunction (delirium, psychosis, seizure, coma), cardiac manifestations, GI symptoms, and liver dysfunction. Hyperthyroid Crisis diagnosis of thyrotoxicosis • elevated levels of circulating thyroid hormone and suppressed thyroid-stimulating hormone (TSH) levels Hyperthyroid Crisis • elevated levels of circulating thyroid hormone and suppressed thyroid-stimulating hormone (TSH) levels • Treatment hypothyroidism Etiology • Hypothyroidism is characterized by low systemic levels of thyroid hormone and may be exacerbated in the postoperative period in patients with preexisting chronic hypothyroidism or as a result of severe stress. • Severe illness, physiologic stress, and drugs may inhibit peripheral conversion of T4 to T3 and induce a hypothyroid-like state. • Hypothyroidism may be primary (surgical removal, ablation, or disease of the thyroid gland), secondary (hypopituitarism), or tertiary (hypothalamic disease). hypothyroidism Presentation and Diagnosis • Patients with chronic hypothyroidism may be asymptomatic or rarely have the severe form (myxedema coma) characterized – coma, loss of deep tendon reflexes, cardiopulmonary collapse – high (∼40%-50%) mortality. • The majority, demonstrate – cold intolerance, constipation, brittle hair, dry skin, sluggishness, weight gain, and fatigue. • The impact of hypothyroidism cardiovascular system – bradycardia, hypotension, impaired cardiac function, conduction abnormalities, pericardial effusion, and increased risk for CAD. • In the critically ill (trauma, sepsis)pulmonary function – a predisposition to pleural effusion, and susceptibility to hypothermia. hypothyroidism Presentation and Diagnosis • The ECG usually shows bradycardia, low voltage, and prolonged PR, QRS, and QT intervals. primary hypothyroidism – serum total T4, free T4, and free T3 levels are low, whereas TSH is elevated. secondary hypothyroidism • TSH, the free T4 index, and free T3 are low. hypothyroidism Treatment • Patients with known hypothyroidism who are receiving replacement hormonal therapy and are in the euthyroid state – do not require any special treatment before surgery but are instructed to continue taking their medications. • In patients with symptomatic chronic hypothyroidism – surgery is postponed until a euthyroid state is achieved. • Patients with myxedema coma or those showing clinical signs of significant hypothyroidism (severe postoperative hypothermia, hypotension, hypoventilation, psychosis, and obtundation) – immediately treated with thyroid hormone, concomitant with the IV administration of hydrocortisone, to avoid an addisonian crisis. IV levothyroxine or triiodothyronine may be given until oral intake is possible. Syndrome of Inappropriate Antidiuretic Hormone Secretion Etiology – The syndrome of inappropriate antidiuretic hormone secretion (SIADH) is the most common cause of chronic normovolemic hyponatremia. – Hyponatremia is defined as a serum sodium concentration of less than 135 mmol/L – hyponatremia despite all attempts to correct the imbalance in the presence antidiuretic activity from elevated arginine vasopressin Syndrome of Inappropriate Antidiuretic Hormone Secretion Etiology – Disorders and conditions that predispose to this relatively rare condition • trauma, stroke, antidiuretic hormone–producing tumors, drugs (ACE inhibitors, dopamine, NSAIDs), and pulmonary conditions. Syndrome of Inappropriate Antidiuretic Hormone Secretion Clinical characteristics • anorexia, nausea, vomiting, obtundation, and lethargy. With more rapid onset, seizures, coma, and death can result. The cardinal criteria of SIADH include – hyponatremia – hypotonicity of plasma, – urine osmolality in excess of plasma osmolality, increased renal sodium excretion – absence of edema or volume depletion – normal renal function. Syndrome of Inappropriate Antidiuretic Hormone Secretion Treatment • Management of SIADH includes treatment of the underlying disease process and removal of excess water (i.e., treatment of the hyponatremia). • Fluid restriction is the mainstay of management of chronic SIADH. • IV administration of normal saline is used only in significantly. • Diuretics such as furosemide occasionally help correct the imbalance. • In some cases, IV administration of 3% saline solution may be required, but correction must be done in a constant, sustained fashion because overly rapid correction can result in seizure activity.